Introduction
Although the incidence and mortality of gastric
cancer (GC) have markedly decreased worldwide over the last 50
years, it remains the world’s second leading cause of tumor-related
mortality (1). Despite advances in
diagnosis and treatment, the majority of patients with advanced GC
will succumb to the disease, due to local tumor invasion and
distant metastasis (2). Tumor
metastasis is a multistep process and is regulated by a number of
growth factors and cellular signaling pathways (3,4).
Fascin is an actin-bundling protein that is important for the
maintenance and stability of filamentous actin bundles, and is
consequently involved in cell motility (5). Fascin expression is low or absent in
the majority of normal adult epithelia and often upregulated in
various types of tumor, for example breast, prostate and brain
tumors, bladder cancer and esophageal squamous carcinoma (6,7). Tumor
cells with high expression of fascin have been found to exhibit
increased membrane protrusions and migration ability (6,7),
suggesting that fascin is associated with clinical aggressiveness
and metastasis. However, the mechanism by which fascin expression
is upregulated in tumors is not understood. Although the prognostic
relevance of fascin expression has been reported in human GC
(8), the present study aimed to
investigate the relationship between fascin expression and cell
migration and invasion in GC cells. Through this, is was hoped to
further elucidate the underlying molecular mechanisms.
Signal transducer and activator of transcription 3
(STAT3) is a well-known transcription factor and regulates a
variety of cellular processes, including cell proliferation and
survival, oncogenesis and cancer metastasis in GC. Dysregulation of
STAT3 signaling is a frequent cause of gastric carcinogenesis
(9–11). Interleukin-6 (IL-6), a member of the
glycoprotein 130 family of cytokines, can induce activation of
STAT3 signaling pathways to affect downstream signaling and
cellular events (12,13). Furthermore, study results suggest
that IL-6 promotes GC metastasis through activation of STAT3
(9,11) and that inhibition of STAT3 blocks
angiogenesis and metastasis of GC (14). However, the mechanism by which
IL-6-induced STAT3 activation promotes GC metastasis is not well
defined. Additionally, IL-6 promotes cell invasion by upregulating
fascin expression in glioblastoma cells (15), suggesting a possible correlation
between STAT3 activation and fascin expression. However, whether
STAT3 induces fascin expression in GC is currently unknown, and the
roles of fascin in the malignant behavior of GC remain unclear.
Materials and methods
Cell culture
Five human gastric carcinoma cell lines, MKN45,
MKN28, BGC823, AGS and SGC7901, were cultured in RPMI-1640 medium
(Invitrogen Life Technologies, Carlsbad, CA, USA) supplemented with
10% fetal bovine saline (FBS). MKN45 cells were subsequently
treated with various concentrations of recombinant human IL-6
(R&D Systems, Minneapolis, MN, USA) for the indicated durations
in their respective starvation mediums. A human gastric epithelial
cell line, GES-1, was cultured in Dulbecco’s modified Eagle medium
(Invitrogen Life Technologies) supplemented with 10% FBS.
Reagents
Janus kinase 2 (JAK2) inhibitor (AG490) and
γ-secretase inhibitor (DAPT) were purchased from Calbiochem (La
Jolla, CA, USA). Dimethyl sulfoxide (DMSO) and DAPI were purchased
from Sigma-Aldrich (St. Louis, MO, USA). Antibodies used for
western blotting and chromatin immunoprecipitation (ChIP) assays
were anti-phosphotyrosine (p)STAT3 (Cell Signaling Technology,
Inc., Beverly, MA, USA), anti-STAT3 (Cell Signaling Technology,
Inc.), anti-nuclear factor (NF)-κB p50 (Santa Cruz Biotechnology,
Inc., Santa Cruz, CA, USA), anti-fascin (Abcam, Cambridge, UK),
anti-hairy and enhancer of split-1 (Hes-1; Abcam),
anti-activated-Notch1 (Abcam), anti-activated-Notch2 (Abcam),
anti-matrix metalloproteinase (MMP)-2 and anti-MMP-9 (Cell
Signaling Technology, Inc.), anti-GAPDH (Abcam), anti-rabbit
immunoglobulin (Ig)G and horseradish peroxidase-linked antibody
(Cell Signaling Technology, Inc.).
ChIP assays
ChIP assays were performed using a ChIP assay kit,
according to the manufacturer’s instructions (Upstate
Biotechnology, Lake Placid, NY, USA) as described previously
(16,17). Briefly, cells were treated as
indicated and cross-linked with formaldehyde and sonication.
Resulting cell lysates (input) were immunoprecipitated with 2.5 μg
STAT3 antibody, NF-κB p50 or normal rabbit IgG. The precipitated
protein-DNA complexes (IP) were subjected to proteinase treatment.
The primers used to confirm the binding of factors to the promoter
region of fascin had the following sequence: were
5′-accttgtgggcagcctgt-3′ and 5′-attccctgcagacaccacct-3′.
Reverse transcription and quantitative
(q)PCR
Reverse transcription and qPCR were performed as
described previously (16–18). RNA was extracted with TRIzol reagent
(Invitrogen Life Technologies) and concentrations of RNA were
quantified by NanoDrop 1000 (NanoDrop, Wilmington, DE, USA).
Reverse transcription was performed using the Reverse Transcription
System (Promega GmbH, Madison, WI, USA) to obtain cDNA, which was
subjected to qPCR using SYBR® Premix Ex Taq™
(Takara Bio, Inc., Shiga, Japan) on a StepOne™ Real-Time PCR System
(Applied Biosystems, Carlsbad, CA, USA). qPCR primers: Human
fascin, 5′-aaaagtgtgccttccgtacc-3′ and 5′-cccattcttcttggaggtca-3′;
GAPDH, 5′-atcaagaaggtggtgaagca-3′ and
5′-gtcgctgttgaagtcagagga-3′.
Western blotting
Cell protein concentrations were quantitated using a
Bio-Rad assay (Bio-Rad, Hercules, CA, USA). Proteins were resolved
by 10% SDS-PAGE and transferred to a polyvinylidene fluoride
membrane (Millipore, Billerica, MA, USA). The membrane was probed
sequentially with the antibodies. Anti-fascin,
anti-activated-Notch1, anti-activated-Notch2, anti-Hes-1,
anti-STAT3, anti-pSTAT3, anti-MMP-2 and -9, anti-NF-κB p50 and
anti-GAPDH antibodies were used. Blots were developed using
chemiluminescence with the LAS-4000 Imaging system (Fujifilm,
Tokyo, Japan).
RNA interference (RNAi)
RNAi was performed using small interfering RNA
(siRNA) against target genes, as described previously (16–18).
RNAi was performed using human STAT3 siRNA oligonucleotides from
Qiagen (Hilden, Germany) and a negative control siRNA. NF-κB siRNA
was from Qiagen and cells were transfected using HiPerFect
transfection reagent (Qiagen).
In vitro scratch wound healing assay
Cells were allowed to grow to confluence and
cultured in serum-free medium for 12 h, prior to scratching with a
sterile pipette tip. Cells were washed twice with growth medium to
remove cell debris. Next, the culture medium was replaced with
growth medium with 5% FBS to minimize cell proliferation. Wound
areas were photographed and analyzed using the IPP 6.0 system
(Intel, Santa Clara, CA, USA) at a magnification of ×100.
Cell migration and invasion assays
Cell migration was assessed using Transwell
Permeable Supports (Corning Inc., Corning, NY, USA). Briefly, cells
were allowed to grow to confluence. In total, 5×104
cells/well were resuspended in 100 μl serum-free medium and plated
onto uncoated 8-μm transwell filter inserts of 24-well plates in
triplicate. The lower chambers contained 600 μl medium containing
15% FBS as a chemoattractant. Nonmigratory cells in the upper
chamber were removed with a cotton swab following incubation for 16
h. Cells on the bottom side were fixed in 100% methanol and stained
with 0.5 μg/ml DAPI for 5 min. Cells were counted using a
fluorescence microscope (Nikon Eclipse 80i; Nikon, Tokyo, Japan) in
five random fields. For evaluation of cell invasion, cells were
allowed to invade Matrigel-coated transwell filters. At the end of
the experiments, invaded cells on the bottom of the membrane were
incubated with 0.1% crystal violet solution and dissolved in 20%
acetic acid. Finally, 100 μl dye mixture was transferred to a
96-well plate for absorbance readings at 560 nm.
GC xenograft model
All animal experiments were approved by the
Institutional Animal Care and Use Committee of Taizhou University
(Taizhou, China) and the study was approved by Taizhou University
Ethics Committee. MKN45 cells (5×106 cells) were
injected subcutaneously into the flanks of 4-week-old female
athymic nude mice (Medical School Laboratory Animal Center,
Zhejiang University, Zhejiang, China). Tumors became palpable (at
~75 mm3) within a week following injection of tumor
cells and animals were randomly assigned to various treatment
groups (n=7 in each group). Nude mice were injected
intraperitoneally with AG490 alone (20 mg/kg). For single-agent
treatment, a vehicle was administered in place of AG490 with the
same schedule. Tumor size was calculated using the following
formula: (width2 × length)/2. At the end of the
experiment, tumors were resected from mice and the presence of
liver metastasis was determined by hematoxylin-eosin (HE)
staining.
Statistical analysis
All data were presented as the mean ± standard
deviation. Statistical significance was determined by Student’s
t-test for paired or unpaired data as appropriate. P<0.05 was
considered to indicate a statistically significant difference. All
analyses were performed using SPSS 16.0 (SPSS Inc., Chicago, IL,
USA).
Results
Fascin is directly regulated by STAT3 in
response to IL-6 in MKN45 cells
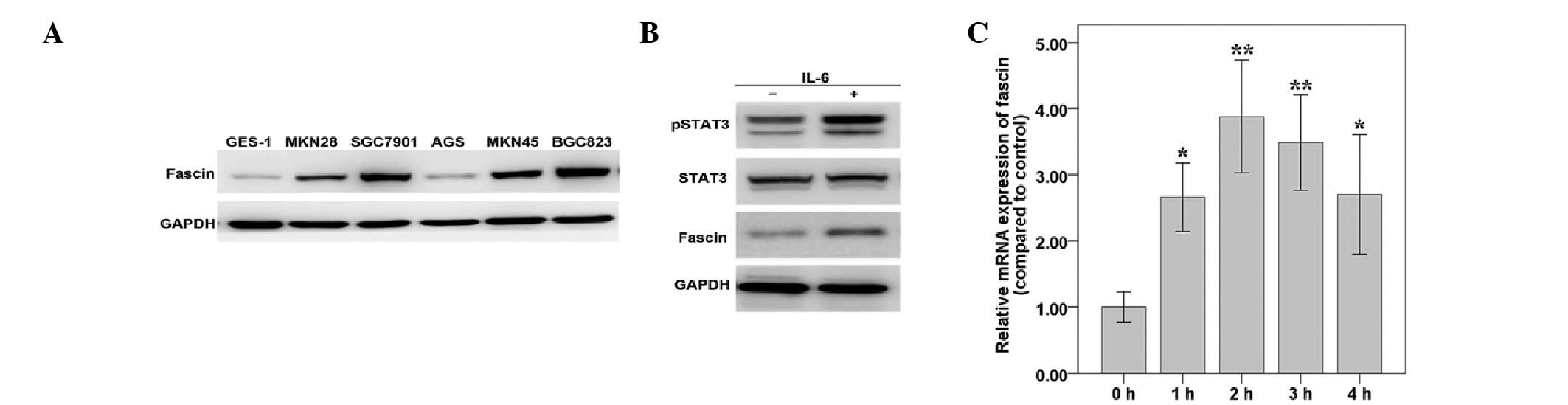
Fascin expression was determined in the GC cell
lines, MKN28, SGC7901, AGS, MKN45 and BGC823, and also in the
immortalized human gastric mucosal epithelial cell line, GES-1.
Fascin was highly expressed in the majority of GC cell lines
(Fig. 1A). Next, the relationship
between fascin expression and STAT3 activation in MKN45 cells was
analyzed, using IL-6 as a stimulating factor. Results showed that
IL-6 induced protein expression of tyrosine phosphorylated STAT3
and fascin, with no effect on total STAT3 protein levels (Fig. 1B). However, as with the typical
pattern of STAT3-target genes, fascin mRNA expression increased
rapidly following IL-6 treatment and peaked at ~3-fold, after 2 h
of treatment, but later decreased (Fig.
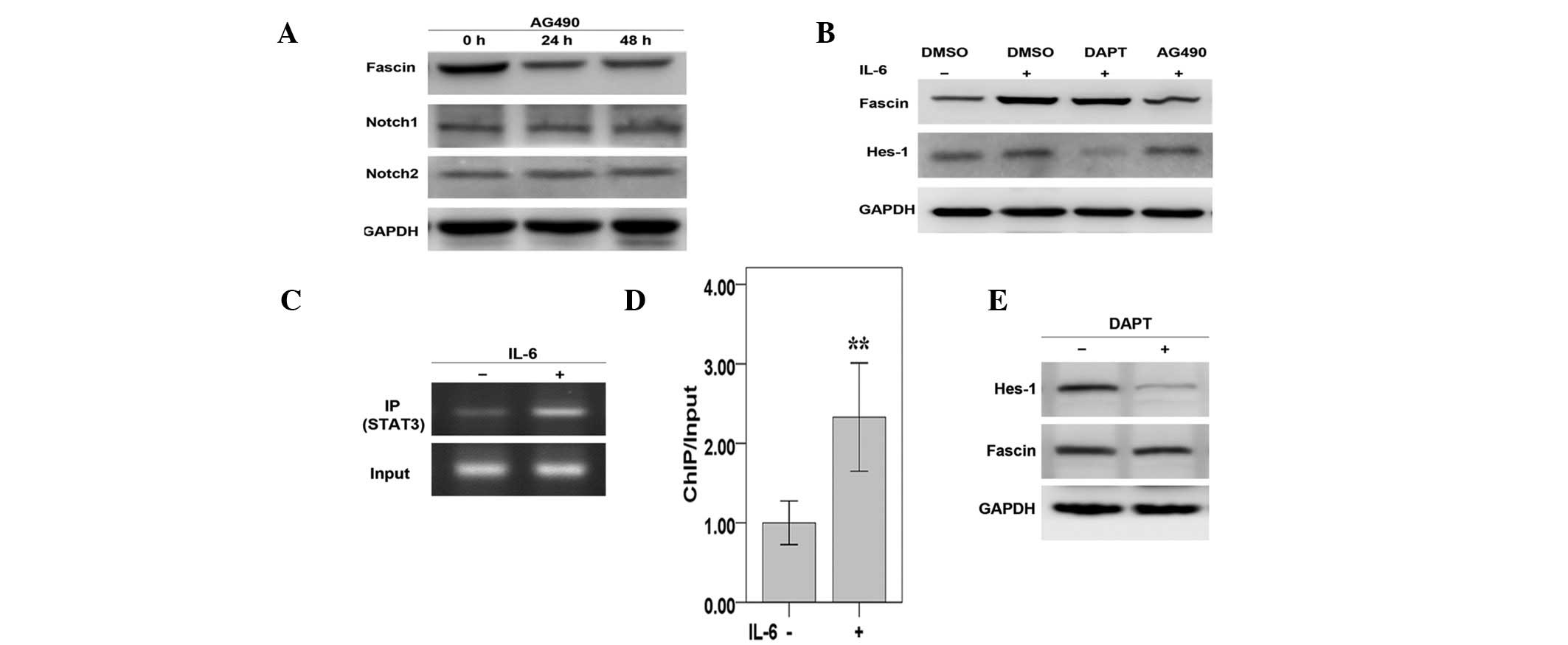
1C). Next, the AG490 JAK2/STAT3 inhibitor was used to inhibit
STAT3 activation. Results demonstrated that AG490 suppressed basal
and IL-6-induced fascin expression (Fig. 2A and B). Furthermore, ChIP assays
revealed that STAT3 directly bound to the fascin promoter. This
binding increased ~2.5-fold when treated with IL-6 (Fig. 2C and D). Collectively, these results
suggest that STAT3 regulates fascin transcription through direct
binding to the fascin promoter in MKN45 cells.
Notch signaling is not involved in fascin
upregulation in MKN45 cells
To investigate whether the endogenous Notch
signaling pathways are involved in promotion of fascin expression,
the DAPT Notch inhibitor was used. Results showed that DAPT
significantly inhibited expression of target gene Hes-1 but had no
significant effect on IL-6-induced fascin expression (Fig. 2B). Basal expression of fascin was
also not altered by DAPT (Fig. 2E).
Furthermore, AG490 had no significant effect on the constitutive
expression of Notch1 and Notch2 (Fig.
2A). These results suggest that Notch signaling pathways may
not be involved in the regulation of fascin expression.
STAT3 activation induced by IL-6 is
required for fascin expression and cell migration and invasion in
MKN45 cells
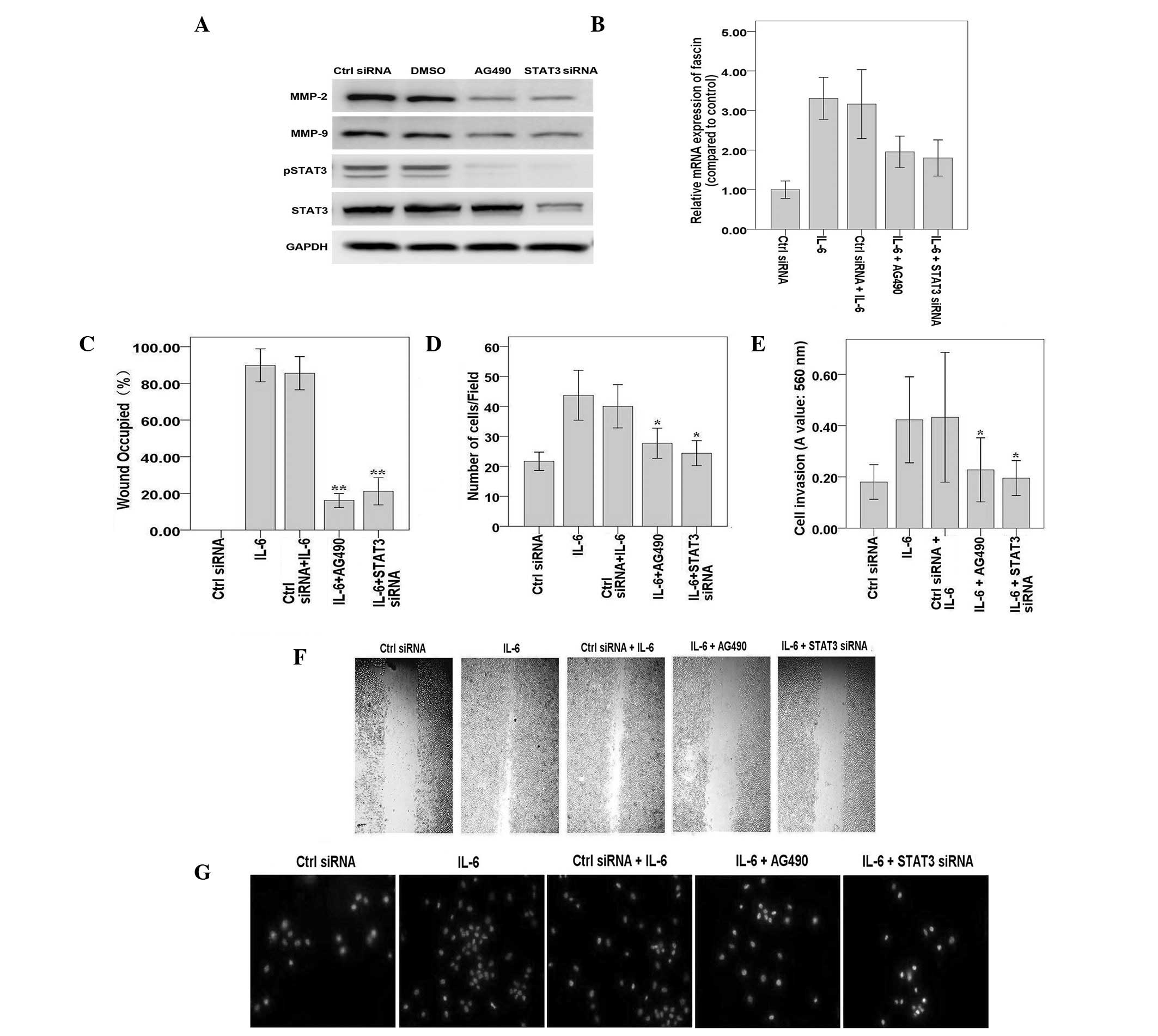
To further investigate whether STAT3 is required for
IL-6-induced fascin expression, STAT3 siRNA and AG490 were used.
Western blotting showed that STAT3 expression was significantly
downregulated by STAT3 siRNA and AG490 (Fig. 3A). qPCR demonstrated that
IL-6-induced elevated fascin mRNA levels were significantly
reversed by STAT3 siRNA transfection or AG490 treatment (Fig. 3B). These results confirm that STAT3
is required for fascin expression in MKN45 cells, in response to
IL-6. In addition, results of cell migration and invasion assays
showed that, compared with cells treated with IL-6 alone, cells
subjected to STAT3 siRNA transfection or AG490 incubation migrated
and invaded less efficiently (Fig.
3C–E). Representative results are shown in Fig. 3F and G. Consistent with this,
expression of MMP-2 and -9 significantly decreased when treated
with AG490 and STAT3 siRNA (Fig.
3A).
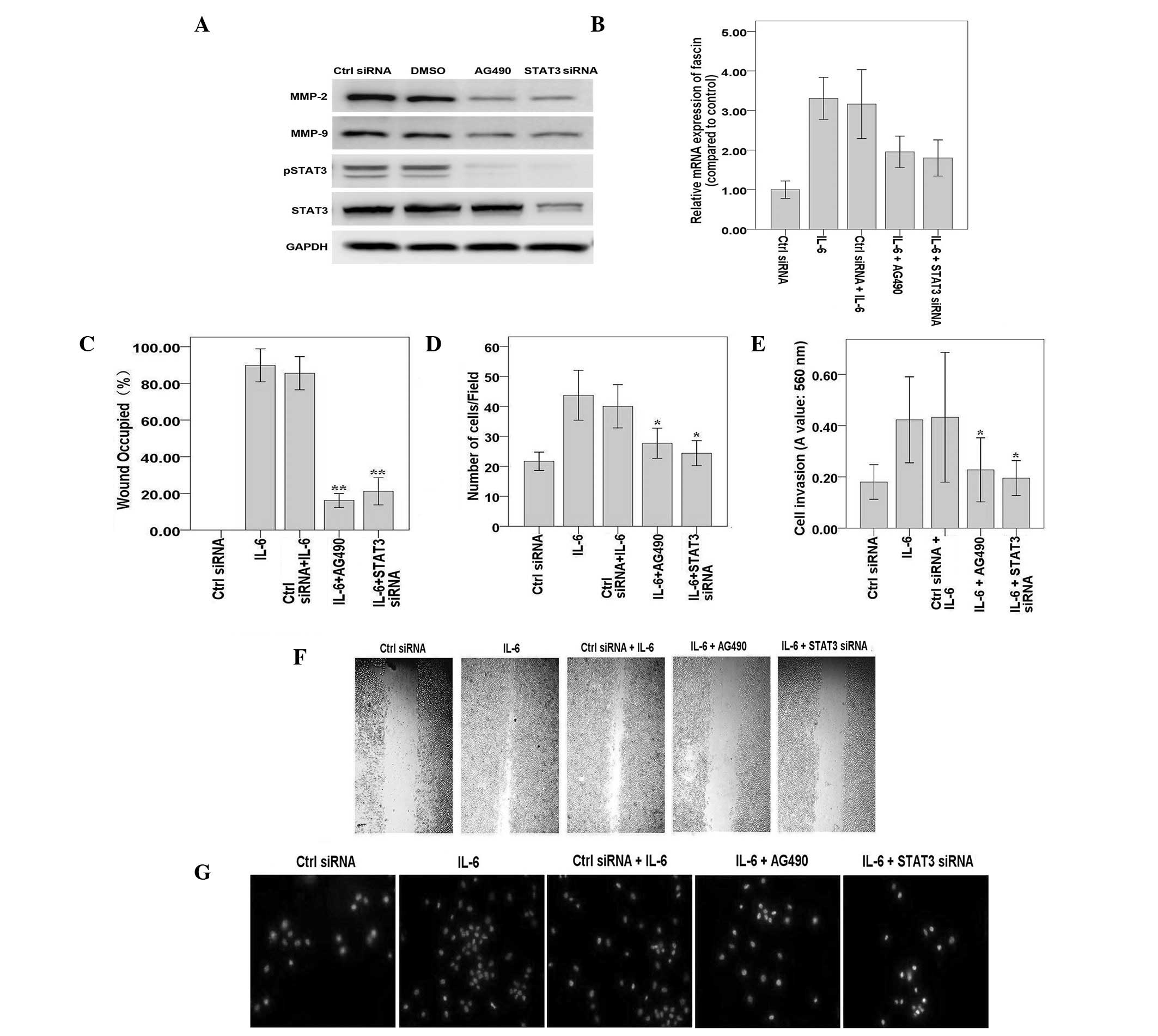 | Figure 3STAT3 is required for IL-6-induced
expression of fascin and cell migration in MKN45 cells. (A) MKN45
cells were transfected with STAT3 siRNA or treated with AG490 and
cultured for 24 h. Whole cell extracts were subjected to western
blotting with antibodies against pSTAT3, total STAT3, MMP-2 and -9
and GAPDH. MKN45 cells were treated with IL-6 for 30 min. (B) MKN45
cells were transfected with STAT3 siRNA or treated with AG490 and
cultured for 3 days prior to treatment with IL-6 for 30 min. mRNA
levels of fascin were detected by quantitative polymerase chain
reaction. Results were standardized to GAPDH and expressed as fold
induction of IL-6-treated cells from three independent experiments.
(C) MKN45 cells were treated as described and wound healing assays
were performed. The percentage of the wound occupied in three
independent experiments was calculated. (D) MKN45 cells were
treated as described and cell migration assays were performed. The
mean number of migrated cells in at least 5 visual fields of 3
independent experiments was calculated. (E) MKN45 cells were
treated as described and cell invasion assays were performed.
Invaded cells were stained and eluted for absorbance readings at
560 nm. (F) Representative experiments of wound healing assays are
shown (magnification, ×100). (G) Representative experiments of cell
migration assays are shown (magnification, ×100).
*P<0.05 and **P<0.01, vs. control. MMP,
matrix metalloproteinase; STAT3, signal transducer and activator of
transcription 3; pSTAT3, phosphotyrosine STAT3; DMSO, dimethyl
sulfoxide; IL-6, interleukin-6; siRNA, small interfering RNA. |
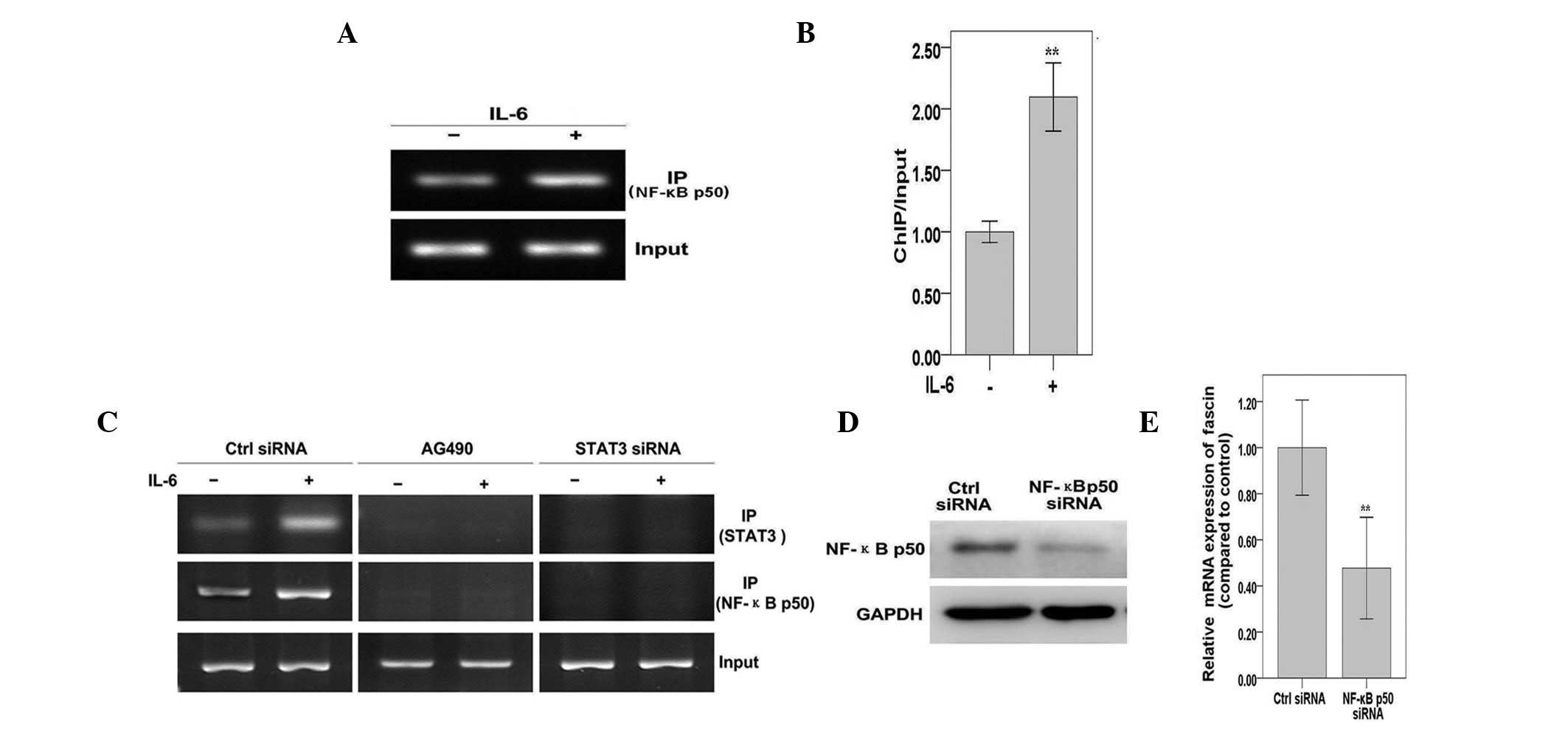
STAT3 is required for NF-κB recruitment
to the fascin promoter in response to IL-6 in MKN45 cells
To investigate the possible cross-talk mechanisms
between the STAT3 and NF-κB pathways, in response to IL-6 treatment
in MKN45 cells, ChIP assays were performed. A significant increase
in NF-κB p50 bound to the fascin promoter was found when cells were
treated with IL-6 (Fig. 4A and B).
However, in STAT3 siRNA-transfected cells and AG490-treated cells,
there was weak or no STAT3 and NF-κB p50 binding to the fascin
promoter in response to IL-6 treatment (Fig. 4C). This indicates that NF-κB p50
binds to the fascin promoter in a STAT3-dependent manner. In
addition, NF-κB p50 silencing resulted in reduced fascin mRNA
expression (Fig. 4D and E).
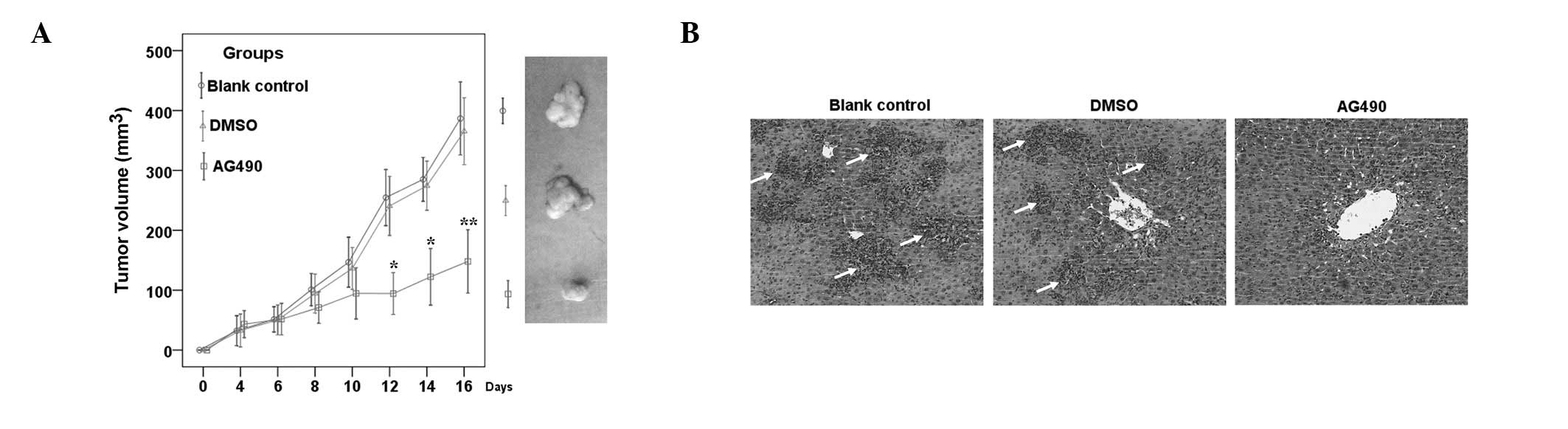
STAT3 inhibition suppresses in vivo
growth and metastasis of GC cells
To determine the role of STAT3 in tumor growth and
metastasis in animals, MKN45-xenografts were established in
BALB/c-nu mice. It was found that STAT3 inhibition by AG490
significantly inhibited tumor growth, compared with DMSO-treated or
untreated controls (Fig. 5A). HE
staining of liver tissue revealed that STAT3 inhibition caused a
reduction in liver metastasis [28.57% (2/7)] compared with the
control group [85.71% (6/7)] (Fig.
5B).
Discussion
Previous data have suggested that fascin expression
is abnormally high in a number of metastatic cancers, and commonly
correlates with the aggressive behavior of tumor cells (6,19). In
human GC, fascin expression significantly correlates with serosal
invasion, histopathological grading, lymph node metastasis,
tumor-node-metastasis stage and recurrence (8,20).
However, to the best of our knowledge, the present study is the
first to investigate the underlying cellular and molecular
mechanisms of fascin expression in GC. Local invasion and lymphatic
metastasis are frequent events in human GC and are associated with
various cytokines, including IL-6 (21). JAK2/STAT3 is one of the major
signaling pathways triggered by IL-6 and is constitutively
activated in numerous cancer cell lines and types, including GC
tissues (22). Aberrantly activated
STAT3 has been found to enhance metastasis of tumors (23). In the present study, the hypothesis
that fascin may be an important downstream effector of
IL-6-regulated signaling, and that IL-6/STAT3 may sustain the basic
level of fascin and upregulate fascin expression in MKN45 cells,
was put forward.
For metastatic tumor cells, in addition to
enhancement of tumor cell motility (24), the ability to penetrate the
extracellular matrix (ECM) is crucial (25). Proteins which are secreted by tumor
cells, for example MMP-2 and -9, can destroy the ECM and facilitate
tumor cell invasion and metastasis (25). Al-Alwan et al showed that
MMP-2 and -9 can be upregulated by fascin (26). Fascin and STAT3 can activate
metastasis-associated molecules, including MMPs (26,27),
but the exact mechanisms by which IL-6-induced STAT3 activation and
fascin expression lead to cell migration and invasion are unclear.
In order to elucidate this, the JAK2/STAT3 signaling pathway was
downregulated in the present study, as IL-6 and STAT3 work together
in the tumor microenvironment to promote several cancer hallmarks,
for example increased proliferation, survival and invasion
(28). The levels of MMP-2 and -9,
which are critical for the execution of invasion and metastasis
(29), were significantly decreased
by STAT3 inhibition. STAT3 inhibition suppressed in vivo
liver metastasis of MKN45 cells, suggesting that STAT3 may be
indispensable for GC cell invasion and metastasis.
The Notch/Hes pathway crosstalk with STAT3 is also
implicated in gastric carcinogenesis (30) and signaling has been reported as a
reciprocal regulatory loop in the control of GC metastasis
(31). As activation of Notch
signaling can promote GC progression by enhancing STAT3
phosphorylation (31), we
hypothesized that the Notch/Hes pathway may also be involved in the
effects of IL-6 and the promotion of fascin expression in MNK45
cells. Notably, expression levels of the Notch target gene,
Hes-1, were significantly suppressed by Notch inhibitor
DAPT, but the downregulation of Notch/Hes signaling did not alter
basal or IL-6-induced fascin expression (Fig. 2B and E). Furthermore, blockade of
JAK/STAT3 with AG490 had no significant effect on the constitutive
expression of Notch1 and Notch2 (Fig.
2A) and IL-6-induced expression of Hes-1 (Fig. 2B). These results suggest that the
Notch/Hes signaling pathway may not be involved in the effects of
IL-6 and is not associated with STAT3 or fascin in MNK45 cells.
The NF-κB transcription factor is able to recruit
unphosphorylated STAT3 to promoters to activate transcription
(32). Additionally, the NF-κB
pathway positively regulates the expression of fascin (33) and can enhance metastasis of numerous
tumor types (34). However, whether
NF-κB has a direct effect on regulation of the STAT3-fascin loop of
GC remains unclear. Therefore, further experiments were performed
and data showed that NF-κB is recruited to the fascin promoter of
GC cells in a STAT3-dependent manner in response to IL-6 treatment.
These results suggest that, similar to STAT3, NF-κB is required for
IL-6-induced expression of fascin and functions at the
STAT3-dependent enhancer to increase fascin expression and promote
GC metastasis. However, the exact role of NF-κB in fascin
transcription in GC has not yet been established. Studies of
STAT3-regulated expression of fascin will provide new insight into
the mechanisms by which IL-6 promotes GC metastasis, in which
multiple factors contribute to the critical step of primary tumor
metastasis.
Whilst STAT3 and NF-κB are two parallel signaling
pathways in human cells, the present study found that they were
related and involved in the regulation of human GC metastasis. In
addressing the cross-talk mechanisms between these two signaling
pathways, possible links and fascin promoter activity were also
analyzed. Further detailed analyses of the fascin promoter and
specific interactions between transcription factors, for example
STAT3 and NF-κB, may also identify potential drug targets to block
metastasis. It has previously been shown that STAT3 regulates
Mucin-4 expression to promote GC metastasis (11). Thus, it is possible that, in the
presence of fascin, STAT3 may regulate other genes that function in
GC metastasis.
The present study has shown that STAT3 may act by
positively regulating fascin expression, NF-κB activity and
subsequent augmentation of cell migration and invasion. By
contrast, other unknown pathways may also be involved in regulating
fascin transcriptional activity via NF-κB. The present study
demonstrates a clear role for STAT3 in regulating GC metastasis,
partially through modification of the expression of
metastasis-associated genes, therefore making fascin a good target
for therapeutic intervention in metastatic GC cells. Improved
understanding of the fascin gene and the impinging signaling
cascades is required to improve understanding of STAT3-driven
processes contributing to increased fascin levels and,
consequently, to more aggressive cellular behavior of GCs.
Acknowledgements
This study was supported by grants from the National
Natural Science Foundation of China (no. 81001113), Zhejiang
Natural Science Foundation (nos. LQ13H190003 and LY12C05002), the
Science and Technology Plans of Taizhou City (no. 1301KY39), and
the Science and Technology Plans of Jiaojiang District of Taizhou
City (no. 132061).
References
|
1
|
Hartgrink HH, Jansen EP, van Grieken NC
and van de Velde CJ: Gastric cancer. Lancet. 374:477–490. 2009.
View Article : Google Scholar
|
|
2
|
Pasini F, Fraccon AP and Manzoni DEG: The
role of chemotherapy in metastatic gastric cancer. Anticancer Res.
31:3543–3554. 2011.PubMed/NCBI
|
|
3
|
Valastyan S and Weinberg RA: Tumor
metastasis: molecular insights and evolving paradigms. Cell.
147:275–292. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Smith SC and Theodorescu D: Learning
therapeutic lessons from metastasis suppressor proteins. Nat Rev
Cancer. 9:253–264. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hashimoto Y, Skacel M and Adams JC: Roles
of fascin in human carcinoma motility and signaling: prospects for
a novel biomarker? Int J Biochem Cell Biol. 37:1787–1804. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen L, Yang S, Jakoncic J, Zhang JJ and
Huang XY: Migrastatin analogues target fascin to block tumour
metastasis. Nature. 464:1062–1066. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hashimoto Y, Kim DJ and Adams JC: The
roles of fascins in health and disease. J Pathol. 224:289–300.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hashimoto Y, Shimada Y, Kawamura J,
Yamasaki S and Imamura M: The prognostic relevance of fascin
expression in human gastric carcinoma. Oncology. 67:262–270. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Okamoto W, Okamoto I, Arao T, Yanagihara
K, Nishio K and Nakagawa K: Differential roles of STAT3 depending
on the mechanism of STAT3 activation in gastric cancer cells. Br J
Cancer. 105:407–412. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Woo S, Lee BL, Yoon J, et al: Constitutive
activation of signal transducers and activators of transcription 3
correlates with better prognosis, cell proliferation and
hypoxia-inducible factor-1α in human gastric cancer. Pathobiology.
78:295–301. 2011.PubMed/NCBI
|
|
11
|
Mejías-Luque R, Peiró S, Vincent A, Van
Seuningen I and de Bolós C: IL-6 induces MUC4 expression through
gp130/STAT3 pathway in gastric cancer cell lines. Biochim Biophys
Acta. 1783:1728–1736. 2008.PubMed/NCBI
|
|
12
|
Lee MJ, Lee JK, Choi JW, et al:
Interleukin-6 induces S100A9 expression in colonic epithelial cells
through STAT3 activation in experimental ulcerative colitis. PLoS
One. 7:e388012012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang L, Yang J, Qian J, et al: Role of
the microenvironment in mantle cell lymphoma: IL-6 is an important
survival factor for the tumor cells. Blood. 120:3783–3792. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen J, Wang J, Lin L, et al: Inhibition
of STAT3 signaling pathway by nitidine chloride suppressed the
angiogenesis and growth of human gastric cancer. Mol Cancer Ther.
11:277–287. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Liu Q, Li G, Li R, et al: IL-6 promotion
of glioblastoma cell invasion and angiogenesis in U251 and T98G
cell lines. J Neurooncol. 100:165–176. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Snyder M, Huang XY and Zhang JJ: Signal
transducers and activators of transcription 3 (STAT3) directly
regulates cytokine-induced fascin expression and is required for
breast cancer cell migration. J Biol Chem. 286:38886–38893. 2011.
View Article : Google Scholar
|
|
17
|
Snyder M, Huang XY and Zhang JJ: Stat3 is
essential for neuronal differentiation through direct
transcriptional regulation of the Sox6 gene. FEBS Lett.
585:148–152. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Snyder M, Huang XY and Zhang JJ: Stat3
directly controls the expression of Tbx5, Nkx2.5, and GATA4 and is
essential for cardiomyocyte differentiation of P19CL6 cells. J Biol
Chem. 285:23639–23646. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sun J, He H, Xiong Y, et al: Fascin
protein is critical for transforming growth factor β
protein-induced invasion and filopodia formation in spindle-shaped
tumor cells. J Biol Chem. 286:38865–38875. 2011.
|
|
20
|
Fu H, Wen JF, Hu ZL, Luo GQ and Ren HZ:
Knockdown of fascin1 expression suppresses the proliferation and
metastasis of gastric cancer cells. Pathology. 41:655–660. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lee SA, Choi SR, Jang JS, et al:
Expression of VEGF, EGFR, and IL-6 in gastric adenomas and
adenocarcinomas by endoscopic submucosal dissection. Dig Dis Sci.
55:1955–1963. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Giraud AS, Menheniott TR and Judd LM:
Targeting STAT3 in gastric cancer. Expert Opin Ther Targets.
16:889–901. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bollrath J and Greten FR: IKK/NF-kappaB
and STAT3 pathways: central signalling hubs in
inflammation-mediated tumour promotion and metastasis. EMBO Rep.
10:1314–1319. 2009. View Article : Google Scholar
|
|
24
|
Jiang P, Enomoto A and Takahashi M: Cell
biology of the movement of breast cancer cells: intracellular
signalling and the actin cytoskeleton. Cancer Lett. 284:122–130.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fink K and Boratyński J: The role of
metalloproteinases in modification of extracellular matrix in
invasive tumor growth, metastasis and angiogenesis. Postepy Hig Med
Dosw (Online). 66:609–628. 2012.(In Polish).
|
|
26
|
Al-Alwan M, Olabi S, Ghebeh H, et al:
Fascin is a key regulator of breast cancer invasion that acts via
the modification of metastasis-associated molecules. PLoS One.
6:e273392011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kotipatruni RR, Nalla AK, Asuthkar S,
Gondi CS, Dinh DH and Rao JS: Apoptosis induced by knockdown of
uPAR and MMP-9 is mediated by inactivation of EGFR/STAT3 signaling
in medulloblastoma. PLoS One. 7:e447982012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sansone P and Bromberg J: Targeting the
interleukin-6/Jak/stat pathway in human malignancies. J Clin Oncol.
30:1005–1014. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Senft C, Priester M, Polacin M, Schröder
K, Seifert V, Kögel D and Weissenberger J: Inhibition of the
JAK-2/STAT3 signaling pathway impedes the migratory and invasive
potential of human glioblastoma cells. J Neurooncol. 101:393–403.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wu WK, Cho CH, Lee CW, Fan D, Wu K, Yu J
and Sung JJ: Dysregulation of cellular signaling in gastric cancer.
Cancer Lett. 295:144–153. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hsu KW, Hsieh RH, Huang KH, et al:
Activation of the Notch1/STAT3/Twist signaling axis promotes
gastric cancer progression. Carcinogenesis. 33:1459–1467. 2012.
View Article : Google Scholar
|
|
32
|
Yang J, Liao X, Agarwal MK, Barnes L,
Auron PE and Stark GR: Unphosphorylated STAT3 accumulates in
response to IL-6 and activates transcription by binding to
NFkappaB. Genes Dev. 21:1396–1408. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kress AK, Kalmer M, Rowan AG, Grassmann R
and Fleckenstein B: The tumor marker Fascin is strongly induced by
the Tax oncoprotein of HTLV-1 through NF-kappaB signals. Blood.
117:3609–3612. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wu Y and Zhou BP:
TNF-alpha/NF-kappaB/Snail pathway in cancer cell migration and
invasion. Br J Cancer. 102:639–644. 2010. View Article : Google Scholar : PubMed/NCBI
|