Introduction
Malignant melanoma (MM) arising from the anorectal
region is rare, comprising only 0.4–1.6% of all melanomas and ~1%
of all anal canal tumors (1,2).
However, the anorectum is the third most common site for the
occurrence of primary MM, preceded only by the skin and eyes
(3). Occasionally, primary
anorectal (PA) MM is misdiagnosed as anorectal cancer, which is
attributed to a lack of immunohistochemical findings. As a result,
there is no consensus on the most effective therapeutic regimen for
PAMM. Preoperative concurrent chemoradiotherapy (CCRT) has been
widely used for the treatment of numerous malignant neoplastic
diseases, however, not in PAMM. The present case report proposes a
novel therapeutic regimen for PAMM by demonstrating a patient who
received preoperative CCRT and sphincter-sparing surgery. Patient
provided written informed consent.
Case report
A 55-year-old female patient experienced
intermittent hematochezia for one year. Digital rectal examination
revealed a hard cauliflower-shaped mass (size, 3.0×4.0 cm), located
1 cm from the anal verge, with bloodstains observed on the
finger-cot. The serum levels were as follows: Carcinoembryonic
antigen, 2.6 μg/l; carbohydrate antigen 19-9, 25.6 U/ml; and
lactate dehydrogenase, 180 U/l, which were all considered to be
within the normal ranges. Abdominal magnetic resonance imaging
(MRI) demonstrated a rectal mass (diameter, 4.2 cm), which had
invaded the anus and cervix, in addition, the lymph nodes of the
right pelvic cavity and right inguen were enlarged. Through
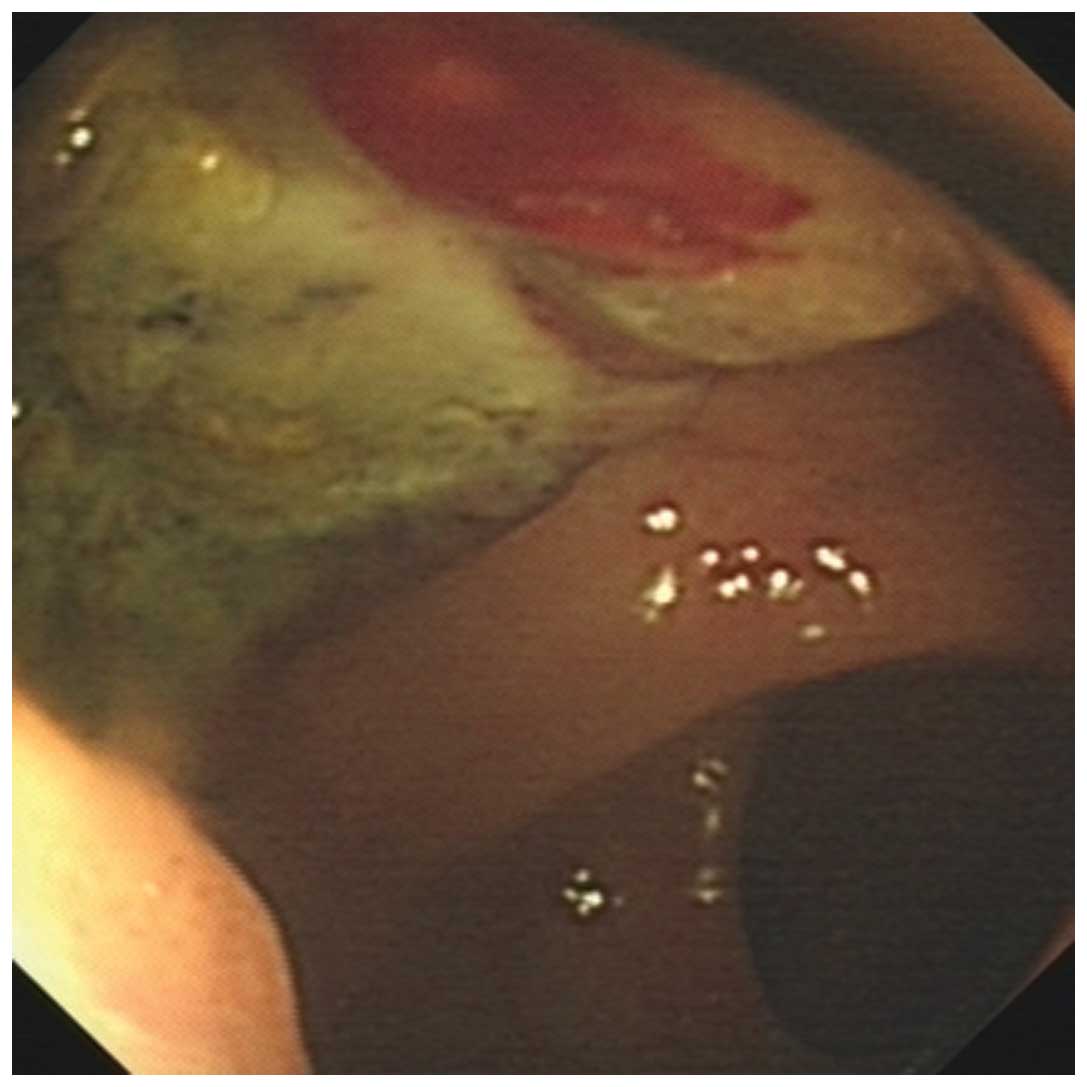
colonoscopy, a pigmented mass with a large ulcer was observed on
the anterior wall of the anorectum, ~4.0 cm in size (Fig. 1). The result of colonoscopy
pathology indicated low differentiated carcinoma, however,
immunohistochemical analysis was not performed. According to the
abovementioned findings, the preoperative diagnosis was a locally
advanced rectal carcinoma. In order to preserve sphincter function,
obtain pathological downstaging and reduce the rate of recurrence,
preoperative CCRT was adopted.
A total irradiation dose of 45.0 Gy was delivered in
daily fractions of 1.8 Gy, five times per week, through a pair of
opposed anterior-posterior fields using a 6-MV linear accelerator.
The treatment fields were set as follows; the superior border was
placed at S1, the inferior border was placed below the anus (~0.5
cm) and the lateral borders of the planning target volume were
1.5-cm lateral to the widest bony margin of the true pelvic wall.
Throughout the radiation period, capecitabine was administered
every 12 h, twice a day following a meal, at a dose of 1,000 mg for
two weeks. Administration of the medication subsequently ceased for
one week. Following this, the medication regimen was continued for
another two weeks. During the therapy, only grade 1 leukopenia
occurred and the treatment was well-tolerated by the patient, with
no regimen interruption.
A digital rectal examination, following CCRT,
revealed a hard cauliflower-shaped mass (size, 2.0×2.0 cm) without
any bloodstaining observed on the finger-cot. The computer
tomography scan demonstrated that the tumor had shrunk sharply
(diameter, 2.0 cm) and there were no enlarged lymph nodes.
The surgery was performed eight weeks following the
completion of CCRT. A cauliflower-shaped tumor (size, 2.0×2.0 cm),
which invaded the posterior wall of the vagina, was observed on the
antetheca of the anal region. However, the enlarged lymph nodes of
the right pelvic cavity and right inguen, which were observed in
the prior MRI scan, were no longer detected. The rectum, uterus,
bilateral accessory and posterior wall of the vagina were excised
during surgery. Finally, coloanal anastomosis and reconstruction of
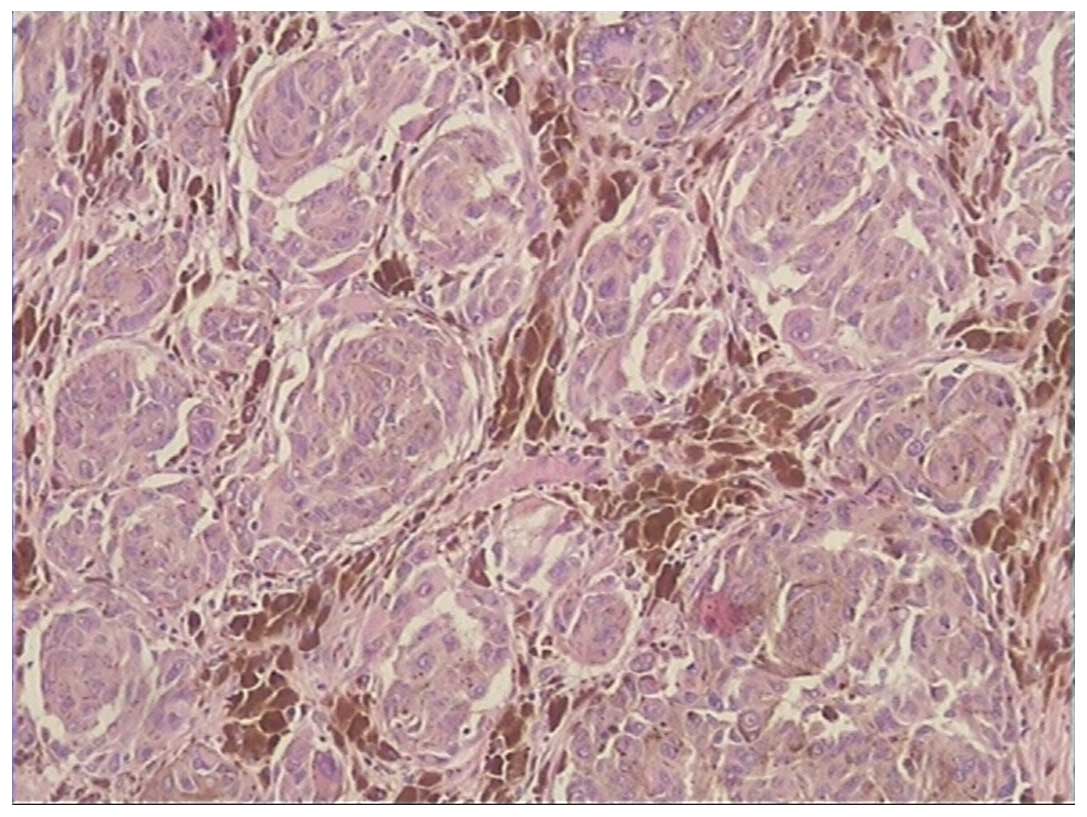
the vagina were performed. A histopathological examination
demonstrated cells, which exhibited marked cytological atypia,
pleomorphism and increased mitotic activity. Numerous melanin
granules were apparent between the tumor cells (Fig. 2). Immunohistochemical staining for
HMB-45 (weakly positive), Melan-A (positive), S-100 (weakly
positive) and VIM (weakly positive) confirmed the diagnosis of
PAMM. According to the American Joint Committee on Cancer
classification for melanoma (7th edition) (4), the postoperative stage was identified
as ypT2aN0M0, stage IB, while the initial stage was cT4bN2M0, stage
III. In addition, the resection margins were negative. There was no
complication following the surgery and the postoperative recovery
was good. The patient did not receive any subsequent adjuvant
therapy.
The patient underwent a close postoperative
follow-up for 15 months, without any evidence of local relapse,
lymphatic metastasis or distant metastasis. As a result of this
treatment strategy, the patient obtained complete remission with a
high quality of life. The only symptoms experienced by the patient
were pain from the incision for one month and occasional instances
of constipation in the six months following surgery. Recently, the
patient has not complained of any symptoms or signs. In the
postoperative follow-up period, the mean Karnofsky Performance
Scale (KPS) score was 90 and the most recent score was 100.
Discussion
MM is a neoplasm of neuroectodermal origin arising
from melanocytes. PAMM most commonly originates near the anorectal
junction, where melanocytes normally occur. Goldman et al
(5) reported 49 cases of PAMM, and
45 of those were located at, or near, the anorectal junction. As MM
arising from the anorectum was initially described by Moore in 1857
(6), a series of articles
describing PAMM have been published. The incidence remains
extremely low, ranging between <1 and 3% (7). In addition, PAMM is a malignant
disease with an exceptionally poor prognosis. The five-year
survival rate is only 9–16% (8,9), which
may be explained by the aggressive nature of the disease. A
previous study identified that 26% of patients had exhibited
distant metastasis at the time of diagnosis (10).
PAMM can easily be mistaken for certain other
lesions, including hemorrhoids, polyp and adenocarcinoma, and
misdiagnosis rates have been recorded as 58.2–86.4% (9,11,12).
There are several common causes for misdiagnosis in PAMM, including
i) the symptoms and signs of PAMM are not specific; ii)
non-pigmented lesions appear on endoscopic examination; iii)
immunohistochemical examination as a definite diagnosis approach is
not performed in every colonoscopy pathology; and iv) MM located on
the anorectum is rare, and inexperienced physicians lack the
vigilance and awareness of this disease.
In the present case, a pigmented mass was revealed
on the colonoscopy, however, the main cause of misdiagnosis was
that an immunohistochemical examination was not performed.
Misdiagnosis of PAMM may lead to a delay in treatment and distant
metastasis. In one study, the five-year survival rate of
misdiagnosed patients was 11%, compared with 25% that had been
diagnosed correctly (9).
As there is a low incidence of, and inexperience
with treating PAMM, the most appropriate treatment strategy remains
controversial. Surgery as a primary treatment strategy for PAMM,
ranges from abdominoperineal resection (APR) to wide local excision
(WLE). However, previous studies comparing the difference in
survival time of patients treated by APR or WLE identified no
statistical difference (10,13).
In a number of studies, adjuvant chemotherapy (14), adjuvant radiation (15), neoadjuvant radiation (16) and immunotherapies (17) have also been used in PAMM, and
certain curative effects were obtained. Preoperative CCRT has a
proven role in the treatment of various malignant diseases,
particularly in locally advanced rectal cancer (18). The predominant role of preoperative
CCRT is to reduce locoregional and pelvic cavity recurrence, and to
obtain a higher rate of sphincter preservation via tumor shrinkage.
In addition, it facilitates the removal of potential
micrometastasis and lessens distant metastases. In the present
case, preoperative CCRT was performed in PAMM and the patient
achieved a pathological partial response. Uner et al
(16) reported a case of PAMM; the
patient received radiation as the primary treatment rather than
surgery and exhibited a similar outcome, indicating that
neoadjuvant therapy may be beneficial to PAMM. The goal of therapy
for PAMM should be to maximize the survival time as well as to
improve quality of life. Preservation of sphincter function is,
therefore, emphasized in surgery. Following CCRT, a decrease in
tumor volume renders sphincter preservation feasible with negative
margins. The timing of surgery following CCRT should also be
considered. In the period following radiation therapy, tumor cells
may be eradicated continually, and the adequate time between CCRT
and surgery is 4–8 weeks (17).
KPS was a tool, developed as a subjective means of
evaluating a patient’s ability to perform ordinary tasks. It is a
clinical prognosis index of the cancer patient population. In the
current case, the patient exhibited a high KPS score following
surgery, which indicates a good prognosis.
In conclusion, PAMM remains a rare disease that is
associated with a poor prognosis. In order to improve the accuracy
of diagnosis, physicians must be vigilant to the occurrence of
PAMM, and immunohistochemistry should be a routine examination
during colonoscopy pathology. The most effective treatment
strategies for PAMM remain the focus of investigation. The
therapeutic regimen of neoadjuvant CCRT together with
sphincter-sparing surgery may guarantee a high quality of life and
provide high efficacy, indicating that it may be an optimal
strategy for patients with PAMM. Further studies are required to
further evaluate the efficacy of this therapeutic regimen.
References
|
1
|
Wanebo HJ, Woodruff JM, Farr GH and Quan
SH: Anorectal melanoma. Cancer. 47:1891–1900. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pack GT and Oropeza R: A comparative study
of melanoma and epidermoid carcinoma of the anal canal: A review of
20 melanomas and 29 epidermoid carcinomas (1930 to 1965). Dis Colon
Rectum. 10:161–176. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Weston SD and Marren M: Malignant melanoma
of the rectum. J Int Coll Surg. 17:403–416. 1952.PubMed/NCBI
|
|
4
|
Balch CM, Gershenwald JE, Soong SJ, et al:
Final version of 2009 AJCC melanoma staging and classification. J
Clin Oncol. 27:6199–6206. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Goldman S, Glimelius B and Påhlman L:
Anorectal malignant melanoma in Sweden. Report of 49 patients. Dis
Colon Rectum. 33:874–877. 1990. View Article : Google Scholar
|
|
6
|
Moore W: Recurrent melanoma of the rectum
after previous removal from the verge of the anus in a man aged
sixty-five. Lancet. 1:2901857.
|
|
7
|
Yap LB and Neary P: A comparison of wide
local excision with abdominoperineal resection in anorectal
melanoma. Melanoma Res. 14:147–150. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Konstadoulakis MM, Ricaniadis N, Walsh D
and Karakousis CP: Malignant melanoma of the anorectal region. J
Surg Oncol. 58:118–120. 1995. View Article : Google Scholar
|
|
9
|
Zhang S, Gao F and Wan D: Effect of
misdiagnosis on the prognosis of anorectal malignant melanoma. J
Cancer Res Clin Oncol. 136:1401–1405. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Thibault C, Sagar P, Nivatvongs S, Ilstrup
DM and Wolff BG: Anorectal melanoma - an incurable disease? Dis
Colon Rectum. 40:661–668. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhong J, Zhou JN, Xu FP and Shang JQ:
Diagnosis and treatment of anorectal malignant melanoma - a report
of 22 cases with literature review. Ai Zheng. 25:619–624. 2006.(In
Chinese).
|
|
12
|
Slingluff CL Jr, Vollmer RT and Seigler
HF: Anorectal melanoma: clinical characteristics and results of
surgical management in twenty-four patients. Surgery. 107:1–9.
1990.
|
|
13
|
Cooper PH, Mills SE and Allen MS Jr:
Malignant melanoma of the anus: report of 12 patients and analysis
of 255 additional cases. Dis Colon Rectum. 25:693–703. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Phade VR and Lawrence WR: Anorectal
melanoma. Br J Surg. 68:667–668. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ballo MT, Gershenwald JE, Zagars GK, et
al: Sphincter-sparing local excision and adjuvant radiation for
anal-rectal melanoma. J Clin Oncol. 20:4555–4558. 2002. View Article : Google Scholar
|
|
16
|
Uner A, Kilic D, Mentes BB, Egehan I and
Dursun A: Neoadjuvant radiotherapy in anorectal malignant melanoma.
Int J Clin Pract. 57:65–67. 2003.PubMed/NCBI
|
|
17
|
Morton DL, Hsueh EC, Essner R, et al:
Prolonged survival of patients receiving active immunotherapy with
Canvaxin therapeutic polyvalent vaccine after complete resection of
melanoma metastatic to regional lymph nodes. Ann Surg. 236:438–448.
2002. View Article : Google Scholar
|
|
18
|
Sanghera P, Wong DW, McConkey CC, Geh JI
and Hartley A: Chemoradiotherapy for rectal cancer: an updated
analysis of factors affecting pathological response. Clin Oncol (R
Coll Radiol). 20:176–183. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bujko K, Nowacki MP and Liszka-Dalecki P:
Radiation therapy for anorectal melanoma - a report of three cases.
Acta Oncol. 37:497–499. 1998. View Article : Google Scholar : PubMed/NCBI
|