Introduction
Secondary neoplasms of the testis are rare, with an
incidence of 0.9% in all testicular tumors according to a previous
German survey (1). The most common
location of the primary neoplasm is the prostate, followed by the
gastrointestinal tract, lungs and kidneys (2–4). Renal
cell carcinoma (RCC) commonly results in metastases to various
organs. Although RCC metastasis is frequently observed in the
lungs, lymph nodes, bones, liver and the brain, it is rarely
identified in the testes (5,6).
Several cases of unilateral testicular metastasis from RCC have
been reported (1,7). Dieckmann et al (1) reported 13 cases of unilateral
testicular metastases with detailed clinical information. They
speculated that testicular metastases have left lateral dominance
by analysing unilateral cases. However, simultaneous bilateral
testicular metastases have not yet been determined. This report
presented an extremely rare case of pathologically proven
simultaneous bilateral testicular metastases from RCC. In addition,
this study reviewed the previously reported cases of testicular
metastases from RCC.
Case report
A 65-year-old man was referred to the Saitama Red
Cross Hospital (Saitama, Japan) with a complaint of indolent left
scrotal enlargement over several months. Physical examination
revealed a stony, hard, hen’s egg-sized mass in the left scrotum. A
normal-sized testis with a small nodule was observed in the
contralateral scrotum. Superficial lymph nodes were not palpable.
Serum levels of α-fetoprotein, β-human chorionic gonadotropin and
soluble interleukin-2 receptor were all within normal limits.
Scrotal ultrasonography revealed a 4.0×3.3-cm mass in the left
testis and a 2.0×1.7-cm mass in the right testis. Contrast-enhanced
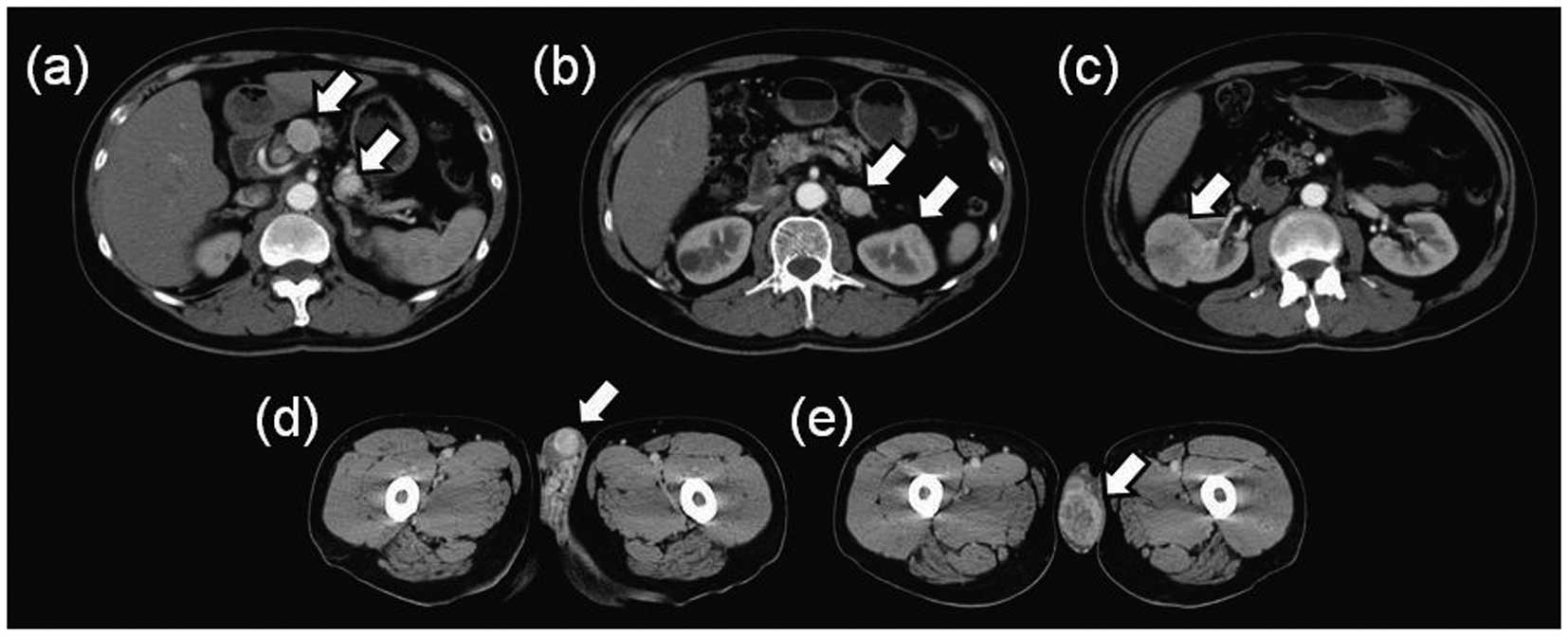
computed tomography of the abdomen identified multiple tumors in
the two kidneys, the pancreas and the left adrenal gland, in
addition to the testes (Fig. 1).
Imaging studies did not show metastasis in other regions, such as
the bone, lungs and brain.
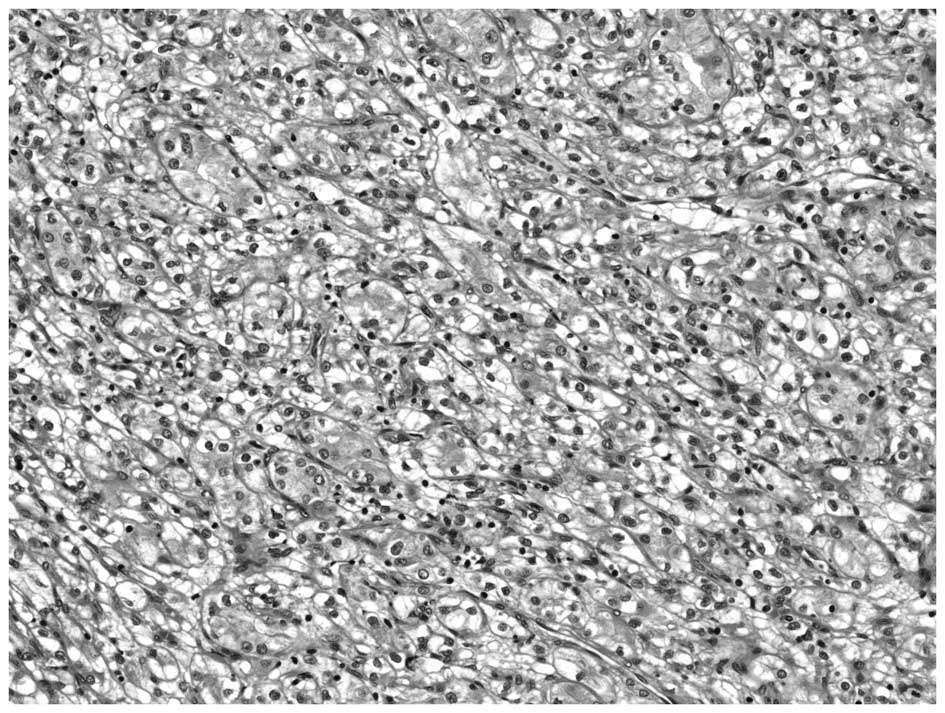
We performed left orchiectomy for pathological
diagnosis. The resected testis contained a yellowish-white tumor
with clear margins accompanied by parenchymal hemorrhage.
Pathological examination revealed that the tumor cells had small,
slightly oval nuclei with optically clear cytoplasm and were
arranged in nests separated by a rich network of sinusoidal
vascular channels (Fig. 2). These
results were compatible with a diagnosis of metastasis from clear
cell RCC. The patient was diagnosed with right RCC that was
metastasizing to the contralateral kidney and adrenal gland, the
pancreas and the testes (staging, cT1bN0M1).
All disseminated tumors were surgically resectable
and the patient’s general condition was good. Therefore, the
patient underwent partial pancreatectomy, left adrenalectomy and
left partial nephrectomy, followed by right radical nephrectomy and
right partial orchiectomy. Complete surgical resection was
achieved. The pathological findings of the resected tumors were
compatible with metastases from the right RCC (clear cell
carcinoma, Grade II, pT1b). Postoperative follow-up examination
without adjuvant therapy showed no recurrence for 11 months. The
patient provided written informed consent.
Discussion
Secondary neoplasms of the testis are rare with a
reported incidence of testicular metastasis of 0.02% (8) and 0.06% (2)at autopsy and testicular metastasis
accounted for 0.9% of all types of testicular tumors (1). Table I
summarized 30 cases of testicular metastasis from RCC. Bilateral
testicular metastasis from RCC has not been previously reported.
However, several cases of bilateral testicular metastases from
prostate cancer (9) and colorectal
cancer (10) have been
determined.
 | Table ITesticular metastasis from renal cell
carcinoma: review of the literature. |
Table I
Testicular metastasis from renal cell
carcinoma: review of the literature.
| | | | Laterality | |
|---|
| | | |
| |
|---|
| Case no. | Author | Year | Age, years | Testis | Kidney | Association between
the testis and the kidney | Solitary or multiple
metastases |
|---|
| 1 | Bandler and Roen | 1946 | 47 | R | R | Ipsilateral | Solitary |
| 2 | Tuchschmid | 1965 | 58 | L | L | Ipsilateral | Solitary |
| 3 | Hanash et
al | 1969 | 70 | R | R | Ipsilateral | NA |
| 4 | Talerman and
Kniestedt | 1974 | 68 | L | L | Ipsilateral | Solitary |
| 5 | Nataf et
al | 1975 | 64 | L | R | Contralateral | Solitary |
| 6 | Nataf et
al | 1975 | 55 | R | L | Contralateral | Multiple |
| 7 | DeBre et
al | 1980 | 63 | L | R | Contralateral | Solitary |
| 8 | Post and Kassis | 1980 | 64 | L | L | Ipsilateral | Solitary |
| 9 | Minervini et
al | 1984 | 56 | L | L | Ipsilateral | Solitary |
| 10 | Yano et
al | 1985 | 62 | L | L | Ipsilateral | Multiple |
| 11 | Ishizuka et
al | 1986 | 71 | L | L | Ipsilateral | Multiple |
| 12 | De Riese et
al | 1986 | 60 | L | L | Ipsilateral | Multiple |
| 13 | Dieckmann et
al | 1988 | 73 | L | L | Ipsilateral | Multiple |
| 14 | Indudhara et
al | 1990 | 67 | L | L | Ipsilateral | Solitary |
| 15 | Daniels et
al | 1991 | 87 | R | L | Contralateral | Solitary |
| 16 | Ribalta et
al | 1993 | 62 | R | R | Ipsilateral | Multiple |
| 17 | Blasco et
al | 1994 | 72 | L | L | Ipsilateral | Solitary |
| 18 | Lauro et
al | 1998 | 56 | R | L | Contralateral | Solitary |
| 19 | Steiner et
al | 1999 | 66 | L | R | Contralateral | Solitary |
| 20 | Nabi et
al | 2001 | 60 | R | L | Contralateral | Solitary |
| 21 | Datta et
al | 2001 | 81 | R | NA | NA | Multiple |
| 22 | Datta et
al | 2001 | 67 | L | R | Contralateral | Solitary |
| 23 | Datta et
al | 2001 | 85 | R | R | Ipsilateral | Solitary |
| 24 | Datta et
al | 2001 | 53 | R | NA | NA | Multiple |
| 25 | Marquez et
al | 2001 | 65 | R | R | Ipsilateral | Solitary |
| 26 | Nemoto et
al | 2007 | 56 | R | NA | NA | Multiple |
| 27 | Camerini et
al | 2007 | 46 | R | R | Ipsilateral | Multiple |
| 28 | Llarena et
al | 2008 | 57 | R | R | Ipsilateral | Multiple |
| 29 | Schmorl et
al | 2008 | 66 | R | R | Ipsilateral | Multiple |
| 30 | Hai-yang et
al | 2010 | 70 | L | R | Contralateral | Multiple |
| 31 | Present case | 2013 | 65 | Bilateral | R | Bilateral | Multiple |
Although RCC commonly results in metastases to
various organs, it rarely spreads to the testes. The testes are
regarded as a ‘tumor sanctuary’, as it has been hypothesized that
tumor cells are not able to grow easily in that environment. The
relatively low temperature of the scrotum could provide
unacceptable conditions for the establishment of metastatic tumor
cells (5). Additionally, the
presence of the blood-testis barrier formed by Sertoli cells, which
physiologically aims to protect spermatozoa, may also play an
indirect role in the prevention of testicular metastasis (6).
This study also searched previous medical literature
using the Medline/PubMed databases and identified 30 reported cases
of unilateral testicular metastasis from RCC, excluding autopsy
cases (Table I). Of the 30 cases,
15 were of left testicular metastases (50%) and 15 were of right
testicular metastases (50%). Although the left side is thought to
be involved more often than the right side (1,11), we
did not observe any particular laterality of testicular metastasis.
The association between primary kidney tumors and the testis
totaled 18 ipsilateral metastases and nine contralateral
metastases. Due to the tendency of metastasis from the kidney to
the testis on the same side, there may be important spreading
routes between the kidney and the testis. One of main routes could
be a retrograde venous spread via the spermatic vein (1,2,8). In
the present case, the primary kidney and the larger testicular
metastasis had the same laterality; therefore, superiority of
ipsilateral metastasis was suggested.
In conclusion, to the best of our knowledge, this
study was the first to present an extremely rare case of
simultaneous bilateral testicular metastases from RCC. Following a
review of the current literature, ipsilateral testicular metastasis
from RCC is more frequent and, thus, retrograde venous spread via
the spermatic vein may be one of the main pathways of testicular
metastasis from RCC. As demonstrated in this case, RCC can result
in testicular metastasis, not only unilaterally but also
bilaterally.
References
|
1
|
Dieckmann KP, Düe W and Loy V:
Intrascrotal metastasis of renal cell carcinoma. Case reports and
review of the literature. Eur Urol. 15:297–301. 1988.PubMed/NCBI
|
|
2
|
Pienkos EJ and Jablokow VR: Secondary
testicular tumors. Cancer. 30:481–485. 1972. View Article : Google Scholar
|
|
3
|
Dutt N, Bates AW and Baithun SI: Secondary
neoplasms of the male genital tract with different patterns of
involvement in adults and children. Histopathology. 37:323–331.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Haupt HM, Mann RB, Trump DL and Abeloff
MD: Metastatic carcinoma involving the testis. Clinical and
pathologic distinction from primary testicular neoplasms. Cancer.
54:709–714. 1984. View Article : Google Scholar
|
|
5
|
Blefari F, Risi O and Pino P: Secondary
tumors of testis: two rare cases and review of the literature. Urol
Int. 48:469–470. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Camerini A, Tartarelli G, Martini L,
Donati S, Puccinelli P and Amoroso D: Ipsilateral right testicular
metastasis from renal cell carcinoma in a responder patient to
interleukine-2 treatment. Int J Urol. 14:259–260. 2007. View Article : Google Scholar
|
|
7
|
Datta MW, Ulbright TM and Young RH: Renal
cell carcinoma metastatic to the testis and its adnexa: a report of
five cases including three that accounted for the initial clinical
presentation. Int J Surg Pathol. 9:49–56. 2001. View Article : Google Scholar
|
|
8
|
Hanash KA, Carney JA and Kelalis PP:
Metastatic tumors to testicles: routes of metastasis. J Urol.
102:465–468. 1969.PubMed/NCBI
|
|
9
|
Giannakopoulos X, Bai M, Grammeniatis E,
Stefanou D and Agnanti N: Bilateral testicular metastasis of an
adenocarcinoma of the prostate. Ann Urol. 28:(Paris). 274–276.
1994.(In French).
|
|
10
|
Hatoum HA, Abi Saad GS, Otrock ZK, Barada
KA and Shamseddine AI: Metastasis of colorectal carcinoma to the
testes: clinical presentation and possible pathways. Int J Clin
Oncol. 16:203–209. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nabi G, Gania MA and Sharma MC: Solitary
delayed contralateral testicular metastasis from renal cell
carcinoma. Indian J Pathol Microbiol. 44:487–488. 2001.PubMed/NCBI
|