Introduction
Plasma cell granuloma is a rare entity describing a
non-neoplastic lesion featuring histological proliferation of
polyclonal plasma cells, lymphocytes, neutrophils, eosinophils and
histiocytes in a fibrotic background (1). While this mass lesion is reported to
occur in nearly every organ in the body, plasma cell granulomas
most frequently present in the lungs. The underlying cause and
natural history of these lesions remains unknown and treatment
options include excision, radiation and steroids (2). The current case report presents the
longest known follow-up period in the literature for an
intracranial plasma cell granuloma. In addition, the course of the
patient’s disease following multimodal therapy, including surgery,
radiation and steroids, is detailed. The study was approved by the
Wake Forest University School of Medicine Institutional Review
Board (Winston-Salem, NC, USA). Written informed consent was
obtained from the patient’s family.
Case report
Patient characteristics
A 55-year-old Caucasian female with a history of
hypertension, chronic otitis and mastoiditis presented to an
outside institution with a three-week history of bitemporal frontal
headaches and left-sided hearing loss. On examination, the patient
was awake and alert but was noted to have difficulty with speech.
Bilateral papilledema was identified by fundoscopy. The remainder
of the exam was nonfocal and without further neurological deficits.
A computed tomography with contrast revealed a 5×5-cm
heterogeneously enhancing mass in the left temporal lobe with a
large amount of associated left hemisphere edema and left-to-right
shift. The patient underwent surgery for further management.
Pathological analysis
Pathological analysis of a subtotal resection
demonstrated perivascular and intraparenchymal collections of
lymphocytes and plasma cells set within a densely fibrotic
background. Neurons and reactive astrocytes were entrapped within
the inflammatory lesion. The lymphocytes and plasma cells appeared
small and mature with no histological evidence of lymphoma or
myeloma. There was no evidence of vasculitis or amyloid deposits on
the routine stains. Immunohistochemical studies revealed the
presence of κ (marginally predominant) and λ light chains,
confirming the polyclonal nature of the plasma cell infiltrate,
along with a mixed population of T and B cells, consistent with an
inflammatory process. Stains for microorganisms and Epstein-Barr
virus were negative.
Further work-up included a bone marrow biopsy, serum
electrophoreses (negative for monoclonal and polyclonal gammopathy)
and β-2 microglobulin, which were all within normal limits. A final
diagnosis of intracranial plasma cell granuloma was made.
Clinical course
The patient’s course was punctuated by several
recurrences over a 14-year follow-up period. The first recurrence
in the left temporal region was detected by surveillance magnetic
resonance imaging (MRI) at three years and treated with another
surgical resection and 3,600-cGy adjuvant radiation therapy
fractionated over four weeks. A second recurrence was again
detected by surveillance MRI at seven years and treated with a
third resection of a 3×5-cm mass. Pathology was again consistent
with recurrent plasma cell granuloma. One month later, the patient
presented to an ophthalmologist with decreasing vision in the left
eye. A small blind spot progressed to complete loss of vision out
of the left eye over the next eight months. Two months later, the
patient noted decreasing vision in the right eye and was referred
to Wake Forest University School of Medicine for further
management.
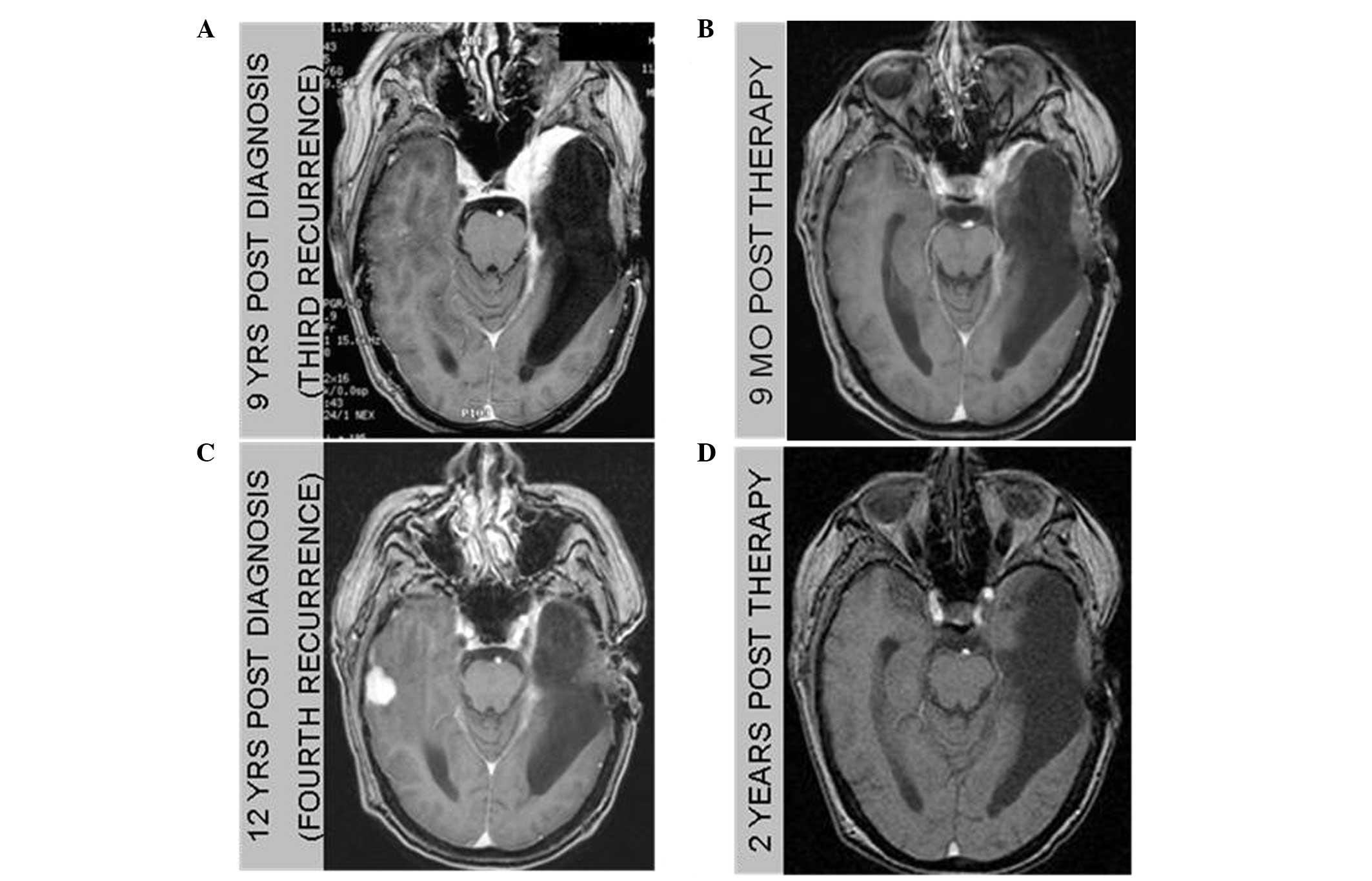
Now at nine-years post-diagnosis, work-up at our
facility, including MRI imaging and erythrocyte sedimentation rate
(ESR) measurement (Fig. 1A),
revealed a third recurrence constituted by a new area of
enhancement, somewhat anterior to the resection cavity in the
anterior temporal fossa, surrounding the orbital apex and involving
the left optic nerve along with an elevated ESR. The patient
refused additional surgical intervention and was not considered to
be a candidate for additional radiation therapy. The treatment plan
consisted of 4 mg dexamethasone four times a day, which was
steadily reduced over two months due to a steroid-induced myopathy
and psychosis. Despite persistent visual loss, a six-month
post-steroid MRI study demonstrated a reduction in size of the
lesion, constituting a partial response, accompanied by a decrease
in the ESR from an initial value of 56 to 10 mm/h. This apparent
response prompted treatment with oral prednisone at a dose of 10 mg
every other day that was well tolerated and without side effects. A
repeat MRI three months later revealed resolution of the mass
(Fig. 1B). The sedimentation rate
remained low at 11 mm/h. Steroids were tapered over the subsequent
two months.
Twelve-years following the initial diagnosis and 1.5
years after steroid treatment, a surveillance MRI demonstrated a
new contralateral peripherally enhancing mass surrounded by
vasogenic edema in the right temporal lobe (Fig. 1C). Of note, surveillance imaging
noted opacification of the right mastoid air cells six months prior
to the occurrence of this lesion representing a potential
infectious etiology seeding eventual granuloma formation. This
fourth recurrence was treated with 80 mg oral prednisone daily.
Following two months of therapy, the patient had a partial response
with a decline in the size of the lesion by 50%. Prednisone was
tapered and eventually discontinued over the next five months. The
ESR was 42 mm/h during this recurrence and remained elevated.
Fourteen years following the initial diagnosis and
two years following the patient’s latest course of prednisone, a
repeat brain MRI revealed a near complete response (Fig. 1D). The sedimentation rate was 10
mm/h (Fig. 2). Several months
later, at 69 years-old, the patient unexpectedly succumbed to a
probable myocardial infarction, arrhythmia or pulmonary embolus at
home, following complaint of substernal chest pain. The patient did
not undergo an autopsy.
Discussion
The number of reported intracranial cases of plasma
cell granuloma reviewed in the literature is ~50 (2–5). The
paucity of long-term follow-up cases may result in an incomplete
understanding of the natural history and recurrence management of
this rare disease. In the present study, the patient was followed
until death, fourteen years following the initial diagnosis.
Furthermore, the individual suffered four disease recurrences,
adding to the eight reported cases of relapsing intra-axial plasma
cell granuloma (3). Treatment of
the recurrences consisted of two craniotomies, 3,600-cGy
fractionated radiation and two courses of glucocorticoid
therapy.
Histopathological analysis remains the gold standard
for achieving the diagnosis of plasma cell granuloma. Tissue
sections in the present patient contained a perivascular infiltrate
of lymphocytes and polyclonal plasma cells, which is characteristic
of plasma cell granulomas (3,6,7). A
slight predominance of κ as compared to λ light chains was noted,
and this has also been found in other cases of plasma cell
granuloma. Given the inflammatory nature of these lesions, the
diagnostic work-up includes a search for microorganisms or a
systemic inflammatory condition. The current patient’s history of
chronic mastoiditis and otitis on the same side of the lesion
raises suspicion of the possibility of undetected organisms.
Monitoring for response to therapy and recurrences
traditionally relies on clinical exam and surveillance imaging. To
the best of our knowledge, this case represents the first time ESR
has been reported to rise and fall in concert with disease
recurrence, presence and resolution. Rising ESR values appeared to
be specific to the disease and were not the result of surgical
intervention, as these recurrences were treated with steroids.
Further, the decline in the ESR appeared to be specific to disease
activity rather than the result of a systemic immune suppression,
as the values correlated with imaging changes. The literature
reports elevation of inflammatory markers, ESR and CRP, in patients
with plasma cell granulomas; however, the marker levels were
analyzed at diagnosis and not serially followed, with only one case
series describing a decrease in ESR following surgical management
of pulmonary plasma cell granulomas (8–10).
Trending ESR may complement imaging with regard to disease
activity, treatment response or impending radiographical
recurrence.
This unique case of a plasma cell granuloma was
treated for four recurrences over the course of 14 years. Each
treatment resulted in a complete, lengthy, but unsustained
response. Relapses and responses of the disease were detected by
imaging and ESR, which may prove supplemental to imaging studies
for evaluating disease activity.
References
|
1
|
Bahadori M and Liebow AA: Plasma cell
granulomas of the lung. Cancer. 31:191–208. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Buccoliero AM, Caldarella A, Santucci M,
Ammannati F, Mennonna P, Taddei A, et al: Plasma cell granuloma -
an enigmatic lesion: description of an extensive intracranial case
and review of the literature. Arch Pathol Lab Med. 127:e220–e223.
2003.PubMed/NCBI
|
|
3
|
Puntambekar P, Santhakumar S, Kupsky WJ,
Tselis A and Mittal S: Primary intracranial plasma cell granulomas
presenting as malignant neoplasms. J Neurooncol. 106:327–337. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kilinç M, Ertürk IO, Uysal H, Birler K,
Evrenkaya T and Akkalyoncu BB: Multiple plasma cell granuloma of
the central nervous system: a unique case with brain and spinal
cord involvement. Case report and review of literature. Spinal
Cord. 40:203–206. 2002.PubMed/NCBI
|
|
5
|
Makino K, Murakami M, Kitano I and Ushio
Y: Primary intracranial plasma-cell granuloma: a case report and
review of the literature. Surg Neurol. 43:374–378. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Coffin CM, Watterson J, Priest JR and
Dehner LP: Extrapulmonary inflammatory myofibroblastic tumor
(inflammatory pseudotumor). A clinicopathologic and
immunohistochemical study of 84 cases. Am J Surg Pathol.
19:859–872. 1995. View Article : Google Scholar
|
|
7
|
Häusler M, Schaade L, Ramaekers VT,
Doenges M, Heimann G and Sellhaus B: Inflammatory pseudotumors of
the central nervous system: report of 3 cases and a literature
review. Hum Pathol. 34:253–262. 2003.PubMed/NCBI
|
|
8
|
Nonomura A, Mizukami Y, Matsubara F,
Shimizu J, Oda M, Watanabe Y, et al: Seven patients with plasma
cell granuloma (inflammatory pseudotumor) of the lung, including
two with intrabronchial growth: an immunohistochemical and electron
microscopic study. Intern Med. 31:756–765. 1992. View Article : Google Scholar
|
|
9
|
Breidahl WH, Robbins PD, Ives FJ and Wong
G: Intracranial plasma cell granuloma. Neuroradiology. 38(Suppl 1):
S86–S89. 1996. View Article : Google Scholar
|
|
10
|
Monzon CM, Gilchrist GS, Burgert EO Jr,
O’Connell EJ, Telander RL, Hoffman AD and Li CY: Plasma cell
granuloma of the lung in children. Pediatrics. 70:268–274.
1982.PubMed/NCBI
|