Introduction
Primary thyroid leiomyosarcoma (TL) represents just
0.014% of primary thyroid cancers (1) and is associated with an extremely
aggressive clinical course, leading to an extremely poor 5-year
survival rate. According to the World Health Organization’s
histological classification of thyroid and parathyroid tumors,
smooth muscle tumors can be either benign (leiomyoma) or malignant
(leiomyosarcoma) (2). Primary TL is
a mesenchymal malignant tumor with smooth muscle differentiation,
arising from the smooth muscle cells of the vessels located in the
thyroid capsule (1). Pathological
examination may be ineffective in distinguishing primary from
metastatic TL and clinical examination and instrumental diagnostic
work-up are required. Soft tissues, gastrointestinal tract and
particularly pelvic organs represent the most common sites of
origin (3). Cytological evaluation
reveals spindle cells, which may also be present in other more
common primary tumors of the thyroid gland, such as medullary or
anaplastic thyroid cancer (4).
Therefore, as in the reported case, preoperative fine needle
aspiration biopsy (FNAB) diagnosis can be extremely hard. According
to our knowledge, only 19 cases of TL, not responding to any
therapeutic approach, associated with a dismal prognosis have been
described (3). We present
cytohistopathological patterns and the clinical course of a patient
affected by TL. A literature analysis was performed using a PubMed
data base search, using keywords thyroid leiomyosarcoma and thyroid
smooth cell tumor. Incidence, diagnostic work-up, management and
most recent drug protocols were evaluated in order to provide the
latest results about this issue. Written informed consent was
obtained from the patient.
Case report
Case presentation and diagnosis
In June 2012, a 77-year-old male was admitted to the
Department of Anaesthesiology, Surgical and Emergency Science VII
Division of General Surgery, Second University of Naples (Naples,
Italy) with a clinical history of a recently arisen neck mass,
resulting in dysphagia and dyspnea. Thyroid-stimulating hormone,
calcitonin, thyroglobulin and carcinoembryonic antigen levels were
in the normal range. Ultrasound examination revealed a hypoechoic
nodular lesion of the right lobe of the thyroid gland, with
irregular margins and a central cystic area (39.6×35.3×34.1 mm)
confirmed by a contrast medium computed tomography (CT) scan
(Fig. 1); bilateral multiple
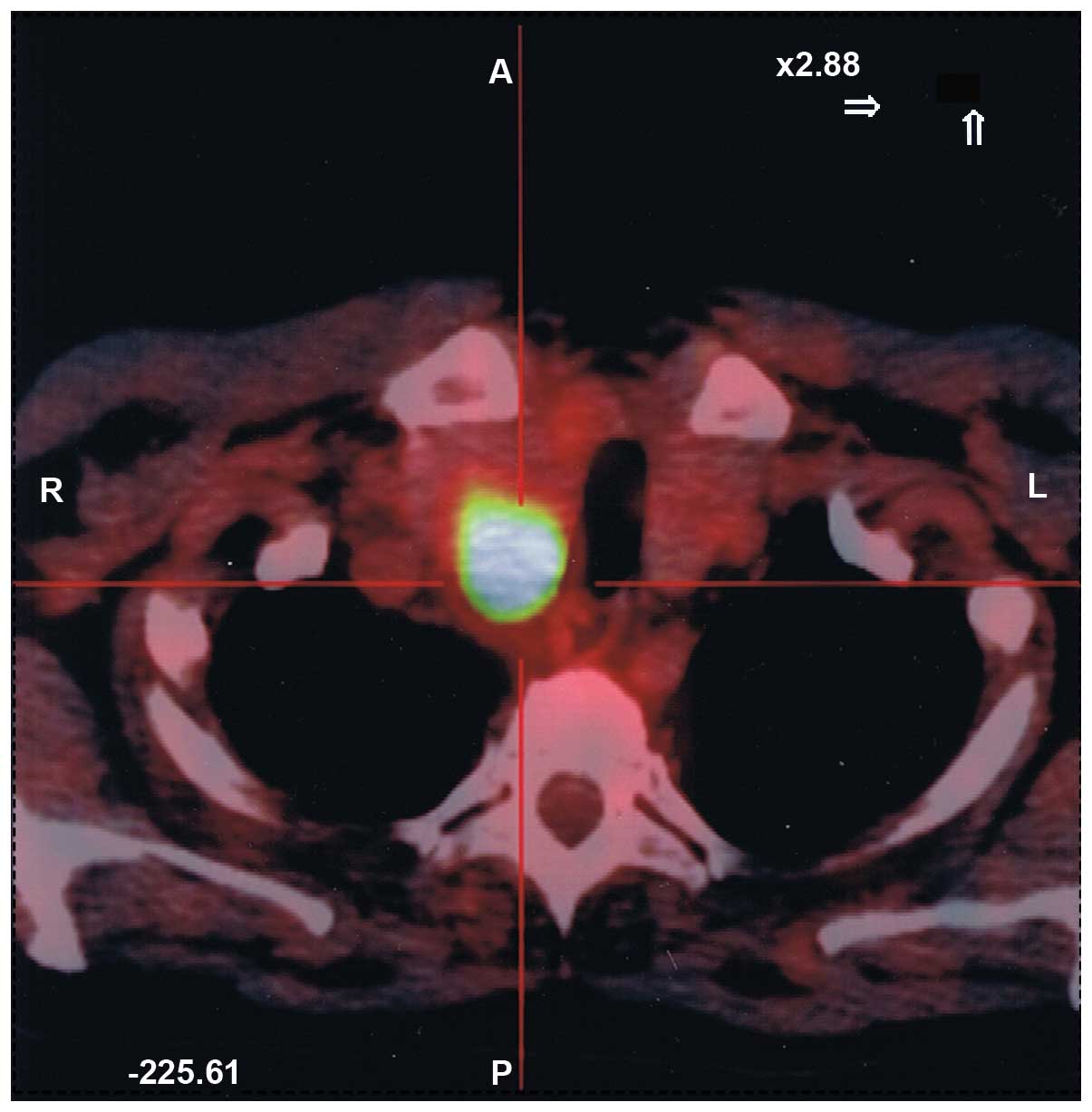
pulmonary lesions were also identified. A positron emission
tomography scan showed a heterogeneous uptake in the right lobe of
the thyroid (SUV 10.6) and in the two pulmonary fields (SUV
5.0–8.0) (Fig. 2). A FNAB revealed
isolated and clustered spindle cells with an epithelioid
aspect.
Surgery and follow-up
The postoperative course following a total
thyroidectomy (TT) was uneventful and the patient was discharged on
day 3. Adjuvant postoperative therapy was not performed due to the
poor general clinical conditions. The patient succumbed 40 days
after surgery, due to respiratory distress.
Cytopathological and histopathological
findings
FNAB was performed using a 25-mm/23G needle
connected to a 10-ml plastic syringe connected to a Cameco holder.
Several slides were obtained, which were either wet-fixed in 95%
ethanol or air-dried and stained, respectively, with Papanicolaou,
May-Grumwald Giemsa and alkaline Congo Red stains.
Cytological smears showed plump spindle cells with
elongated, blunt-ended nuclei and acidophilic, fibrillary
cytoplasm; these cells were isolated or in clusters, in a
proteinaceous and necrotic background. There were also isolated
cells with abundant eosinophilic cytoplasm and epithelioid
features. These features were highly suspected for a malignancy of
mesenchymal origin.
Grossly, the tumor originated within the right lobe
of the thyroid gland and measured 4.5–6.5 cm in the greatest
diameter. The mass was mainly solid, with areas of fresh tumor
necrosis, hemorrhage and cystic degeneration, and was not
well-circumscribed.
The histological pattern of growth was predominantly
solid, with clusters of epithelioid cells mixed with areas of
spindle-shaped and pleomorphic cells. These clusters were
interspersed with areas of marked sclerosis and with large areas of
coagulative necrosis and hemorrhage. The single cells showed
considerable variation in nuclear size, shape and morphology;
however, the majority of neoplastic cells presented hyperchromatic
nuclei and abundant eosinophilic cytoplasm that showed focal,
irregular, intracytoplasmic vacuoles. A distinct fibrillarity was
present within the cytoplasm of a number of cells. The mitotic rate
was extremely high (25 mitosis/10 high-power field), and atypical
mitotic figures were also present. The neoplasia showed invasion of
the periglandular fat tissue.
Immunohistochemical staining showed diffused and
marked reactivity with vimentin and H-caldesmon, and focally, with
smooth muscle actin and specific muscle actin. No reactivity was
shown for all keratins tested (pan-cytokeratin AE1-AE3, CK7, CK19,
CK5/6 and CK8/18), EMA, TTF-1, thyroglobulin and for the
endothelial markers, CD31 and factor VIII.
Morphological and immunophenotypic features were
suggestive of a malignant neoplasia with mesenchymal origin, such
as a primary leiomyosarcoma of the thyroid gland.
Discussion
Papillary and follicular variants are the most
frequent thyroid neoplasms, followed by medullary cancers, often
part of multiple endocrine neoplasia type 2 (5–8).
Extremely rare and aggressive, anaplastic carcinoma, considered a
fatal tumor, is associated with a poor survival rate, as reported
for sarcomatoid carcinoma of other origins (9). In the last 10 years,
ultrasonography-guided FNAB has allowed a more precocious diagnosis
(10,11). Primary TL, an extremely rare
neoplasm, may originate from smooth muscle cells of the capsula
vessels. Metaplasia from a previously existing thyroid anaplastic
carcinoma should be considered (1,12,13).
At the time of first diagnosis, TL is frequently associated with
distant metastases. It is a fatal tumor with a 1-year survival rate
of <20%. Grossly, TL are large fleshy white-gray masses, with
foci of fresh tumor necrosis and hemorrhage, and a tendency for
cystic degeneration. Microscopically, the pattern of growth is
usually fascicular, with tumor bundles intersecting each other.
Certain tumors also present areas with a whorled appearance. The
individual neoplastic cells are elongated, with abundant
acidophilic fibrillary cytoplasm; the nucleus is generally
centrally located and typically blunt-ended or ‘cigar-shaped’.
These features also appear on cytological samples. The degree of
nuclear atypia is highly variable and the mitotic activity varies
considerably. High mitotic activity is virtually diagnostic of
malignancy, although a TL must be strongly suspected for a tumor
that is widely necrotic, hemorrhagic and with significant atypia,
even if the mitotic index is low.
Immunohistochemically, TL show reactivity for
vimentin, smooth muscle actin, muscle-specific actin, smooth muscle
myosin, desmin, H-caldesmon and basal lamina components, including
laminin and type IV collagen. H-caldesmon is a muscle marker used
to discriminate between smooth muscle cells and myofibroblasts;
this marker appears to be associated with the degree of
differentiation. Other antigens sporadically identified in TL are
S-100 protein, estrogen and progesterone receptor proteins, raising
the possibility of hormonal responsiveness (14).
In our referral endocrine surgery center, 250–300
thyroidectomies are performed per year. One case of primary TL has
been observed in the last 33 years. To our knowledge, only 19 cases
have been described so far in the international literature, making
the present case the twentieth reported case of primary TL
(3). In the majority of cases,
patients are generally female in their sixth and seventh decades
(15) and complaining of local
compressive symptoms, in addition to neck pain and tenderness.
Differential diagnosis includes anaplastic or medullary thyroid
carcinoma, solitary fibrous tumor and spindle epithelial tumor with
thymus-like differentiation (SETTLE), due to the presence in each
variant of spindle cell elements.
The majority of anaplastic (undifferentiated)
thyroid tumors show ‘sarcoma-like’ features, with spindle-shaped
neoplastic cells arranged in a fascicular or whorled pattern of
growth. Immunohistochemical stains for keratins, expressed in
50–100% of cases, confirm the epithelial nature of the tumor.
Medullary thyroid carcinoma cells may be spindle-shaped; however,
immunohistochemically, they are reactive for keratins, thyroid
transcription factor-1 (thyroglobulin-negative), neuron-specific
enolase, chromogranin (A, B and C), synaptophysin, opioid peptides
and calcitonin. SETTLE, occurring in children and adolescents, is a
rare tumor usually located in the thyroid gland and perithyroid
tissue. Histologically, it is a biphasic neoplasm composed of
spindle cells admixed with epithelial structures, generally without
atypia.
TL preoperative diagnosis can be extremely
difficult. It is important to discriminate between primary TL and
‘non-thyroid’ cervical leiomyosarcoma (1% of head and neck sarcoma)
and, furthermore, exclude a metastatic origin from stomach, pelvis
and soft tissue (16). CT scan and
magnetic resonance imaging are useful for defining the local extent
of disease and for identifying distant metastases. To date, it is
not clear whether therapy is effective in prolonging survival, as
demonstrated in 19 reported cases (3). Rapid locoregional infiltration and
diffuse brain or lung metastases are responsible for the high
mortality rate. Total or near-total thyroidectomy, for the majority
of thyroid pathologies, associated with therapeutic modified
radical neck dissection should be considered for intrathyroidal
disease (17–21). Chemotherapy has not shown any
therapeutic efficacy. Wang et al and Raspollini et al
reported interesting data in the management of thyroid and uterus
leiomyosarcomas through the overexpression of c-Kit proto-oncogene,
a tyrosine kinase receptor (4,22).
However, the use of imatinib mesylate (tyrosine kinase inhibitor)
did not prevent the relapse and the fatal outcome in one patient
with TL associated with lung metastases (23). In the case of locoregional
infiltrating disease, surgery may be performed to prevent airway or
esophageal obstruction. Often, therapies do not produce any
clinical benefit, only palliative results.
TL remains a fatal tumor, invariably associated with
a dismal prognosis, and, although notable improvements in oncology,
an efficacious multimodal treatment protocol is lacking. To modify
the poor surgical outcomes, novel and effective adjuvant
therapeutic strategies, based on a molecular approach, are
required.
References
|
1
|
Thompson LD, Wenig BM, Adair CF, Shmookler
BM and Heffess CS: Primary smooth muscle tumors of the thyroid
gland. Cancer. 79:579–587. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
DeLellis RA, Lloyd VR, Heitz PU and Eng C:
World Health Organization Classification of Tumours: Pathology and
Genetics of Tumours of Endocrine Organs. IARC Press; Lyon: 2004
|
|
3
|
Amal B, El Fatemi H, Souaf I, Moumna K and
Affaf A: A rare primary tumor of the thyroid gland: report a new
case of leiomyosarcoma and literature review. Diagn Pathol.
8:362013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pezzolla A, Docimo G, Ruggiero R, et al:
Incidental thyroid carcinoma: a multicentric experience. Recenti
Prog Med. 101:194–198. 2010.(In Italian).
|
|
5
|
Pasquali D, Santoro A, Bufo P, et al:
Upregulation of endocrine gland-derived vascular endothelial growth
factor in papillary thyroid cancers displaying infiltrative
patterns, lymph node metastases, and Braf mutation. Thyroid.
21:391–399. 2011. View Article : Google Scholar
|
|
6
|
Conzo G, Circelli L, Pasquali D, et al:
Lessons to be learned from the clinical management of a MEN 2A
patient bearing a novel 634/640/700 triple mutation of the RET
proto-oncogene. Clin Endocrinol (Oxf). 77:934–936. 2012. View Article : Google Scholar
|
|
7
|
Conzo G, Musella M, Corcione F, De Palma
M, Ferraro F, Palazzo A, et al: Laparoscopic adrenalectomy, a safe
procedure for pheochromocytoma. A retrospective review of clinical
series. Int J Surg. 11:152–156. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Di Vizio D, Insabato L, Conzo G, et al:
Sarcomatoid carcinoma of the colon: a case report with literature
review. Tumori. 87:431–435. 2001.PubMed/NCBI
|
|
9
|
Conzo G, Troncone G, Docimo G, et al:
Cytologically undetermined follicular lesions: surgical procedures
and histological outcome in 472 cases. Ann Ital Chir. 84:251–256.
2012.
|
|
10
|
Troncone G, Volante M, Iaccarino A, et al:
Cyclin D1 and D3 overexpression predicts malignant behavior in
thyroid fine-needle aspirates suspicious for Hurtle cell neoplasms.
Cancer Cytopathol. 117:522–529. 2009.
|
|
11
|
Adachi M, Wellman KF and Garcia R:
Metastatic leiomyosarcoma in brain and heart. J Pathol. 98:294–296.
1969. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chetty R, Clark SP and Dowling JP:
Leiomyosarcoma of the thyroid: immunohistochemical and
ultrastructural study. Pathology. 25:203–205. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tulbah A, Al-Dayel F, Fawaz I and Rosai J:
Epstein-Barr virus-associated leiomyosarcoma of the thyroid in a
child with congenital immunodeficiency: a case report. Am J Surg
Pathol. 23:473–476. 1999. View Article : Google Scholar
|
|
14
|
Iida Y, Katoh R, Yoshioka M, Oyama T and
Kawaoi A: Primary leiomyosarcoma of the thyroid gland. Acta Pathol
Jpn. 43:71–75. 1993.PubMed/NCBI
|
|
15
|
Deng XR, Wang G, Kuang CG, Peng GZ and
Chen RS: Metastasis of leiomyosarcoma to the thyroid. Chin Med J
(Engl). 118:174–176. 2005.PubMed/NCBI
|
|
16
|
Cirocchi R, Boselli C, Guarino S, et al:
Total thyroidectomy with ultrasonic dissector for cancer:
multicentric experience. World J Surg Oncol. 10:702012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
De Bellis A, Conzo G, Cennamo G, et al:
Time course of Graves’ ophthalmopathy after total thyroidectomy
alone or followed by radioiodine therapy: a 2-year longitudinal
study. Endocrine. 41:320–326. 2012.
|
|
18
|
Conzo G, Pasquali D, Bellastella G, et al:
Total thyroidectomy, without prophylactic central lymph node
dissection, in the treatment of differentiated thyroid cancer.
Clinical retrospective study on 221 cases. Endocrine. 44:419–425.
2013. View Article : Google Scholar
|
|
19
|
Docimo G, Ruggiero R, Subitosi A, Casalino
G, Bosco A, Gili S, Conzo G and Docimo L: Ultrasound scalpel
thyroidectomy: prospective randomized study. Ann Ital Chir.
83:491–496. 2012.PubMed/NCBI
|
|
20
|
Conzo G, Docimo G, Ruggiero R, Napolitano
S, Palazzo A, Gambardella C, Mauriello C, Tartaglia E, Cavallo F
and Santini L: Surgical treatment of papillary thyroid carcinoma
without lymph nodal involvement. G Chir. 33:339–342.
2012.PubMed/NCBI
|
|
21
|
Wang TS, Ocal IT, Oxley K and Sosa JA:
Primary leiomyosarcoma of the thyroid gland. Thyroid. 18:425–428.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Raspollini MR, Aminni G, Villanucci A,
Pinzani P, Simi L, Paglierani M and Taddei GL: C-kit overexpression
in patients with uterine leiomyosarcomas: a potential alternative
therapeutic treatment. Clin Cancer Res. 10:3500–3503. 2004.
View Article : Google Scholar
|
|
23
|
Day AS, Lou PJ, Lin WC and Chou CC:
Over-expression of c-kit in a primary leiomyosarcoma of the thyroid
gland. Eur Arch Otorhinolaryngol. 264:705–708. 2007. View Article : Google Scholar : PubMed/NCBI
|