Introduction
Deep neck space abscesses are common and the
majority of cases originate from infections or trauma to the head
and neck structures (1–5). A neck abscess or cervical cellulitis
as the initial presentation of carcinoma of unknown primary (CUP)
is rare. CUP is an uncommon malignancy and is defined as the
presence of metastatic cancer without an identifiable primary
origin (6–8). To the best of our knowledge, the
presentation of CUP as a deep neck abscess has not been previously
reported in the English literature. The aim of the present case was
to avoid potential pitfalls in the management of deep neck
abscesses. Furthermore, it was proposed that for the purpose of
accurate diagnosis, fine-needle aspiration of neck masses should be
conducted promptly according to the age of the patients and the
risk factors that are typically observed in malignancies.
Case report
Case presentation
A 71-year-old female, with a betel nut-chewing habit
and a history of hypertension, presented with a fever and a painful
swelling on the left side of the neck which had both lasted for
three days. The neck mass, which was diagnosed as a cervical
lymphadenitis at a local clinic, had been present for one week, had
progressively increased in size and had become red. The physical
examination showed that the patient had a temperature of 38.3°C and
presented with a tender mass (size, 3 cm) and skin erythema on the
left side of the neck at level II-III. The total white cell count
was 18.7×109/l and the C-reactive protein value was 12.3
mg/dl (normal value, <0.5 mg/dl). No additional clinical
abnormalities, such as transnasal fiberoptic laryngoscopy, were
identified as a result of the head and neck examinations. The
patient provided written informed consent.
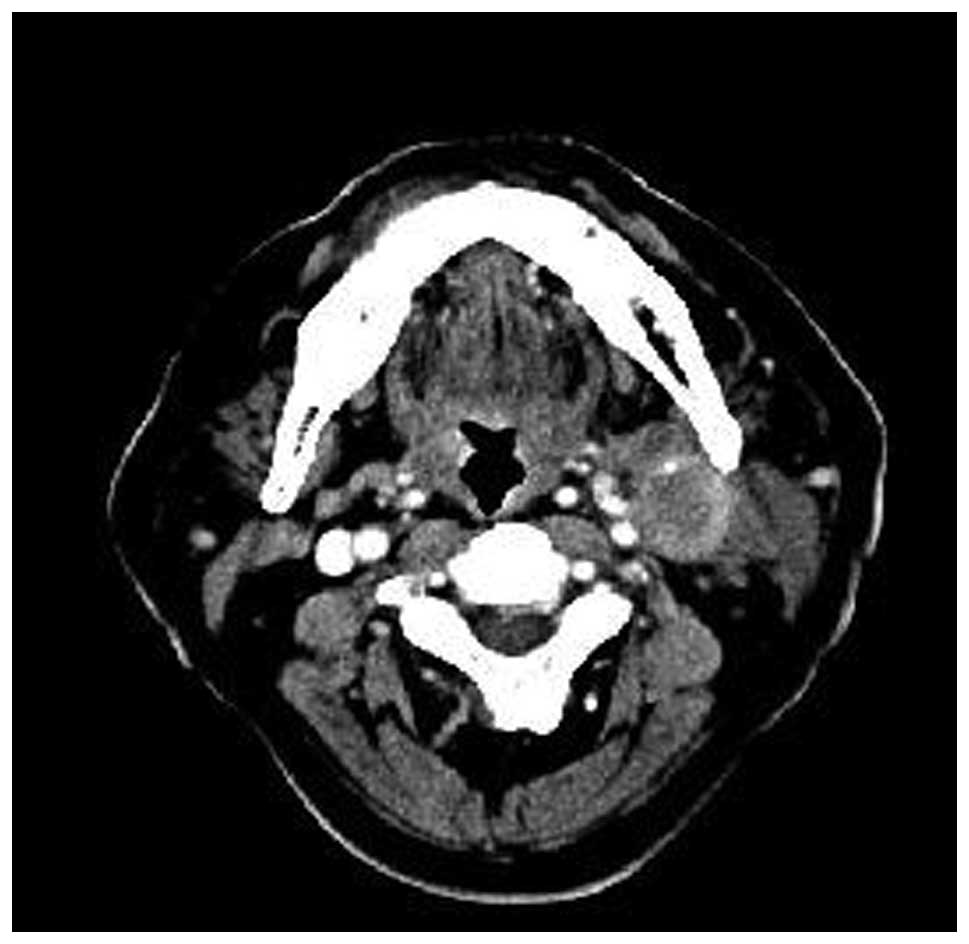
Imaging and diagnosis
An ultrasonographic scan showed a hypoechoic and
heterogeneous deep abscess between the left sternocleidomastoid
muscle and the common carotid artery. A contrast-enhanced computed
tomography scan of the neck was performed and a hypodense
predominantly cystic lesion, exhibiting ring enhancement over the
left carotid space, was observed (Fig.
1). The pus culture developed Staphylococcus aureus and
the cytological examination via fine-needle aspiration revealed the
presence of non-malignant inflammatory cells alone. Following
adequate control of the infection, the patient became afebrile and
the skin erythema ameliorated. However, the neck mass remained
present and the possibility of a malignancy could not be excluded
due to the patient regularly chewing betel nut and a concern
regarding the lateral cervical cystic lesion that the patient
exhibited. Therefore, an additional fine-needle aspiration of the
lesion was conducted and the cytology revealed malignant epithelial
cells, which were consistent with squamous cell carcinoma. The
diagnostic procedures were conducted to characterize the occult
carcinoma, although the results of the abdominal ultrasonographic
scan, chest radiography and the bone scintigraphy were all observed
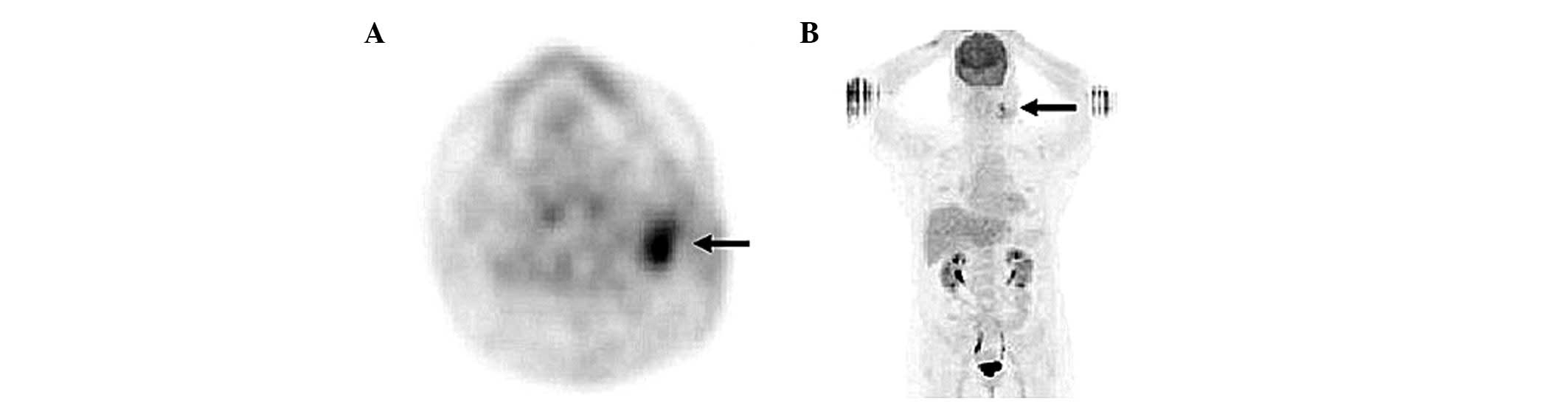
to be normal. The primary fluorodeoxyglucose (FDG) uptake site was
detected by F-18-FDG positron emission tomography in the lymph
nodes of the left-sided level II area of the neck, with a maximum
standardized uptake value of 5.7 (Fig.
2). Therefore, the patient was diagnosed as exhibiting a CUP
with lymph node metastasis in the neck, in addition to a deep neck
abscess.
Patient outcome
The patient subsequently underwent a left side
modified radical neck dissection, which was followed by
radiotherapy treatment. The patient survived and showed no
indication of recurrence within the five-year follow-up.
Discussion
Neck abscesses and deep neck infections are common
diseases, which may arise from various head and neck regions,
including the teeth, adenotonsillar tissues, the nasal cavity,
pharynx, paranasal sinuses and the salivary glands. Odontogenic and
tonsillar infections are the predominant causes; however,
malignancies may occasionally present with one of the
aforementioned deep neck infections. In previous studies, sporadic
cases of metastatic carcinoma presenting as deep neck abscesses
from certain head and neck regions were reported, such as the
paranasal sinus, nasopharynx, tonsil, tongue base, pharynx, larynx,
thyroid and parotid glands (1–5).
However, these were not related to CUP.
CUP was identified to account for ~3–5% of newly
diagnosed cancer patients in the Swiss population (6), representing a heterogeneous group. It
is defined as the presence of metastatic cancer without an
identifiable primary origin, based on obtaining a detailed medical
history and conducting precise clinical examinations, imaging of
anatomic sites and diagnostic investigations (7). Although patients who exhibit cervical
lymph node metastasis often present with a primary cancer site in
the head and neck region, no primary tumor was identified in a
previous study, despite extensive diagnostic workups in ~2% of the
patient group that was observed (8). In the present case, there was no
indication of the primary tumor. Thus, it was hypothesized that the
tumor had receded as a result of spontaneous regression by
apoptosis or immune-modulated destruction, following metastasis to
the local lymph nodes (9,10). Alternatively, the tumor may have
been too small for accurate sampling (11). However, the possibility that the
tumor cells may have originated from benign epithelial inclusions
in the lymph node of the neck and were destroyed by the growth and
spread of the tumor (12) could not
be excluded. Moreover, the occurrence of ectopic epithelium in the
lymph nodes is uncommon and embryonic admixing is the most likely
explanation (12).
Malignant lymph node metastasis, which presents as a
deep neck abscess or cervical cellulitis, is rare and may be due to
the relatively effective vascular supply to the head and neck
region (1). The causes and
predisposing factors for this type of deep neck infection remain
unknown; however, it has been hypothesized that the invariably
infected ulcer of the primary tumor is a potential source of the
abscess-forming bacteria, which drain into the lymph nodes
(2). Conversely, the center of a
large malignant lesion may be susceptible to infection due to tumor
necrosis, which results from an insufficient vascular supply
(3). The organism most commonly
observed in a tumor abscess is Staphylococcus aureus
(2).
The infections that coexist with the malignancy
complicate the clinical observations and may lead to a delayed
diagnosis. This is due to the infection superimposing on the
malignant process, which reduces the likelihood of obtaining a
biopsy that exhibits a good representation (4). In patients with a high risk of head
and neck squamous cell carcinomas, such as smokers, alcohol
drinkers, those that chew betel nut and elderly patients, a high
index of suspicion must be maintained even when the initial
cytology is benign. Furthermore, age may provide an indication into
the differential diagnosis of the patients that exhibit a deep neck
infection. Previous studies have identified that the average age of
patients (range, 40–74 years; median, 64 years), with deep neck
infections and malignancies, was two decades older than that of the
patients exhibiting simple pyogenic deep neck infections. These
commonly occur in a younger population, aged between 20 and 40
years (5), and the clinical
symptoms of the patients that were observed were similar to those
of the patients exhibiting a simple pyogenic deep neck infection.
Therefore, establishing a careful follow-up procedure after initial
treatment is recommended. This may enable the detection of possible
occult carcinomas in patients who exhibit an obscure etiology of
infection or those who present typical risk factors for squamous
cell carcinoma. Moreover, the current case demonstrated a
requirement for the careful review of cytological specimens, as in
the present study, the precise diagnosis was determined following
the repetition of the cytologic evaluation. It is likely that the
result of the initial pathological examinations of the abscess
aspirates or the abscess wall may be negative for malignancy when
there are abundant inflammatory cells; thus, the presence of a
marginal number of atypical clusters of cells may be ignored.
Furthermore, the clinical presentation may influence the diagnosis.
Although a benign pathology may be observed where the patient
exhibits a resolved neck abscess, these cases should be carefully
followed up as a malignancy may manifest during the convalescence
of the abscess.
In the management of these cases of deep neck
abscesses associated with malignancy, a definitive treatment for
the tumor and an appropriate treatment of the abscess are required.
In addition, detection of the primary site is critical as this may
result in patients receiving site-specific treatment with a
favorable prognosis. The majority of primary sites are able to be
confirmed pathologically, shortly following the diagnosis of a
cervical metastasis. Therefore, detailed medical history-tracing,
careful investigation and pathological examination of tissues
obtained from fine-needle aspiration or surgical biopsy in the
suspected malignancy area, are important to reduce the time it
takes to identify the primary malignant origin. Although the
primary origin of the malignancy in the present study was not
identified, a good recovery was observed following the modified
radical neck dissection and the radiotherapy treatment.
In conclusion, malignancies may present as deep neck
abscesses and patients may, therefore, require a careful
examination, particularly those who exhibit a high risk of head and
neck carcinoma.
References
|
1
|
Thompson HY, Fulmer RP and Schnadig VJ:
Metastatic squamous cell carcinoma of the tonsil presenting as
multiple cystic neck masses. Report of a case with fine needle
aspiration findings. Acta Cytol. 38:605–607. 1994.
|
|
2
|
Ross H: Metastatic squamous carcinoma in
lymph nodes with abscess formation. Aust N Z J Surg. 35:103–107.
1965. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee WC, Walsh RM and Tse A: Squamous cell
carcinoma of the pharynx and larynx presenting as a neck abscess or
cellulitis. J Laryngol Otol. 110:893–895. 1996.PubMed/NCBI
|
|
4
|
Op de Beeck K, Hermans R, Delaere PR, Van
den Bogaert W and Marchal G: Laryngeal squamous cell carcinoma
presenting as a prelaryngeal neck abscess: report of two cases. Eur
Radiol. 11:2479–2483. 2001.PubMed/NCBI
|
|
5
|
Wang CP, Ko JY and Lou PJ: Deep neck
infection as the main initial presentation of primary head and neck
cancer. J Laryngol Otol. 120:305–309. 2006.PubMed/NCBI
|
|
6
|
Levi F, Te VC, Erler G, Randimbison L and
La Vecchia C: Epidemiology of unknown primary tumours. Eur J
Cancer. 38:1810–1812. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Calabrese L, Jereczek-Fossa BA, Jassem J,
Rocca A, Bruschini R, Orecchia R and Chiesa F: Diagnosis and
management of neck metastases from an unknown primary. Acta
Otorhinolaryngol Ital. 25:2–12. 2005.PubMed/NCBI
|
|
8
|
Johansen J, Eigtved A, Buchwald C,
Theilgaard SA and Hansen HS: Implication of
18F-fluoro-2-deoxy-D-glucose positron emission tomography on
management of carcinoma of unknown primary in the head and neck: a
Danish cohort study. Laryngoscope. 112:2009–2014. 2002. View Article : Google Scholar
|
|
9
|
Sperduto P, Vaezy A, Bridgman A and Wilkie
L: Spontaneous regression of squamous cell lung carcinoma with
adrenal metastasis. Chest. 94:887–889. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Husseini S, Krauss DJ and Rullis I:
Spontaneous regression of metastatic embryonal testicular
carcinoma: 22-year followup. J Urol. 136:119–120. 1986.PubMed/NCBI
|
|
11
|
Dong MJ, Zhao K, Lin XT, Zhao J, Ruan LX
and Liu ZF: Role of fluorodeoxyglucose-PET versus
fluorodeoxyglucose-PET/computed tomography in detection of unknown
primary tumor: a meta-analysis of the literature. Nucl Med Commun.
29:791–802. 2008.PubMed/NCBI
|
|
12
|
Morita Y, Yamagishi M, Shijubo N, Nakata
H, Kurihara M and Asakawa M: Squamous cell carcinoma of unknown
origin in middle mediastinum. Respiration. 59:344–346. 1992.
View Article : Google Scholar : PubMed/NCBI
|