Introduction
Hyperthermia has long been established as a
treatment option for cancer, particularly for superficial types of
cancer (1). Hyperthermia is used
alone or as an adjunct to radiotherapy or chemotherapy (2–5).
Traditional hyperthermia (41–43°C, or even lower) can
synergistically enhance the therapeutic effects of radiotherapy by
inducing apoptosis. In hyperthermia with thermal ablation
(>60°C), direct killing of tumor cells occurs by necrosis
(6,7).
High temperatures (>46°C) can directly induce
cell damage, including severe protein denaturation and DNA damage
(8,9). These changes are irreversible and
ultimately result in cell death. Tumor cells express specific
tumor-associated antigens. In high-temperature (e.g. >46°C)
conditions, tumor cells swell and break into pieces, allowing
antigen release. This creates a large antigen load for the
generation of antitumor immunity. Although high temperatures cause
severe protein denaturation, this is likely to destroy the
immunogenicity of tumor cells (10–14).
When thermal ablation temperatures (>60°C) are achieved, there
is a high risk of shock syndrome induced by the sudden and large
production of necrotic tumor material. However, a relatively low
temperature range (46–55°C) can increase the proportion of
apoptotic cells among the dead cells, which is likely to reduce the
risk of shock syndrome (15). To
the best of our knowledge, there are no previous studies which
aimed to determine the correlation between temperatures of 50–70°C
and antitumor effects.
Glioma is the most common brain tumor. Surgery,
chemotherapy and radiotherapy form the basis of glioma treatment.
However, the prognosis of patients with glioma is poor (16). The development of alternative
therapies for patients with glioma is essential to improve their
prognosis. Previously, it was indicated that hyperthermia can
prolong the survival time and rate of patients with glioma
(17). Specific reports have
revealed the mechanisms of action of hyperthermia on glioma cell
lines (18,19). However, mild-temperature
hyperthermia was utilized in these studies.
The aim of the present study was to clarify the
exact correlation between high-temperature hyperthermia (HTH) at
50–70°C and the resulting antitumor effects, using a glioma rat
model. The effects of HTH were evaluated in a glioma rat model by
histopathological examination.
Materials and methods
Treatment device
In this study, a tissue ablation device for
veterinary medicine (AMTC 200; Alexon Inc., Ehime, Japan) was used.
This device can regulate temperature between 50 and 70°C.
Preparation of the glioma-bearing mouse
model
F344 rats (female; 31–37 weeks old) were purchased
from CLEA Japan (Osaka, Japan). The animals were maintained under
conventional conditions. The use of these animals and the
procedures they underwent were approved by the Animal Research
Committee of Tottori University (Torrati, Japan).
9L cells were maintained in E-MEM (Wako, Inc.,
Osaka, Japan) containing 10% fetal bovine serum, 0.1 mg/ml
neomycin, 0.05 mg/ml streptomycin and 0.05 mg/ml penicillin at 5%
CO2 and 37°C under a humidified atmosphere in an
incubator. The rats were anesthetized via inhalation of 3–5%
isoflurane (Intervet, Inc., Tokyo, Japan). In total,
2.5×107 cells (0.2 ml) were injected subcutaneously into
the dorsal regions of each rat. Rats with tumor diameters exceeding
10 mm were used for the experiment.
Study design
Rats (n=14) were randomized into four groups:
Nontreatment (NT; n=3), 70°C (T-70) HTH (n=3), 60°C (T-60) HTH
(n=4) and 50°C (T-50) HTH (n=4) groups. The tumor growth rates were
calculated according to the tumor volumes (mm3/day). On
day 0, HTH was performed for 10 min at 70, 60 or 50°C. On days 0,
3, 6, 9 and 12, the volumes of the tumor tissues were calculated by
measuring the mediastinum, transverse length and depth of each
tumor. The tumor tissues were removed on day 12 and fixed in 10%
buffered formalin.
Histological examination
Fixed samples were embedded in paraffin and
sectioned in a routine manner. The sections were subjected to
hematoxylin-eosin (HE), Ki-67 and terminal dUTP nick-end labeling
(TUNEL) staining.
For Ki-67 staining, tissue sections (3 μm) on glass
slides were deparaffinized, washed with ethanol and water, and
soaked in phosphate-buffered saline (PBS). The sections were
autoclaved with 0.01 M citrate buffer (pH 6.0) for 15 min (121°C).
The sections were then washed with PBS and incubated with rabbit
polyclonal anti-Ki-67 antibody (1:50; E0468, Dako, Glostrup,
Denmark) for 30 min at room temperature. After washing with PBS,
the sections were incubated with rat anti-IgG antibody (1:100;
sc-372; Vector Laboratories, Inc., Burlingame, CA, USA) for 30 min
at room temperature. The slides were washed with PBS and stained
using the ABC method (PK-4000; Vector Laboratories, Inc.) for 30
min.
For TUNEL staining, tissue sections (3 μm) on glass
slides were deparaffinized, washed with ethanol and water, and
soaked in diluted water. TUNEL staining was performed using the
In situ Apoptosis Detection kit (Takara Bio, Inc., Shiga,
Japan) according to the manufacturer’s instructions. Ten high-power
fields were randomly selected and the positive cells were
counted.
Image analysis of Ki-67 staining
Quantitative digital morphometric analysis of the
Ki-67-positive area was performed. Ten randomly-selected high-power
fields (magnification, ×200) were photographed for each cross
section using a digital camera attached to an Olympus microscope
system (Olympus Corporation, Tokyo, Japan). The color wavelengths
of the copied images were transformed into digital readings using
Lumina Vision software (Mitani Corporation, Tokyo, Japan), allowing
for quantification of the various color wavelengths with pixels as
the unit of measurement. The percentage of positive areas in the
tumor tissues was calculated by dividing the total pixel area of
the positive areas by the total pixel area corresponding to the
entire tumor tissue in the field of view. The tumor tissues of
three mice were analyzed in each group. The mean scores for 30
fields were used to determine the percentage of positive areas for
each group.
Statistical analysis
Data are expressed as the mean ± standard error of
the mean. Statistical analyses were performed using one-way
analysis of variance followed by the Tukey-Kramer test or the
Steel-Dwass test. P<0.05 was considered to indicate a
statistically significant difference.
Results
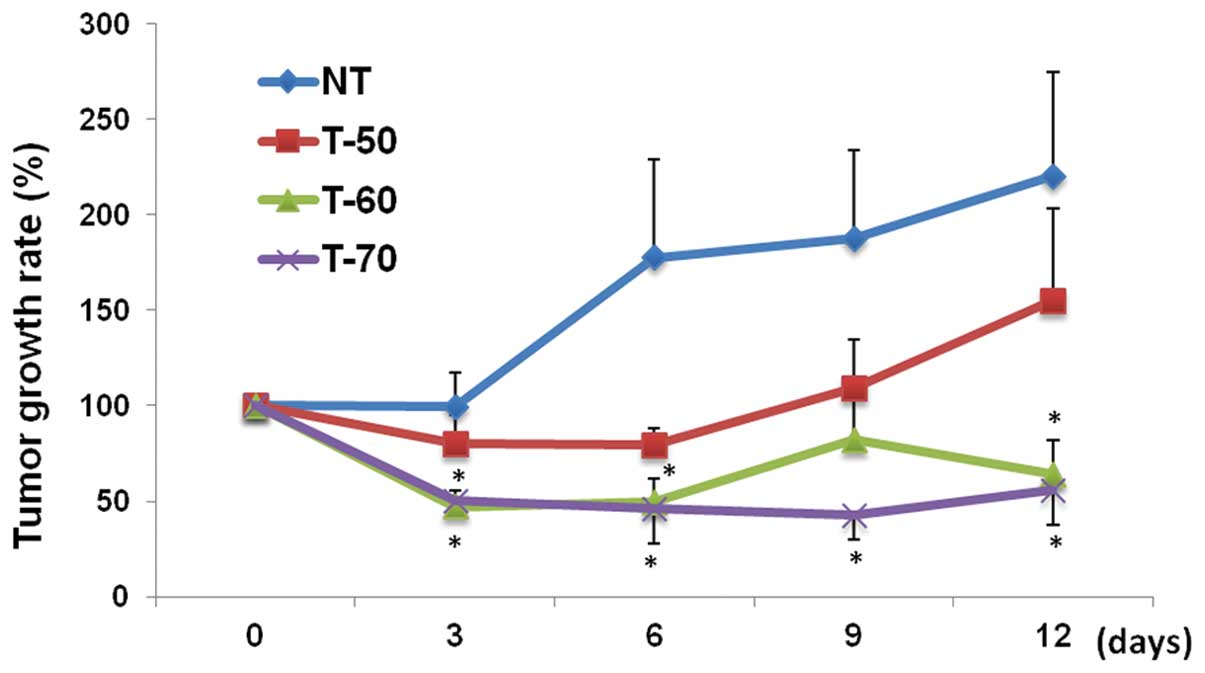
Tumor growth rates
The tumor growth rates of the various groups are
shown in Fig. 1. The tumor growth
rates were significantly lower in the T-70 group than those in the
NT group on days 3, 6, 9 and 12 (P<0.05). The tumor growth rates
were significantly lower in the T-60 group than those in the NT
group on days 3, 6 and 12. The tumor growth rates were slightly,
but insignificantly, lower in the T-50 group than those in the NT
group. The tumor growth rates were also lower in the T-70 and T-60
groups than those in the T-50 group on days 3, 6, 9 and 12. The
tumor growth rates in the T-60 and T-70 groups were similar on days
3, 6 and 12.
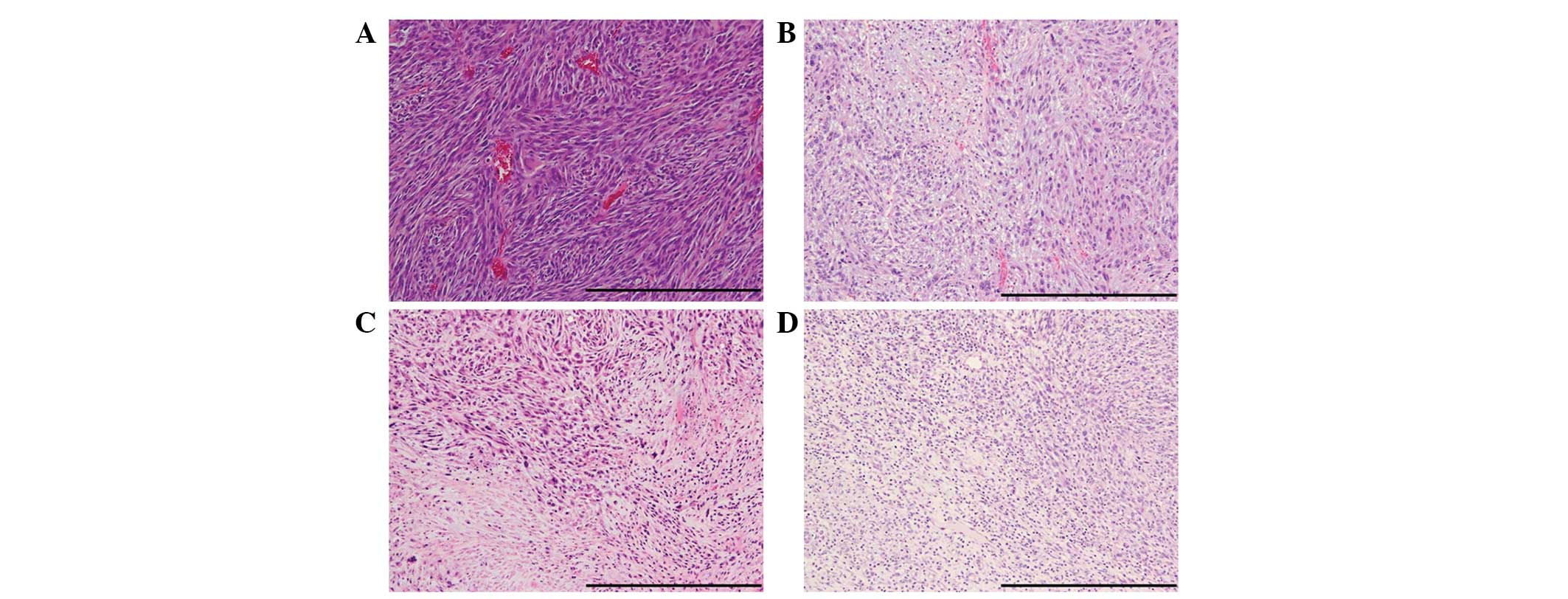
Histological evaluation
The results of HE staining are shown in Fig. 2. In the NT group, active cell
proliferation was frequently observed. Cell proliferation was
markedly suppressed in the T-70 and T-60 groups compared with that
in the NT group. In addition, in the T-70 and T-60 groups, necrotic
cells were widely observed. Cell proliferation was slightly
suppressed in the T-50 group compared with that in the NT group,
and only a few necrotic cells were observed.
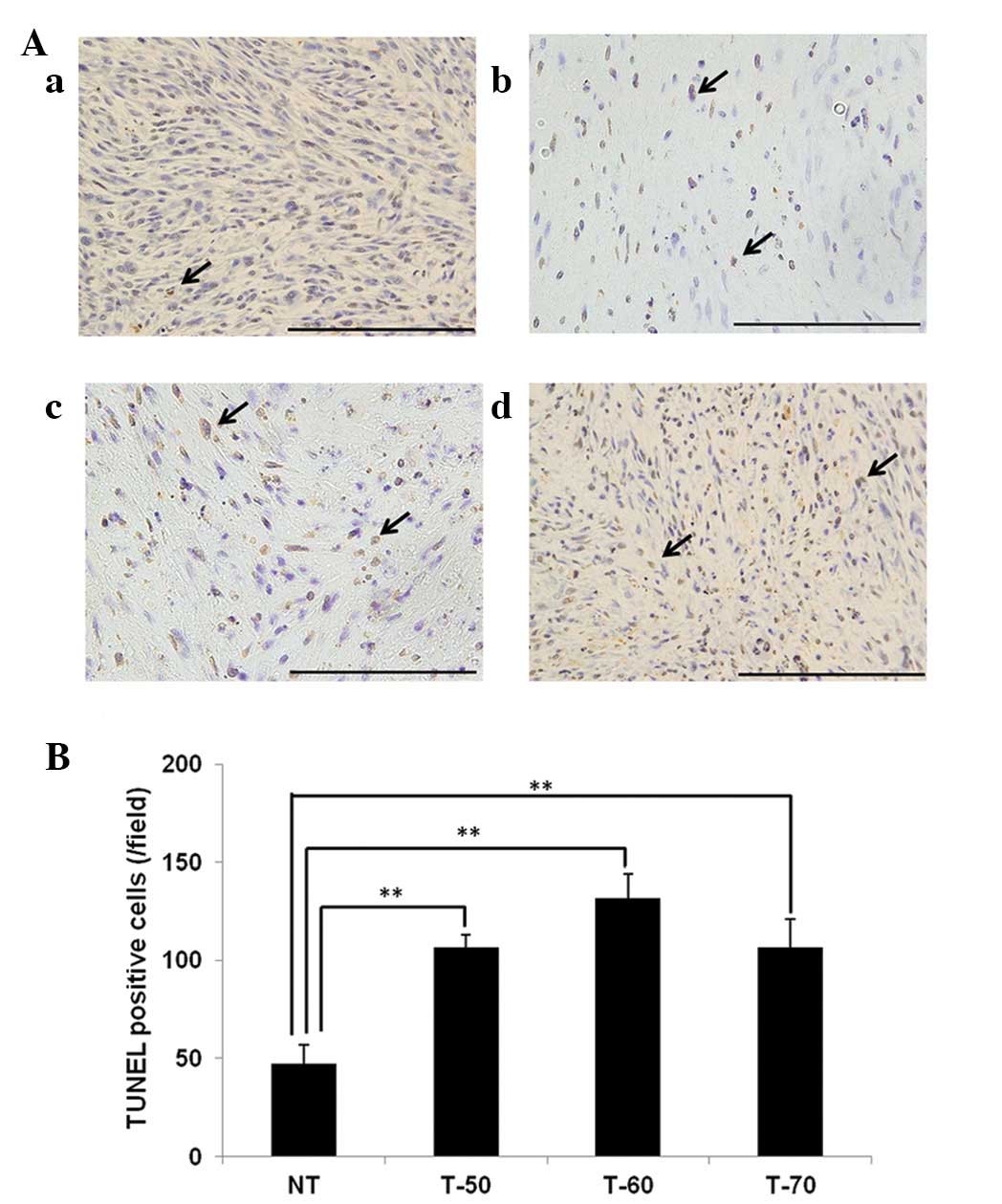
TUNEL staining
The results of TUNEL staining are shown in Fig. 3A. The TUNEL-positive cells are
denoted by arrows. The numbers of TUNEL-positive cells were
significantly higher in the T-70 (106.1±14.2 cells/field), T-60
(131.4±12.4 cells/field) and T-50 groups (106.7±6.7 cells/field)
than those in the NT group (47.1±9.5 cells/field) (P<0.01)
(Fig. 3B).
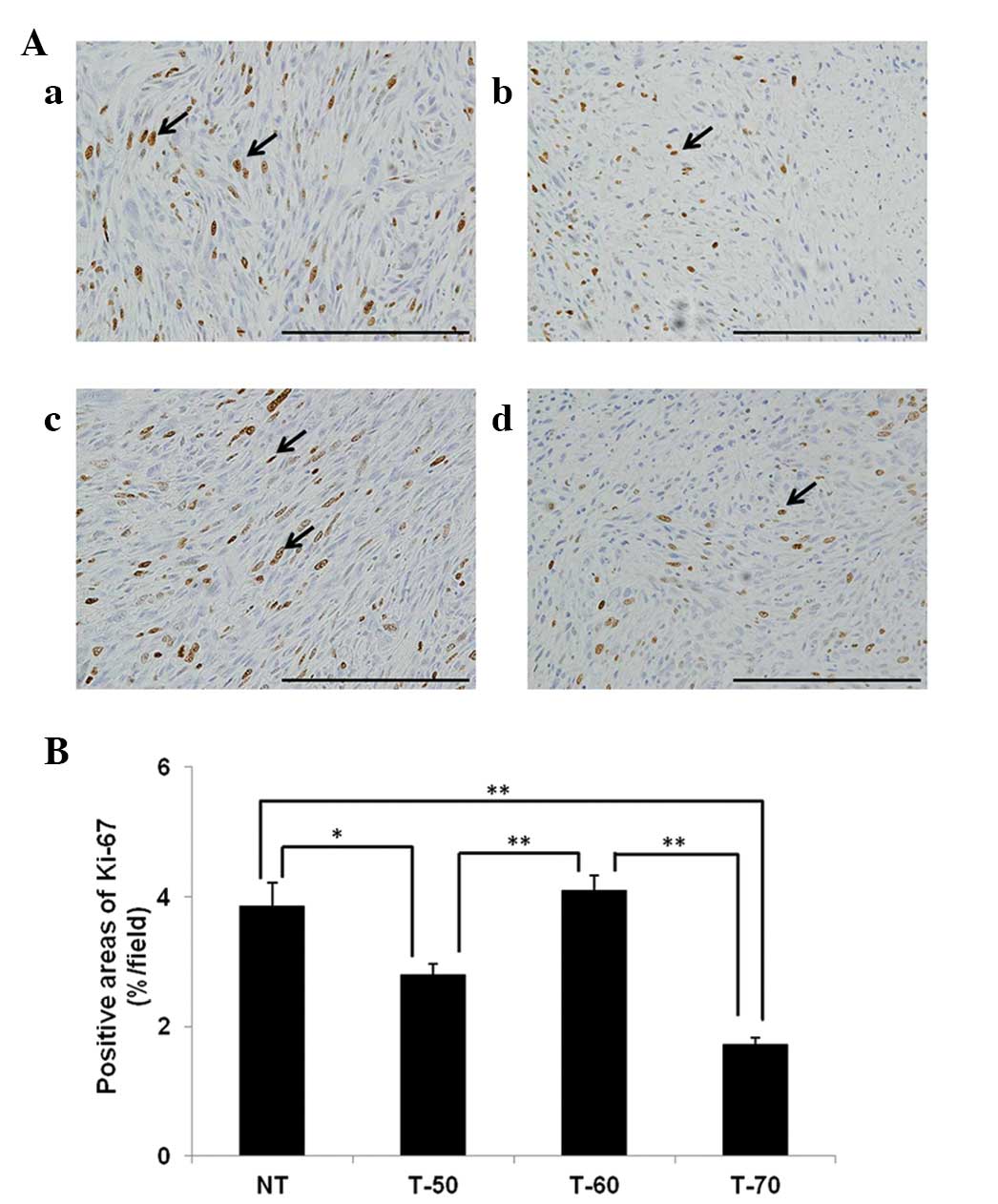
Ki-67 staining
The results of Ki-67 stains are shown in Fig. 4A. Ki-67-positive areas are denoted
by arrows. The Ki-67-positive area was significantly smaller in the
T-70 group (1.7±0.1%/field) than that in the NT (3.9±0.4%/field)
and T-60 groups (4.1±0.2%/field) (P<0.01). The Ki-67-positive
area was significantly smaller in the T-50 group (2.8±0.2 %/field)
than in the NT and T-60 groups (P<0.05, vs. NT; P<0.01 vs.
T-60) (Fig. 4B).
Discussion
In the present study, the antitumor effects of HTH
were evaluated using a glioma rat model. HTH at 60 and 70°C
significantly suppressed tumor growth. Previously, specific reports
indicated that HTH has potency as a treatment for melanoma in
experimental models (23,24). Li et al (24) previously described that local HTH
(≥50°C) inhibited tumor growth and stimulated a favorable antitumor
immune response in a malignant melanoma model. However, the authors
did not investigate the correlation between higher temperatures
(>60°C) and antitumor effects.
Studies of hyperthermia have focused on two commonly
applied strategies, conventional hyperthermia at mild temperatures
(42–45°C) (1,20,21)
and ablation therapy at high temperatures (>70°C) (22). To the best of our knowledge, no
study has examined the difference in antitumor effects between mild
(42–45°C) and high temperatures (>70°C) under the same
conditions as performed in the present study. Necrotic cells were
more commonly observed in the T-60 and T-70 groups than in the NT
groups. Previous reports indicated that HTH directly induced cell
damage and necrosis (6,7). In the T-50, T-60 and T-70 groups in
the present study, the numbers of TUNEL-positive cells in tumor
tissues were significantly increased compared with those in the NT
group. This finding indicates that relatively low temperatures
induce apoptosis (15). Our data
also indicate that HTH at 50–70°C induces necrosis and apoptosis in
a glioma rat model.
Ki-67 is a cell proliferation marker that is
detected during all active phases of the cell cycle, but is absent
in resting cells (25). Ki-67
expression increases during S phase until mitosis, when its
expression is maximal. Following cell division, cells in G1 phase
exhibit decreased Ki-67 expression until they reenter the S phase
when the level of Ki-67 increases again (26). Ki-67 expression is also useful for
diagnosing and assessing the grade of tumors in the central nervous
system (27). The Ki-67-positive
areas were significantly smaller in the T-50 and T-70 groups than
in the NT groups. Our data also indicate that temperatures
exceeding 70°C sufficiently suppress cell proliferation. Following
suppression of cell proliferation, apoptosis may be induced in
circumferential areas. The Ki-67-positive area was significantly
smaller in the T-70 group than that in the T-60 group, although the
tumor growth rates in these groups were equally decreased. We
cannot explain this difference, however, one possible explanation
may be that there are differences in the percentages of apoptotic
cells, as the T-60 group had significantly more TUNEL-positive
cells than the other groups. HTH at 60°C may suppress tumor growth
by inducing apoptosis more significantly than HTH at other
temperatures. Further studies, including those of other molecules
associated with apoptosis, are required to clarify this point.
In conclusion, HTH at temperatures exceeding 60°C
suppressed tumor growth in a glioma-bearing rat model. In addition,
HTH at 50–70°C induced necrosis and apoptosis in a glioma rat
model. Further studies is required to clarify the differences in
the mechanisms of action for HTH at 60 and 70°C.
References
|
1
|
Soares PI, Ferreira IM, Igreja RA, Novo CM
and Borges JP: Application of hyperthermia for cancer treatment:
recent patents review. Recent Pat Anticancer Drug Discov. 7:64–73.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wust P, Hildebrandt B, Sreenivasa G, Rau
B, Gellermann J, Riess H, Felix R and Schlag PM: Hyperthermia in
combined treatment of cancer. Lancet Oncol. 3:487–497. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Falk MH and Issels RD: Hyperthermia in
oncology. Int J Hyperthermia. 17:1–18. 2001. View Article : Google Scholar
|
|
4
|
Ross MI: Current status of hyperthermic
limb perfusion for in-transit melanoma. Int J Hyperthermia.
24:205–217. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pennacchioli E, Fiore M and Gronchi A:
Hyperthermia as an adjunctive treatment for soft-tissue sarcoma.
Expert Rev Anticancer Ther. 9:199–210. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Harmon BV, Takano YS, Winterford CM and
Gobé GC: The role of apoptosis in the response of cells and tumours
to mild hyperthermia. Int J Radiat Biol. 59:489–501. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Horsman MR: Tissue physiology and the
response to heat. Int J Hyperthermia. 22:197–203. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Diederich CJ: Thermal ablation and
high-temperature thermal therapy: overview of technology and
clinical implementation. Int J Hyperthermia. 21:745–753. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Roti Roti JL: Cellular responses to
hyperthermia (40–46 degrees C): cell killing and molecular events.
Int J Hyperthermia. 24:3–15. 2008.
|
|
10
|
den Brok MH, Sutmuller RP, van der Voort
R, Bennink EJ, Figdor CG, Ruers TJ and Adema GJ: In situ tumor
ablation creates an antigen source for the generation of antitumor
immunity. Cancer Res. 64:4024–4029. 2004.
|
|
11
|
Baronzio G, Gramaglia A and Fiorentini G:
Hyperthermia and immunity. A brief overview. In Vivo. 20:689–695.
2006.
|
|
12
|
Zerbini A, Pilli M, Penna A, Pelosi G,
Schianchi C, Molinari A, Schivazappa S, Zibera C, Fagnoni FF,
Ferrari C and Missale G: Radiofrequency thermal ablation of
hepatocellular carcinoma liver nodules can activate and enhance
tumor-specific T-cell responses. Cancer Res. 66:1139–1146. 2006.
View Article : Google Scholar
|
|
13
|
Mukhopadhaya A, Mendecki J, Dong X, Liu L,
Kalnicki S, Garg M, Alfieri A and Guha C: Localized hyperthermia
combined with intratumoral dendritic cells induces systemic
antitumor immunity. Cancer Res. 67:7798–7806. 2007. View Article : Google Scholar
|
|
14
|
Zhang HG, Mehta K, Cohen P and Guha C:
Hyperthermia on immune regulation: a temperature’s story. Cancer
Lett. 271:191–204. 2008.
|
|
15
|
Moroz P, Jones SK and Gray BN:
Magnetically mediated hyperthermia: current status and future
directions. Int J Hyperthermia. 18:267–284. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rees JH: Diagnosis and treatment in
neuro-oncology: an oncological perspective. Br J Radiol.
84:S82–S89. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fiorentini G, Giovanis P, Rossi S, Dentico
P, Paola R, Turrisi G and Bernardeschi P: A phase II clinical study
on relapsed malignant gliomas treated with electro-hyperthermia. In
Vivo. 20:721–724. 2006.PubMed/NCBI
|
|
18
|
Bidwell GL 3rd, Perkins E, Hughes J, Khan
M, James JR and Raucher D: Thermally targeted delivery of a c-Myc
inhibitory polypeptide inhibits tumor progression and extends
survival in a rat glioma model. PLoS One. 8:e551042013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang DC, Zhang Y, Chen HY, Li XL, Qin LJ,
Li YJ, Zhang HY and Wang S: Hyperthermia promotes apoptosis and
suppresses invasion in C6 rat glioma cells. Asian Pac J Cancer
Prev. 13:3239–3245. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Stojkovic R and Radacic M: Cell killing of
melanoma B16 in vivo by hyperthermia and cytotoxins. Int J
Hyperthermia. 18:62–71. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ito A, Fujioka M, Yoshida T, et al:
4-S-Cysteaminylphenol-loaded magnetite cationic liposomes for
combination therapy of hyperthermia with chemotherapy against
malignant melanoma. Cancer Sci. 98:424–430. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Haen SP, Pereira PL, Salih HR, Rammensee
HG and Gouttefangeas C: More than just tumor destruction:
immunomodulation by thermal ablation of cancer. Clin Dev Immunol.
1602502011.
|
|
23
|
Xia QS, Liu X, Xu B, Zhao TD, Li HY, Chen
ZH, Xiang Q, Geng CY, Pan L, Hu RL, et al: Feasibility study of
high-temperature thermoseed inductive hyperthermia in melanoma
treatment. Oncol Rep. 25:953–962. 2011.PubMed/NCBI
|
|
24
|
Li DY, Tang YP, Zhao LY, Geng CY and Tang
JT: Antitumor effect and immune response induced by local
hyperthermia in B16 murine melanoma: Effect of thermal dose. Oncol
Lett. 4:711–718. 2012.PubMed/NCBI
|
|
25
|
Brown DC and Gatter KC: Ki67 protein: the
immaculate deception? Histopathology. 40:2–11. 2002. View Article : Google Scholar
|
|
26
|
Lopez F, Belloc F, Lacombe F, Dumain P,
Reiffers J, Bernard P and Boisseau MR: Modalities of synthesis of
Ki67 antigen during the stimulation of lymphocytes. Cytometry.
12:42–49. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Prayson RA: The utility of MIB-1/Ki-67
immunostaining in the evaluation of central nervous system
neoplasms. Adv Anat Pathol. 12:144–148. 2005. View Article : Google Scholar
|