Introduction
Primary squamous cell carcinoma (SCC) arising from
an unknown primary site and metastasizing to the stomach is
extremely rare (1–9). Due to the poor prognosis associated
with primary SCC and the requirement for an appropriate diagnosis,
special attention is required that may lead to an improved
therapeutic strategy. In the present study, a unique case of an SCC
in the interspace between the liver and stomach is reported.
Furthermore, the present report identifies the possible
pathogenesis, diagnosis and treatment of this type of tumor. The
study was approved by the ethics committee of Subei People’s
Hospital of Jiangsu Province (Yangzhou, China) and the patient
provided consent for publication.
Case report
A 59-year-old male was admitted to Subei People’s
Hospital of Jiangsu Province on June 21, 2012, complaining of upper
abdominal pain with no evident inducible factor, which had
persisted for one month; the pain was discontinuous and dull. The
patient’s past medical history was unremarkable, with the exception
of mild weight loss. The patient had smoked one pack of cigarettes
per day for 25 years. A physical examination revealed no abdominal
mass; however, there was tenderness in the right upper quadrant of
the abdomen.
Laboratory studies revealed that the complete blood
count and blood chemistry were within the normal range. No abnormal
tumor markers were detected: Cancer antigen (CA)125, 3.15 KU/l
(<35.00 KU/l); CA15-3, 2.16 KU/l (<35.00 KU/l); CA19-9, 3.57
KU/l (<35.00 KU/l); CA242, 2.58 KU/l (<20.00 KU/l);
α-fetoprotein, 6.57 ng/ml (<20.00 ng/ml); carcinoembryonic
antigen, 2.25 ng/ml (<5.00 ng/ml); neuron-specific enolase,
<1.0 ng/ml (<13.00 ng/ml); ferritin, 19.70 ng/ml (male,
<322.00 ng/ml; female, <219.00 ng/ml); human growth hormone,
2.20 ng/ml (<7.50 ng/ml); or β-human chorionic gonadotropin,
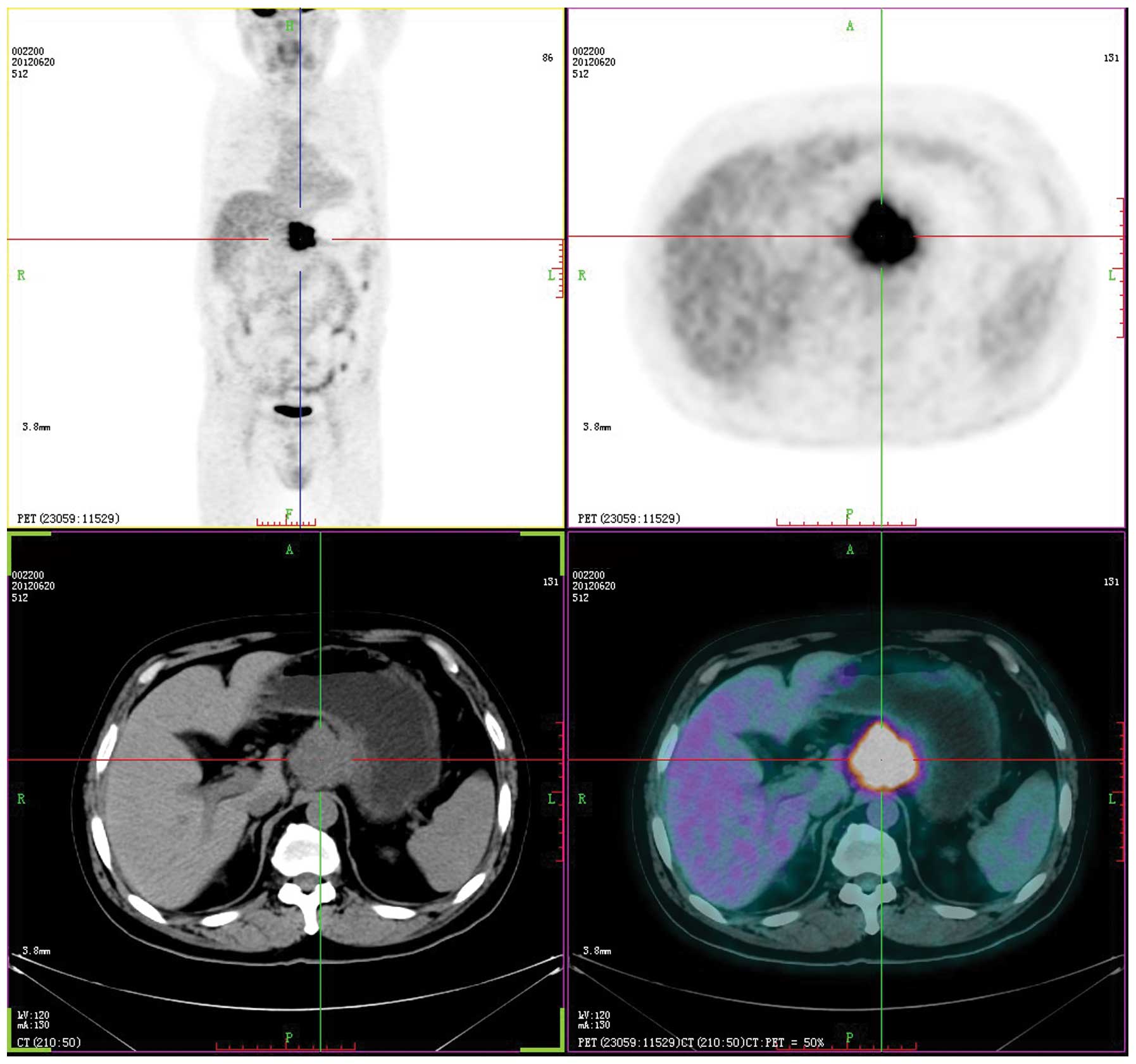
<0.03 mIU/ml (<3.00 mIU/ml). Axial positron emission
tomography (PET), computed tomography (CT), PET/CT and maximum
intensity projection images are shown in Fig. 1. PET/CT identified a hypermetabolic
lesion in the interspace between the liver and stomach. There was
no additional fludeoxyglucose (18F) uptake, which indicated a
primary site on the transaxial PET/CT scans of the head, neck,
chest, pelvis, extremities or other abdominal organs (including the
spleen, pancreas, gallbladder, kidney, large and small intestines).
The patient subsequently underwent surgical resection. The tumor
was located in the interspace between the liver and stomach, it
measured 6×5 cm, was close to the left gastric artery, and invaded
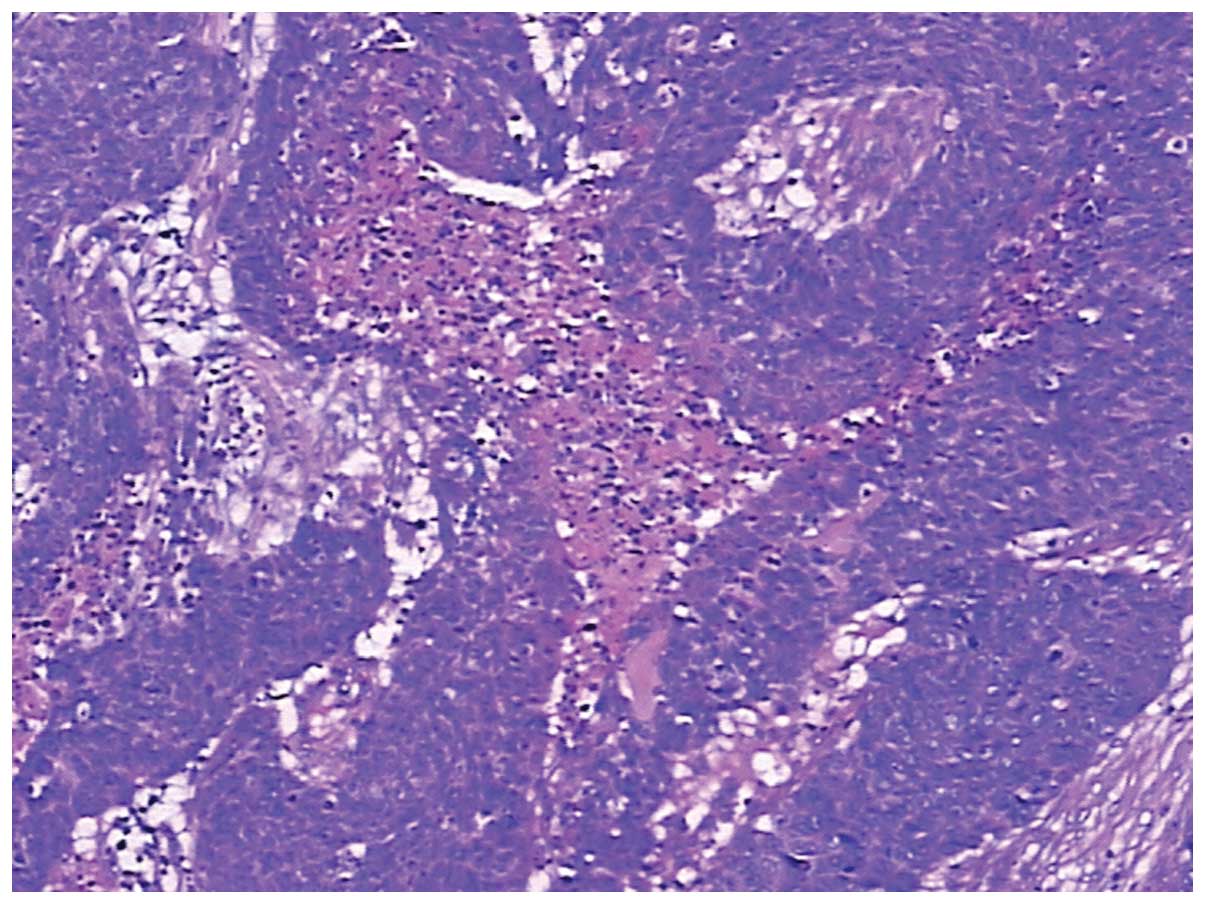
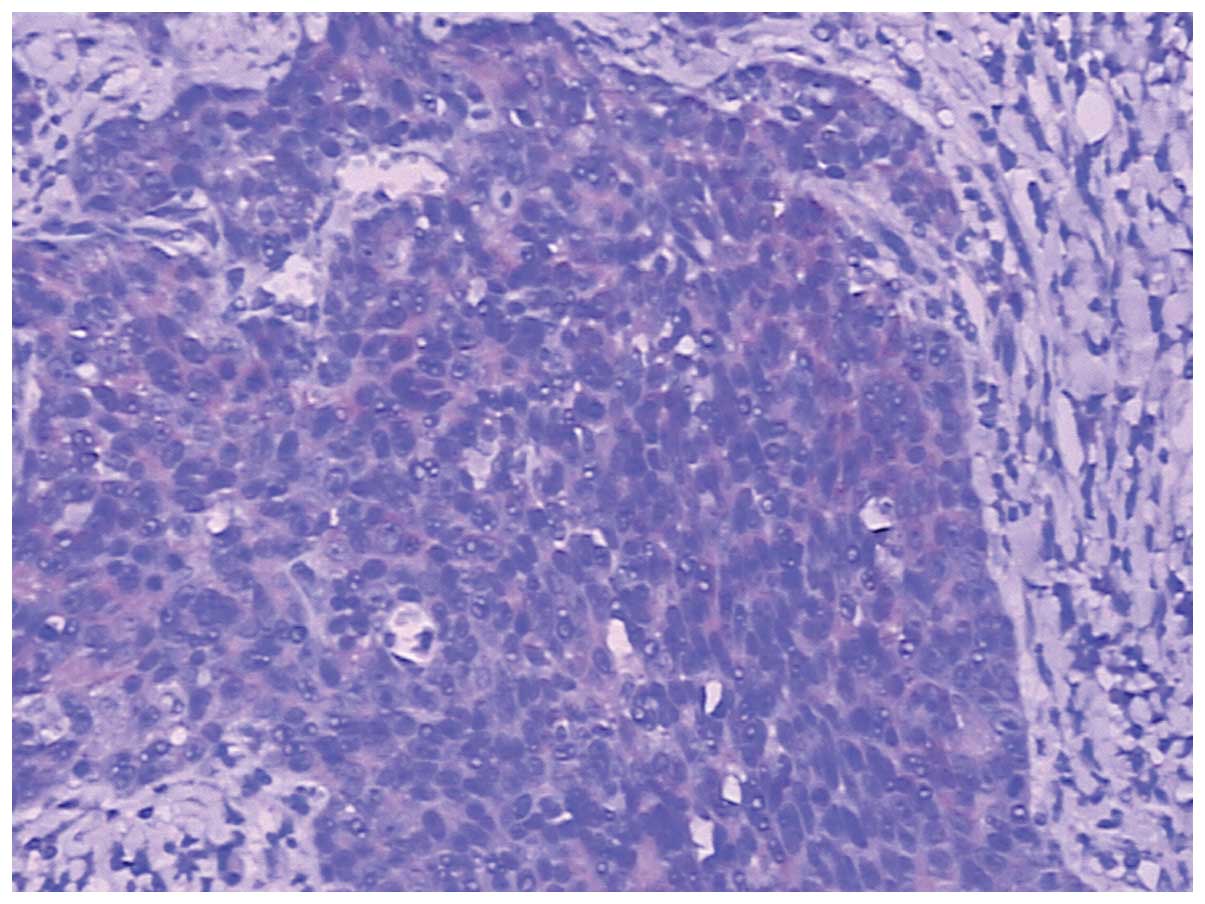
the gastric wall and the pancreas. Intraoperative fast pathological
sections revealed that the tumor tissues were composed of nidulant,
multi-mitotic cells and necrosis, which were identified as SCC
(Fig. 2); therefore, the tumor was
resected and a proximal gastrectomy was performed.
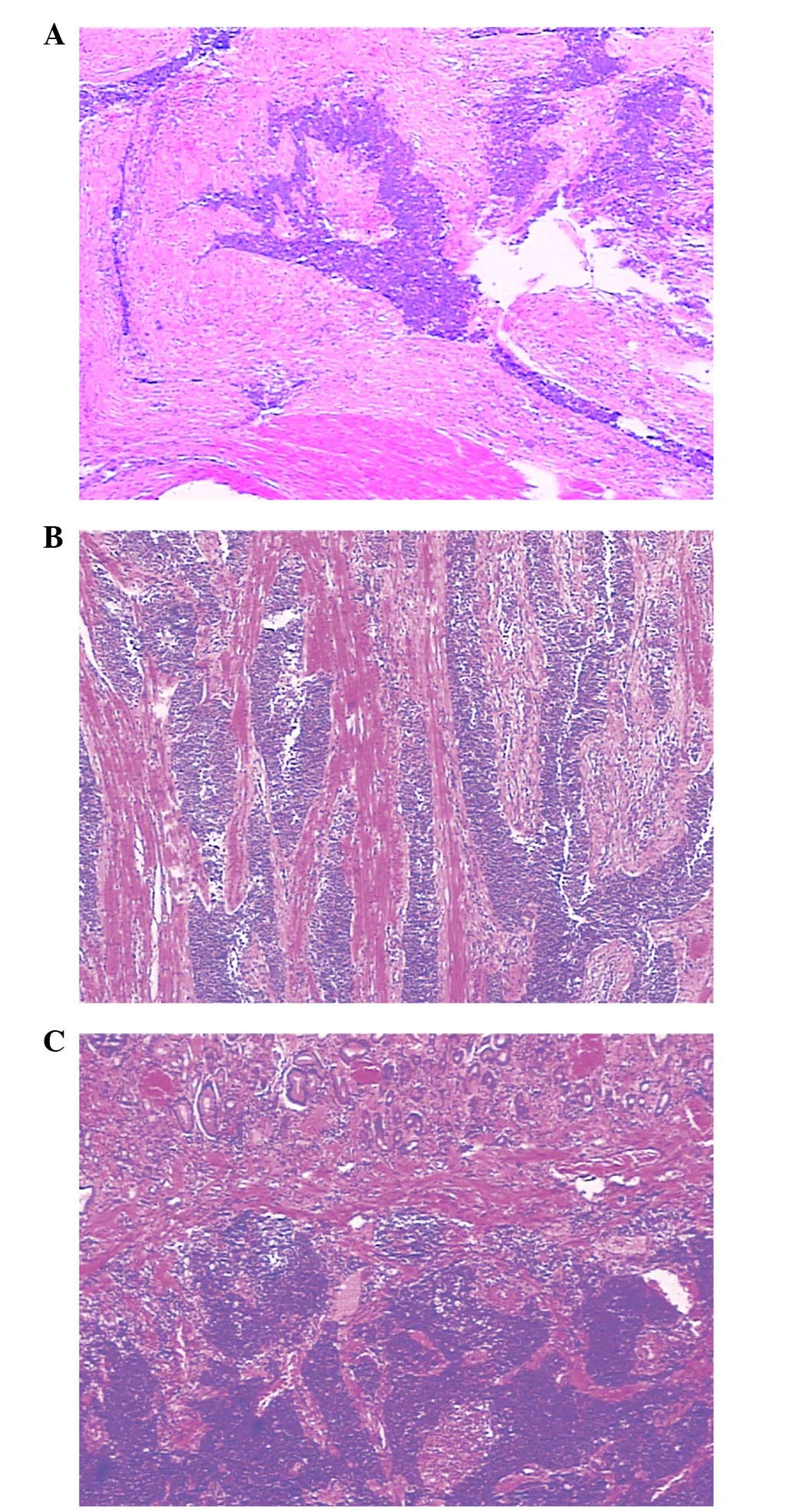
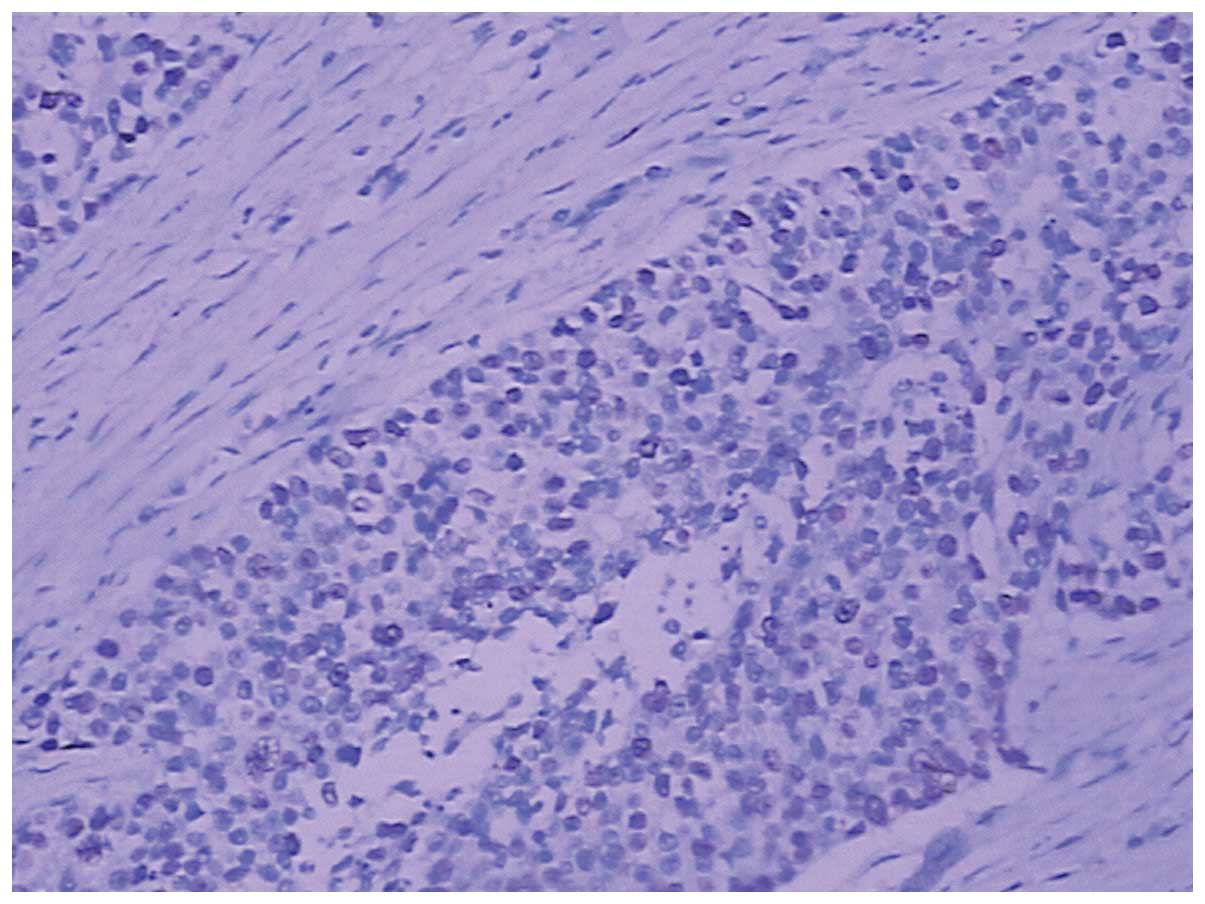
Histopathology revealed that the SCC infiltrated
into the serosal fibrous tissue, lamina muscularis and submucosa of
the gastric wall (Fig. 3A–C);
however, there was no cancer cell infiltration into the mucosa. The
surgical margins were negative, however, metastasis to one lymph
node in the lesser curvature of the stomach was observed.
Furthermore, the esophagogastric junction was negative for the
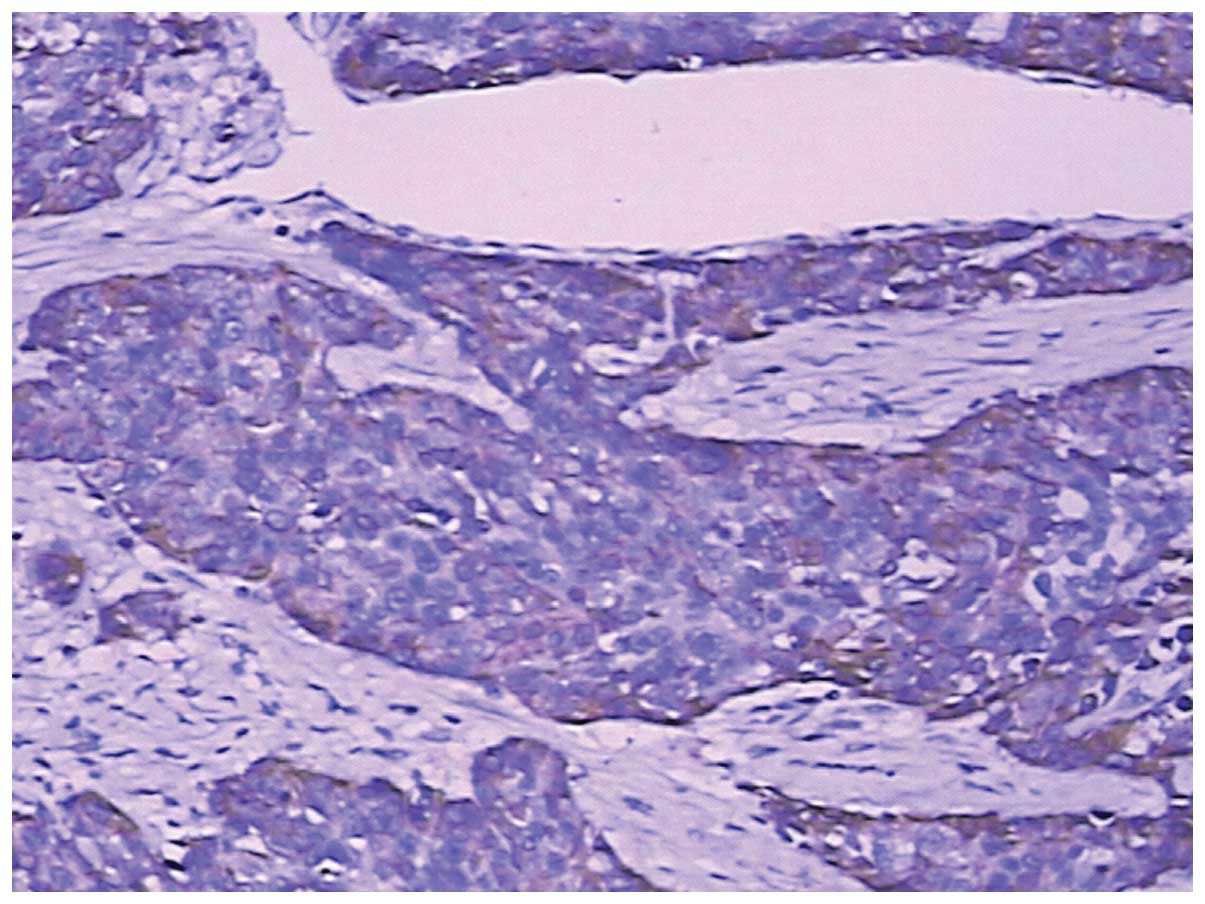
tumor. The immunohistochemical staining was positive for
cytokeratin (CK)5/6, p63, CKpan and glutathione S-transferase π
(Figs. 4–7), and negative for cluster of
differentiation (CD)56, CDX-2, chromogranin A, CK20, CK7, S100,
Syn, Villin, P-glycoprotein, epidermal growth factor receptor,
topoisomerase II and p53. The Ki-67 proliferation index was ~50%
(Fig. 8). Due to the progression of
the disease, postoperative chemotherapy was recommended, and the
patient and the patient’s family consented to four sessions of
chemotherapy. At the end of the 12-month follow-up, which was
conducted using ultrasonography and CT, the patient had survived
and there was no evidence of recurrence and metastasis.
Discussion
Primary SCC of the stomach was first described in
1895 (10) and remains a rare
entity. SCC occurs mostly in males (male to female ratio, 5:1)
(11). The diagnostic criteria for
primary SCC of the stomach are as follows: The tumor must not be
located in the cardia; the tumor must not extend into the
esophagus; and there must be no evidence of SCC in any other
organs. In the present case, the cardia was intact and the 5-cm
segment between the esophagus and the proximal portion of the tumor
was normal. No SCC findings were determined in other organs during
the physical examination. Throughout the follow-up period, there
was no evidence of other malignant tumors in the patient. Boswell
and Helwig (12) defined four
histopathological criteria that are required for the diagnosis of
SCC of the stomach: Presence of keratinizing cell masses with pearl
formation, a mosaic cell arrangement, intracellular bridges and
high concentrations of sulfhydryl or disulfide bonds, which
indicate keratin production.
To reach a diagnosis of primary SCC of the stomach,
alternative sources of malignant squamous cells must be excluded.
For example, islands of squamous cells originating from the
esophagus may exist in the cardia and may be a potential source for
the development of SCC. SCCs that originate in the esophagus itself
may extend into the stomach by direct invasion. Primary SCC may
originate elsewhere in the body (for example, the head, neck, lung,
bronchus and cervix uteri) and metastasize to the stomach.
Metastatic disease from such sites may be ruled out by clinical
examination, particularly PET/CT.
Usually, primary SCC of the stomach initially invade
the mucosa; those limited to outside the area of the mucous
membrane are extremely rare. Histologically, the tumor tissues were
located outside the area of the mucous membrane without adenoid
tumor tissue structures or tumor mucosal lesions; therefore, it may
be considered that the tumor tissues were not associated with the
mucosal epithelium and glands. Therefore, the present case is
neither primary SCC nor adenoacanthoma of the stomach. Furthermore,
gross and pathological examinations eliminated direct invasion of
the esophageal SCC into the stomach. No tumors were determined in
other organs during the physical examination that included PET/CT.
Therefore, the tumor was identified as a metastatic gastric tumor
or an SCC arising from an unknown primary site and metastasizing to
the stomach.
In a previous study, immunohistochemical staining
showed strong staining for high molecular weight CK5/6 and p63 in
the SCC (1). The
immunohistochemical findings of the case in the present study were
consistent with these. Therefore, immunohistochemical examination
should be performed and immunomarkers, including CK5/6 and p63,
should be included in the immunohistochemistry examination.
Since the tumor is extremely uncommon, the mechanism
has not been well elucidated. Numerous pathological processes have
been proposed, including heterotopic squamous epithelium, squamous
metaplasia, multipotent stem cells capable of differentiating into
cells of any type, overgrowth of the squamous component in primary
adenocarcinoma and local extension or metastasis of esophageal SCC
(13). The favored suggestion is
the malignant transformation in an area of squamous metaplasia. The
development of SCC in the absence of metaplasia, but with chronic
inflammation, has previously been reported (1). Straus et al (14) performed detailed histological
examinations of patients that were considered to have pure SCC and
demonstrated the presence of glandular components. Mori et
al (13) proposed the following
hypothesis based on these findings: Neoplastic multipotent cells
initially become adenocarcinomas, which is followed by the
occurrence of squamous metaplasia and subsequent conversion into
SCC.
Owing to the rarity and advanced presentation of
SCC, there is a lack of evidence to support a particular management
strategy and prognosis is difficult to predict. Surgery to achieve
R0 (no residual tumor) resection remains the mainstay of the
treatment and is well supported by adjuvant therapies as reported
in the present study. Regardless of undergoing only four
chemotherapy sessions, the patient in the present study did not
exhibit recurrence or metastasis; therefore, paclitaxel and
platinum-based agents are recommended. A good response to
chemoradiotherapy, with respect to recurrence, following surgical
resection was reported by Michalet et al (15). Adjuvant radiotherapy following
surgical resection and subsequent chemotherapy have resulted in
survival periods of >3 years, in a case of advanced stage SCC
the patient was free of recurrence with a good quality of life for
five years (2). Good long-term
survival in gastric SCC has been reported with chemotherapy alone
despite locally invasive tumors (3). However, insufficient information is
available on the adjuvant role of chemoradiotherapy in SCC arising
from an unknown primary site metastasizing to the stomach compared
with other digestive tumors, such as esophageal SCC, where it has
been shown to have a definite role. Its pathogenesis, diagnosis and
treatment remain a topic of debate and further studies would
benefit the patients that are affected by this rare disease.
In conclusion, a rare case of SCC from an unknown
primary site metastasizing to the stomach is presented. To the best
of our knowledge, this is the first case report to have
investigated this tumor type. The pathogenesis, diagnosis and
treatment of an SCC of this type has generally been considered
poor, thus, additional cases require investigation to confirm
this.
References
|
1
|
Callacondo D, Ganoza-Salas A, Anicama-Lima
W, et al: Primary squamous cell carcinoma of the stomach with
paraneoplastic leukocytosis: a case report and review of
literature. Hum Pathol. 40:1494–1498. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schmidt C, Schmid A, Lutteges JE, et al:
Primary squamous cell carcinoma of the stomach. Report of a case
and review of literature. Hepatogastroenterology. 48:1033–1036.
2001.PubMed/NCBI
|
|
3
|
Yildirim Y, Akcali Z, Bilezikci B, et al:
Primary squamous cell carcinoma of the stomach: a case report.
Tumori. 91:440–442. 2005.PubMed/NCBI
|
|
4
|
Dursun M, Yaldiz M, Isikdogan A, et al:
Primary squamous cell carcinoma of the stomach: a case report and
review of the literature. Eur J Gastroenterol Hepatol. 15:329–330.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Akbulut S, Finci R and Ozyilkan E: Primary
squamous cell carcinoma of the stomach: a case report. Acta
Gastroenterol Belg. 66:189–190. 2003.PubMed/NCBI
|
|
6
|
Takita J, Kato H, Miyazaki T, et al:
Primary squamous cell carcinoma of the stomach: a case report with
immunohistochemical and molecular biologic studies.
Hepatogastroenterology. 52:969–974. 2005.PubMed/NCBI
|
|
7
|
Amuluru K and Gupta H: Primary squamous
cell carcinoma of the stomach: a case report. J Gastrointest
Cancer. 41:24–26. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Karaca G, Pekcici MR, Ozer H, et al:
Primary squamous cell carcinoma of the stomach in a 68-years-old
man. Geriatr Gerontol Int. 11:119–120. 2011.PubMed/NCBI
|
|
9
|
Dursun M, Yaldiz M, Isikdogan A, et al:
Primary squamous cell carcinoma of the stomach: a case report and
review of the literature. Eur J Gastroenterol Hepatol. 15:329–330.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Muto M, Hasebe T, Muro K, et al: Primary
squamous cell carcinoma of the stomach: a case report with a review
of Japanese and Western literature. Hepatogastroeneterology.
46:3015–3018. 1999.PubMed/NCBI
|
|
11
|
Volpe CM, Hameer HR, Masetti P, et al:
Squamous cell carcinoma of the stomach. Am Surg. 61:1076–1078.
1995.PubMed/NCBI
|
|
12
|
Boswell JT and Helwig EB: Squamous cell
carcinoma and adenoacanthoma of the stomach. A clinicopathologic
study. Cancer. 18:181–192. 1965. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mori M, Iwashita A and Enjoji M: Squamous
cell carcinoma of the stomach: report of three cases. Am J
Gastroenterol. 81:339–342. 1986.PubMed/NCBI
|
|
14
|
Straus R, Heschel S and Fortmann DJ:
Primary adenosquamous carcinoma of the stomach. A case report and
review. Cancer. 24:985–995. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Michalet V, Gaudin JL, Bancel B, et al:
Squamous cell carcinoma of the celiac area. Report of a case and
review of the literature. Gastroenterol Clin Biol. 26:1168–1171.
2002.(In French).
|