Introduction
Primary central nervous system non-Hodgkin’s
lymphoma (PCNSNHL) is rare and accounts for 0.8–1.89% of
intracranial tumors (1). The
occurrence of PCNSNHL confounded by another malignancy is extremely
uncommon. The pathogenesis of such a condition is not well
established. The present study describes a case of coexisting
PCNSNHL and colorectal adenocarcinoma for the first time. Written
informed consent was obtained from the patient’s family.
Case report
A 61-year-old female was admitted to Renji Hospital
(Shanghai, China) in December 2011 with a five-day history of night
sweats following a resection for non-Hodgkin’s lymphoma of splenium
corporis callosi. One month previously, the patient underwent
contrast-enhanced cranial magnetic resonance imaging for dizziness,
which indicated a splenium corporis callosi mass. Thus, the patient
underwent splenium corporis callosi mass resection. Frozen
pathology revealed lymphoma and immunohistochemistry identified
cells that were CD19(+++), Bcl-2(+), Bcl-6(+), CD23(−), CD5
(partially positive), CD10(+), CD20(+), CD43 (partially positive),
CK (pan)(−), glial fibrillary acidic protein(−), Ki-67 (60%
positive), CD2 (partially positive), neuron-specific enolase (−),
CD79a(+), multiple myeloma oncogene 1(+), CD3(+) and cyclin D1(+),
thereby confirming the presence of B cell lymphoma. The
post-operative recovery was good, but five days prior to admission,
the patient experienced night sweats. Following admission, a
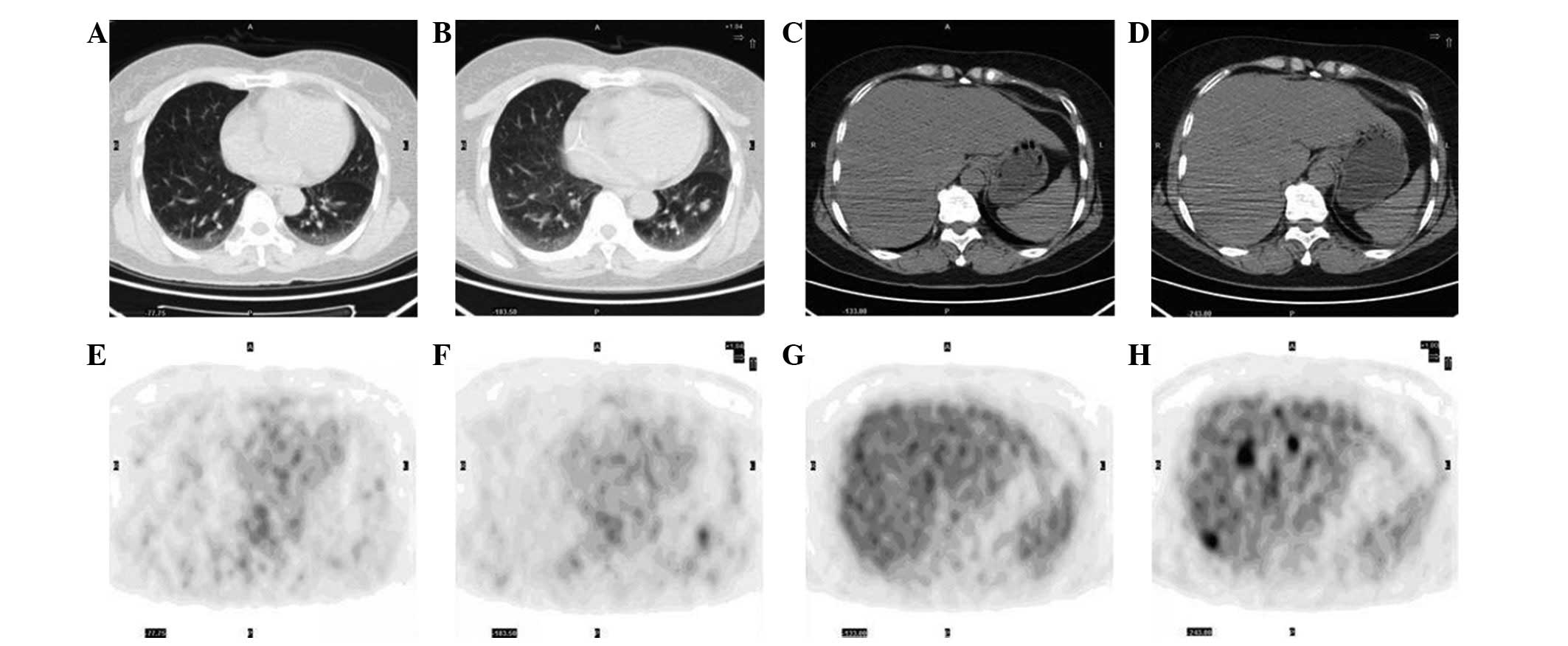
positron emission tomography-computed tomography (PET-CT) scan was
performed. The results indicated that tumor activity remained
following the non-Hodgkin’s lymphoma of splenium corporis callosi
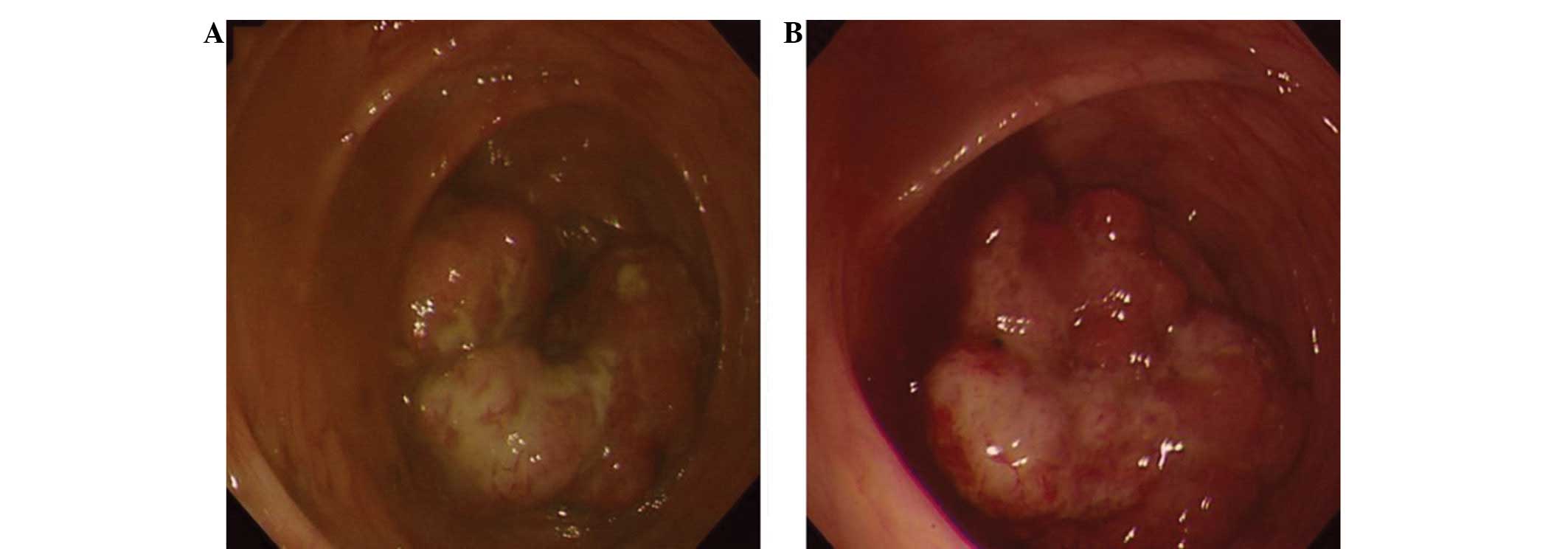
resection, and an ascending colon mass was identified. Electronic
colonoscopy was performed in order to identify the pathological
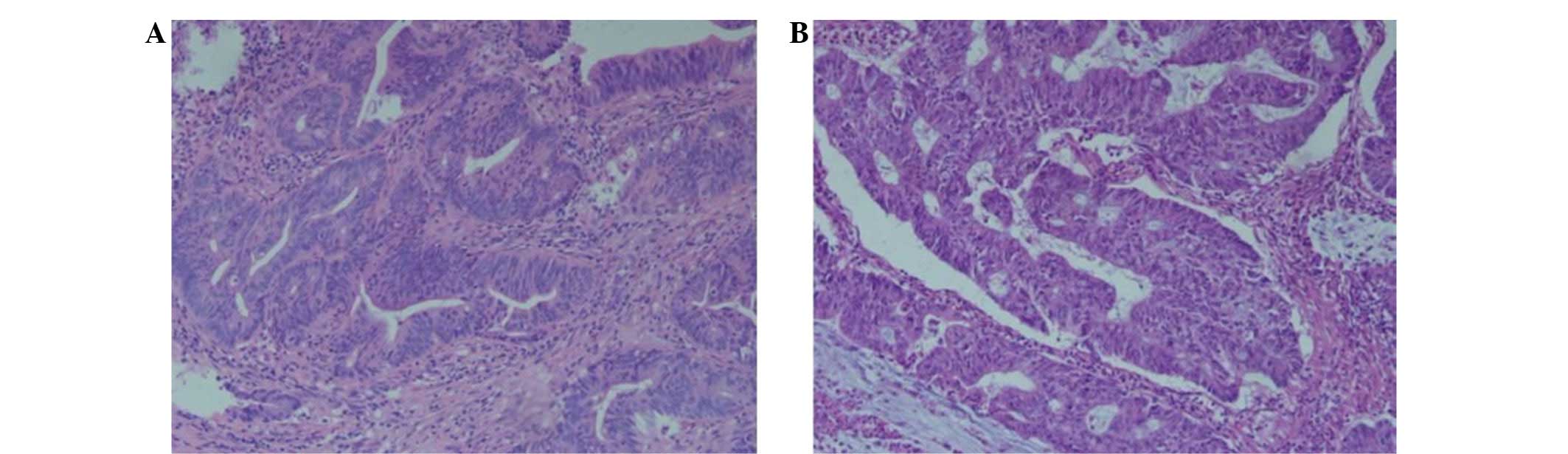
characteristics of the ascending colon mass (Fig. 1A). Biopsy revealed an ascending
colon high-grade intraepithelial neoplasia (Fig. 2A). Carcinoembryonic antigen (CEA)
and α-fetoprotein serum levels were negative. Although these
findings did not exclude the possibility of eventual malignancy,
the patient declined further treatment for the ascending colon
mass, simply accepting adjuvant chemotherapy following the lymphoma
resection.
Due to the aggravating abdominal discomfort, a
PET-CT scan was performed again in April 2012. The scan indicated
the possibility of primary intestinal malignancy with hepatic
multiple metastases and left lower lung metastasis. Biopsy under
electronic colonoscope revealed an ascending colon adenocarcinoma
(Figs. 1B and 2B). Therefore, hemicolectomy for the right
colon carcinoma was performed. The postoperative pathological
findings demonstrated a poorly and moderately differentiated
ascending colon adenocarcinoma and a partial mucinous
adenocarcinoma. Immunohistochemistry results were as follows:
Cytokeratin 7 (CK7) (−), CK20(+), CEA(+), TOPO IIa(−), P53(−),
Ki-67 (50%), HER-2(+) and cyclooxygenase 2(−).
Discussion
Synchronous carcinomas are defined as multiple
separate neoplasms that are diagnosed at the same time or within a
six-month period of identifying the primary lesion. The gross and
histological criteria of synchronous carcinomas, described by
Warren and Gates in 1932 (2), are
as follows: i) the neoplasms must be clearly malignant as
determined by histological evaluation; ii) each neoplasm must be
geographically separate and distinct; and iii) the possibility that
the second neoplasm represents a metastasis should be excluded.
Colorectal neoplasm confounded by lymphoma is in line with the
criteria. The condition is uncommon. As far as we are aware, all
the relevant studies are individual case reports (3–9) where
the two carcinomas are localized in the same site, including the
intestine or intestinal lymph nodes. Colorectal neoplasm confounded
by extraintestinal lymphoma is rarer. Chang et al (10) reported an Epstein-Barr
virus-positive case that was diagnosed as diffuse large B cell
lymphoma in the cranial cavity and the ileocecal junction area.
Following treatment with rituximab and chemotherapy, the cranial
carcinoma disappeared, but the ileocecal lesion remained.
Microscopic examination of the ileocecal lesion that was removed
surgically demonstrated that it was an adenocarcinoma confounded by
residual lymphoma.
All the previously mentioned studies had a
colorectal neoplasm and lymphoma in the same site. By contrast, the
present study described the case of an elderly female with
coexisting PCNSNHL and colorectal adenocarcinoma for the first
time, with lymphoma in the cranial cavity and adenocarcinoma in the
intestinal cavity. No hepatic or pulmonary metastases were observed
in the first PET-CT scan (Fig. 3A, B, E
and F), and the biopsy revealed a high-grade intraepithelial
neoplasia. After four cycles of chemotherapy, hepatic and pulmonary
metastases were discovered in the second PET-CT scan (Fig. 3C, D, G and H). The second biopsy
revealed adenocarcinoma. Similar changes were observed in the study
by Chang et al (10).
PCNSNHL may lead to systemic immune function changes, resulting in
intestinal tumorigenesis, which was accelerated by chemotherapy.
Although the metastases may simply be due to chance, it is
recommended that patients with PCNSNHL periodically undergo tumor
marker examinations, a whole-body CT scan and electronic
colonoscopy during chemotherapy.
The development of a malignancy, including
colorectal neoplasm and lymphoma involves oncogenes and associated
genes. The genes that are associated with colorectal neoplasm and
lymphoma have been identified to include C-myc, Bcl-2 and survivin
(11–17). C-myc is an oncogene that plays a
central role in the genesis of numerous human cancers. Bcl-2 and
survivin belong to the inhibitor of apoptosis family of proteins.
These genes are likely to take part in the development of a
synchronous occurrence of PCNSNHL and colorectal
adenocarcinoma.
In addition, common drugs in the chemotherapy
regimen for PCNSNHL are cyclophosphamide, doxorubicin, vincristine
and prednisone, while those in the chemotherapy regimen for
colorectal neoplasm are 5-fluorouracil, capecitabine and antitumor
platinum complexes. The two groups of drugs rarely overlap with
each other. Therefore, further research is required to identify how
to optimize the chemotherapy regimen in patients with coexisting
PCNSNHL and colorectal adenocarcinoma. C-myc, Bcl-2 and survivin
may offer breakthrough treatments for this disease in the
future.
References
|
1
|
Ferreri AJ, Reni M, Zoldan MC, Terreni MR
and Villa E: Importance of complete staging in non-Hodgkin’s
lymphoma presenting as a cerebral mass lesion. Cancer. 77:827–833.
1996.
|
|
2
|
Warren S and Gates O: Multiple primary
malignant tumors: a survey of the literature and statistical study.
Am J Cancer. 16:1358–1414. 1932.
|
|
3
|
Bhanote M, Choksi M, Cassar P, Edelman M,
DellaRatta R and Staszewski H: Metastatic adenocarcinoma of the
colon and follicular lymphoma within the same lymph node: a case
report and review of the literature. Int J Gastrointest Cancer.
36:171–175. 2005. View Article : Google Scholar
|
|
4
|
Devi P, Pattanayak L and Samantaray S:
Synchronous adenocarcinoma and mucosa-associated lymphoid tissue
lymphoma of the colon. Saudi J Gastroenterol. 17:69–71. 2011.
View Article : Google Scholar
|
|
5
|
Cornes JS: Multiple primary cancers:
primary malignant lymphomas and carcinomas of the intestinal tract
in the same patient. J Clin Pathol. 13:483–489. 1960. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kanehira K, Braylan RC and Lauwers GY:
Early phase of intestinal mantle cell lymphoma: a report of two
cases associated with advanced colonic adenocarcinoma. Mod Pathol.
14:811–817. 2001. View Article : Google Scholar
|
|
7
|
Mir-Madjlessi SH, Vafai M, Khademi J and
Kamalian N: Coexisting primary malignant lymphoma and
adenocarcinoma of the large intestine in an IgA-deficient boy. Dis
Colon Rectum. 27:822–824. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Padmanabhan V and Trainer TD: Synchronous
adenocarcinoma and mantle cell lymphoma of the colon. Arch Pathol
Lab Med. 127:E64–E66. 2003.PubMed/NCBI
|
|
9
|
Moriya Y, Koyama Y, Minato K, Shimoyama M,
Hirota T and Itabashi M: Coexisting malignant lymphoma and advanced
adenocarcinoma of the colon - a case report. Gan No Rinsho.
31:894–899. 1985.(In Japanese).
|
|
10
|
Chang H, Chuang WY, Shih LY and Tang TC:
Collision in the colon: concurrent adenocarcinoma and diffuse large
B-cell lymphoma in the same tumour. Acta Clin Belg. 66:302–304.
2011.
|
|
11
|
Bavi P, Uddin S, Bu R, Ahmed M, Abubaker
J, Balde V, Qadri Z, Ajarim D, Al-Dayel F, Hussain AR and Al-Kuraya
KS: The biological and clinical impact of inhibition of
NF-κB-initiated apoptosis in diffuse large B cell lymphoma (DLBCL).
J Pathol. 224:355–366. 2011.
|
|
12
|
Markovic O, Marisavljevic D, Cemerikic V,
Perunicic M, Savic S, Filipovic B and Mihaljevic B: Clinical and
prognostic significance of apoptotic profile in patients with newly
diagnosed nodal diffuse large B-cell lymphoma (DLBCL). Eur J
Haematol. 86:246–255. 2011. View Article : Google Scholar
|
|
13
|
Pedersen MØ, Gang AO, Poulsen TS, Knudsen
H, Lauritzen AF, Nielsen SL, Gang UO and Nørgaard P: Double-hit
BCL2/MYC translocations in a consecutive cohort of patients with
large B-cell lymphoma - a single centre’s experience. Eur J
Haematol. 89:63–71. 2012.
|
|
14
|
Schrader A, Bentink S, Spang R, Lenze D,
Hummel M, Kuo M, Arrand JR, Murray PG, Trümper L, Kube D and
Vockerodt M: High Myc activity is an independent negative
prognostic factor for diffuse large B cell lymphomas. Int J Cancer.
131:E348–E361. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sharrard RM, Royds JA, Rogers S and
Shorthouse AJ: Patterns of methylation of the c-myc gene in human
colorectal cancer progression. Br J Cancer. 65:667–672. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sun N, Meng Q and Tian A: Expressions of
the anti-apoptotic genes Bag-1 and Bcl-2 in colon cancer and their
relationship. Am J Surg. 200:341–345. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Xiaoyuan C, Longbang C, Jinghua W,
Xiaoxiang G, Huaicheng G, Qun Z and Haizhu S: Survivin: a potential
prognostic marker and chemoradiotherapeutic target for colorectal
cancer. Ir J Med Sci. 179:327–335. 2010. View Article : Google Scholar : PubMed/NCBI
|