Introduction
Postoperative spindle cell nodule (PSCN) of the
bladder is a rare non-neoplastic lesion of the bladder consisting
of a reactive proliferation of spindle cells. PSCN occurs between
several weeks or months following surgery at the site of surgical
intervention, such as transurethral resection or biopsy (1). Although PSCN resembles a sarcoma, it
has a favorable prognosis and conservative management is considered
a reasonable treatment option for the disease (2). The majority of the tumors of the
bladder are malignant, with transitional cell carcinoma being the
most common type of malignant tumor. However, other tumors may lead
to misdiagnosis. This report presents a case of PSCN of the bladder
and reviews the literature to summarize its characteristics and
assist in avoiding misdiagnosis and unnecessary treatment. Patient
provided written informed consent.
Case report
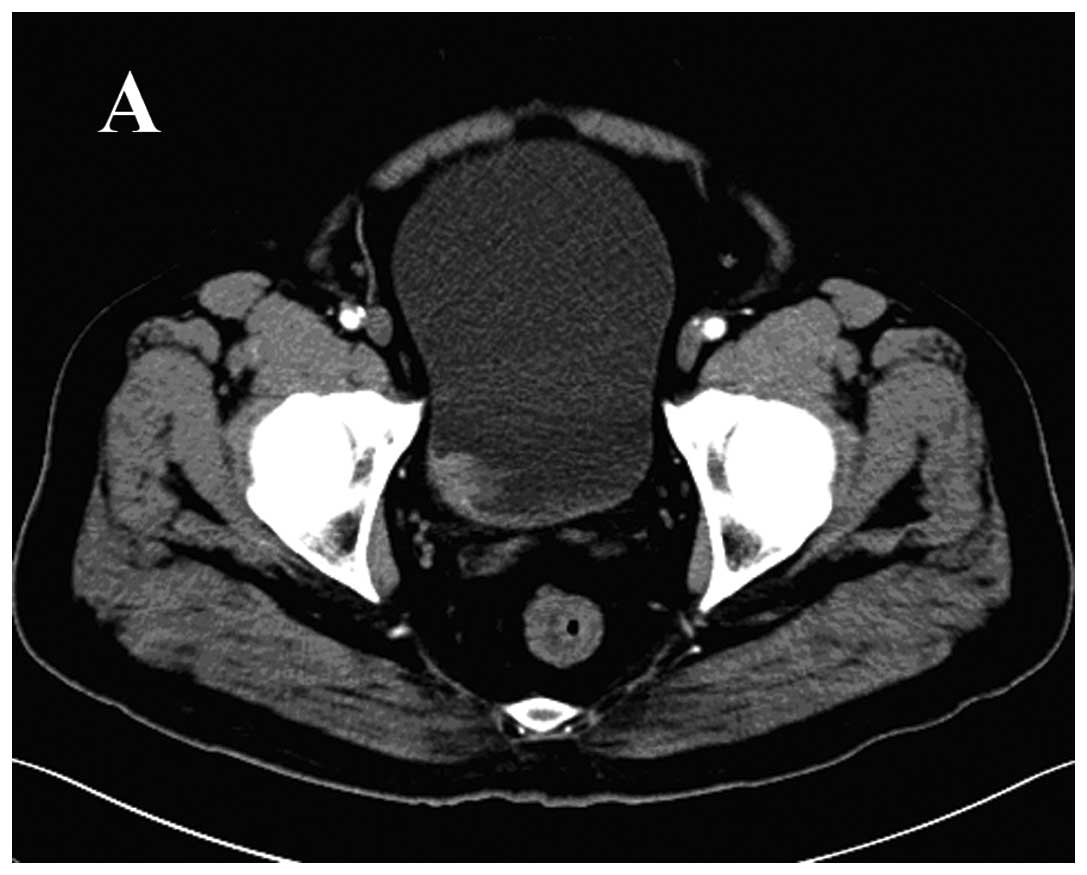
A 71-year-old male patient underwent cystoscopy on
6th February 2011 for painless, total gross hematuria. A 2.5
cm-diameter, solid, pedunculated mass with a necrotic lesion on the
surface of the right side of the bladder wall was identified
(Fig. 1A). The patient had a
10-year history of hypertension and had received a coronary artery
stent for coronary heart disease five years previously, in addition
to a four-year history of gout. Bladder mass biopsy revealed
low-grade papillary urothelial carcinoma. The patient underwent
transurethral resection (TUR) of the lesion. Five weeks later, the
patient underwent a second TUR for persistent gross hematuria. A
mass was identified on the right-side wall, and the pathological
results were compatible with a diagnosis of sarcomatoid carcinoma.
Seven months later, the patient underwent a third TUR for tumor
recurrence. The histopathological findings suggested a diagnosis of
sarcomatoid carcinoma, but no bladder mass was detected by computed
tomography scan prior to the resection (Fig. 1B). In accordance with the
pathological results, a radical cystectomy with regional lymph node
dissection and Bricker ileal conduit urinary diversion was
performed. The final pathological sections indicated a diagnosis of
PSCN.
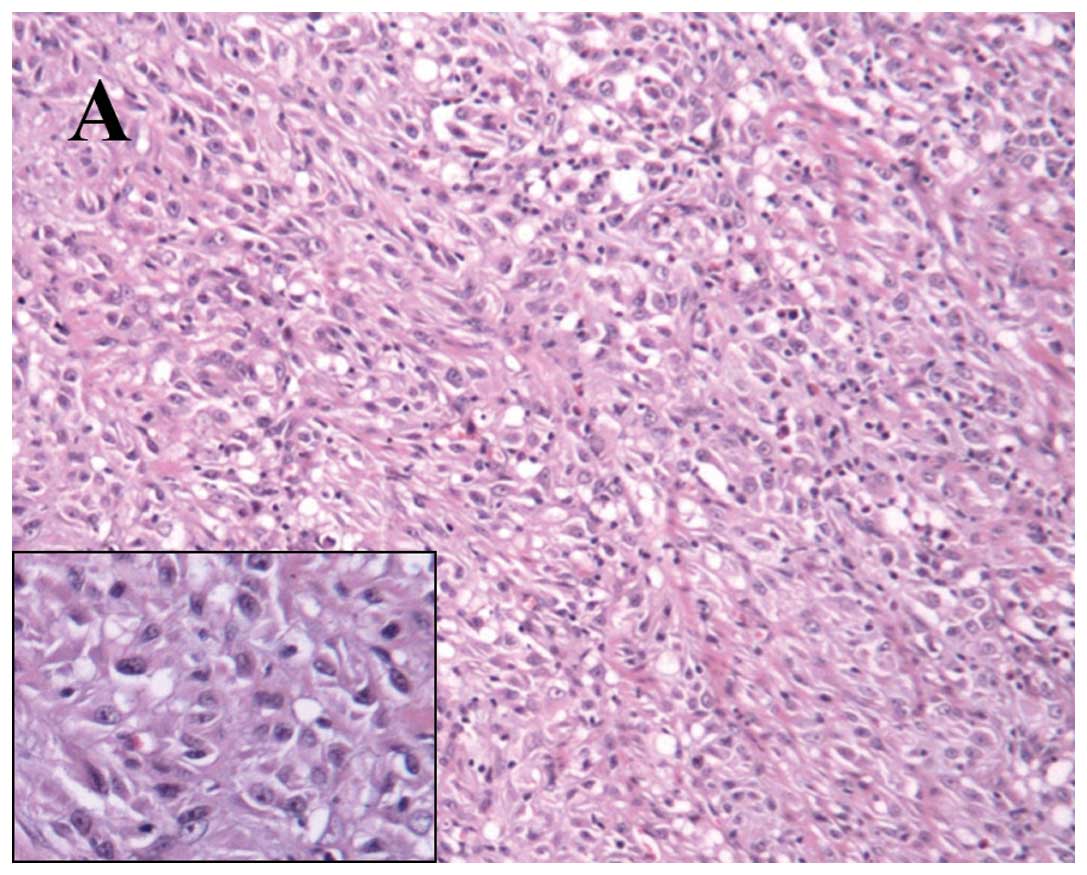
Immunostaining was performed on fixed sections
embedded in paraffin with appropriate controls. Stains for the
expression of vimentin and cytokeratin were positive, and focal
positivity for smooth muscle actin (SMA) and cytokeratin (CK)8/18
was noted (Fig. 2). The Ki-67 index
was 15%. Immunostaining for desmin, epithelial membrane antigen
(EMA), S-100, CK34β E12, CK14, P63, CK7 and CK20 was negative. The
patient received no further therapy and was without evidence of
disease 14 months later.
Discussion
PSCN of the urinary bladder was first reported in
1984 by Proppe et al (3),
who coined the term ‘post-operative spindle cell nodule’ in a study
including a series of eight patients with proliferation of spindle
cells following surgical procedures. In the article, Proppe
reported in detail the clinical findings, pathological features and
initial diagnoses of these cases. However, due to the limitations
of the technology at the time, the authors did not analyze the
lesions using immunohistochemical methods and examined the nodules
using only light microscopy.
Microscopic examination revealed several important
characteristics of PSCN (4,5), including intersecting fascicles of
spindle cells, small blood vessels and various chronic inflammatory
cells scattered in myxoid stroma. The spindle cells were arranged
in bundles or nodules, which had compacted acidophilic cytoplasm
and elongated, blunt-ended nuclei. There were numerous mitotic
figures among the spindle cells but without significant atypia. The
spindle cells frequently invaded the bladder walls between smooth
muscles and penetrated through the walls into surrounding soft
tissue without disrupting the muscle fibers (2). Small foci of hemorrhage and moderate
edema were present in the stroma. The inflammatory cells included
plasma cells, lymphocytes and macrophages and, in a few cases
(5), neutrophils and eosinophils
were identified during examination. Necrosis and calcification were
absent.
PSCN and sarcomatoid carcinoma are difficult to
distinguish from one another (2,6). The
two diseases share numerous similarities, including numerous
spindle cells scattered in myxoid stroma and various chronic
inflammatory cells in the surroundings. However, sarcomatoid
carcinoma is a rare malignancy of the bladder with markedly
atypical spindle cell proliferation and increased irregular
mitoses.
PubMed and Embase were searched for all reports of
spindle cell bladder tumors. The inclusion criterion for cases was
a diagnosis of PSCN of the bladder by the referring pathologist.
Six articles were identified, comprising 21 cases, including the
patient of the present report. General patient information and
histological data were tabulated (Tables I and II). Patients ranged in age between 40 and
85 years (mean, 65 years). Males were affected more than females
(1.6:1). The majority of the patients presented with hematuria
(4/6). The lesions ranged in size between 0.4 and 4.5 cm
(mean, 2.0 cm). The percentage of cases without invasion of
the muscularis was 62.5% (10/16) and, immunohistochemically, the
lesional cells of PSCN stained positive for cluster of
differentiation 68 (100%), vimentin (100%), CK AE1/AE3 (84%), SMA
(81%), muscle-specific actin (MSA; 80%), desmin (57%), p53 (60%)
and EMA (14%). S-100 protein was negative. Micci et al
(7) identified three signals for
chromosome 7 in one case by interphase fluorescence in situ
hybridization. Another report demonstrated that PSCN and
sarcomatoid carcinoma stained positive for vimentin, and that some
PSCNs stained positive for CK and EMA, which may lead to
misdiagnosis of sarcomatoid carcinomas (6). However, MSA and SMA are negative in
sarcomatoid carcinoma tissue but positive in PSCN tissue.
Differences are also apparent under electron microscopy, which
reveals fibroblastic or myofibroblastic differentiation in PSCN in
contrast to epithelial differentiation in sarcomatoid carcinoma
(8,9).
 | Table IClinical data of 21 patients with
postoperative spindle cell nodule of the bladder. |
Table I
Clinical data of 21 patients with
postoperative spindle cell nodule of the bladder.
| Case | Age, years | Gender | Prior bladder
procedures | Symptoms | Nodule size, cm | T stage | Therapy | Follow-up status,
months | Study |
|---|
| 1 | 49 | M | Biopsy, 2 months
priora | Hematuria | 3.0 | 2 | PC | CIS (12) | Iczkowski et
al (10) |
| 2 | 83 | M | TUR, 1 week
priora | Hematuria | 1.7 | 2 | TUR | NET (8.5) | Iczkowski et
al (10) |
| 3 | 56 | M | 7 biopsies, 5 months
priora | None | 0.8 | ND | TUR | NET (30) | Iczkowski et
al (10) |
| 4 | 70 | M | 13 TURs, 13 months
priora | None | 0.4 | ND | TUR | NET (26.4) | Iczkowski et
al (10) |
| 5 | 64 | M | TUR, 3 months
priora | Hematuria | ND | 2 | TUR | NET (24) | Micci et al
(7) |
| 6 | 75 | F | TUR | ND | ND | 1 | TUR | NET (27) | Spiess et al
(11) |
| 7 | 49 | F | TUR | ND | ND | a | TUR | NET(13) | Spiess et al
(11) |
| 8 | 78 | F | TUR | ND | ND | a | TUR | NET (2) | Spiess et al
(11) |
| 9 | 71 | M | TUR | ND | ND | 2 | PC | NET (67) | Spiess et al
(11) |
| 10 | 40 | M | TUR | ND | ND | 1 | TUR | NET (45) | Spiess et al
(11) |
| 11 | 85 | M | TUR | ND | ND | 1 | TUR | NET (46) | Spiess et al
(11) |
| 12 | 76 | F | TUR | ND | ND | 1 | TUR | DOD (48) | Spiess et al
(11) |
| 13 | 62 | M | TUR | ND | ND | a | TUR | NET (62) | Spiess et al
(11) |
| 14 | 72 | F | TUR | ND | ND | 1 | TUR | DOD (48) | Spiess et al
(11) |
| 15 | 66 | F | TUR | ND | ND | 1 | TUR | NET (34) | Spiess et al
(11) |
| 16 | 72 | M | ND | ND | 4.5 | <2 | ND | NET (62) | Montgomery et
al (5) |
| 17 | 73 | F | ND | ND | ND | ≥3 | ND | ND | Montgomery et
al (5) |
| 18 | 45 | F | TUR, 2 weeks
priora | Hematuria | 2.0 | ND | TUR | NET (24) | Lo et al
(12) |
| 19 | 55 | M | ND | Hematuria | ND | ND | TUR | NET (12) | Wick et al
(13) |
| 20 | 60 | M | ND | None | ND | ND | TUR | NET (6) | Wick et al
(13) |
| 21 | 71 | M | TUR, 5 weeks
priora | Hematuria | 1.5 | 3 | RC | NET (5) | Present case |
 | Table IIImmunohistochemical reactivity in 21
cases of postoperative spindle cell nodule of bladder. |
Table II
Immunohistochemical reactivity in 21
cases of postoperative spindle cell nodule of bladder.
| Study | p53 | CK AE 1/3 | EMA | SMA | MSA | Desmin | Vimentin | S-100 | CD 68 |
|---|
| Iczkowski et
al (10) | 3/4 | 2/4 | 1/3 | 2/4 | 2/3 | 2/3 | 4/4 | 0/3 | ND |
| Micci et al
(7) | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| Spiess et al
(11) | ND | 10/10 | ND | 10/10 | ND | ND | 10/10 | ND | 10/10 |
| Montgomery et
al (5) | ND | 1/1 | ND | ND | ND | ND | ND | ND | ND |
| Lo et al
(12) | 0/1 | 0/1 | 0/1 | 0/1 | ND | 0/1 | 1/1 | 0/1 | ND |
| Wick et al
(13) | ND | 2/2 | 0/2 | ND | 2/2 | 2/2 | 2/2 | 0/2 | ND |
| Present case | ND | 1/1 | 0/1 | 1/1 | ND | 0/1 | 1/1 | 0/1 | ND |
| Total | 3/5 | 16/19 | 1/7 | 13/16 | 4/5 | 4/7 | 18/18 | 0/7 | 10/10 |
The majority of PSCNs of the bladder were managed
locally by TUR. Partial cystectomies were performed on two
patients, and a radical cystectomy was performed on the patient of
the present study. Whether PSCN was only a type of reactive
proliferation or a true neoplasm remains unclear. Follow-up data
was available for 20 patients. No tumors recurred or metastasized
in 17 patients, suggesting that PSCN tends to be a benign lesion.
Two patients succumbed to other diseases. Only one patient was
diagnosed with carcinoma in situ of the bladder 12 months
after surgery, although the association between the recurrence and
the PSCN is not yet clear. Due to the good postoperative follow-up
results, the best choice for symptomatic patients is likely TUR,
while partial cystectomy and radical cystectomy should not be
recommended. Bladder-sparing surgery is advised to preserve the
patient’s quality of life.
In conclusion, this report has described a patient
with a postoperative spindle cell nodule that occurred in the
bladder following a TUR for treatment of bladder carcinoma. In
occasional cases, the recurrence of bladder mass following surgical
procedures may not be a malignant tumor, but a reactive
proliferation such as PSCN. Thus, it is necessary to perform a
preoperative biopsy before each surgery for diagnosis. Following
detailed pathological analysis and clear diagnosis, TUR is the
ideal treatment for avoiding extensive surgery.
References
|
1
|
Huang WL, Ro JY, Grignon DJ, Swanson D,
Ordonez NG and Ayala AG: Postoperative spindle cell nodule of the
prostate and bladder. J Urol. 143:824–826. 1990.PubMed/NCBI
|
|
2
|
Young RH: Tumor-like lesions of the
urinary bladder. Mod Pathol. 22(Suppl 2): S37–S52. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Proppe KH, Scully RE and Rosai J:
Postoperative spindle cell nodules of genitourinary tract
resembling sarcomas. A report of eight cases. Am J Surg Pathol.
8:101–108. 1984. View Article : Google Scholar
|
|
4
|
Kim SW, Oh YL, Choi JY, Lee JI, Chung JH
and Kim JS: Postoperative spindle cell nodule after thyroidectomy:
a case mimicking recurrence with anaplastic transformation of
thyroid cancer. Head Neck. 35:E13–E17. 2013. View Article : Google Scholar
|
|
5
|
Montgomery EA, Shuster DD, Burkart AL,
Esteban JM, Sgrignoli A, Elwood L, Vaughn DJ, Griffin CA and
Epstein JI: Inflammatory myofibroblastic tumors of the urinary
tract: a clinicopathologic study of 46 cases, including a malignant
example inflammatory fibrosarcoma and a subset associated with
high-grade urothelial carcinoma. Am J Surg Pathol. 30:1502–1512.
2006. View Article : Google Scholar
|
|
6
|
Lott S, Lopez-Beltran A, MacLennan GT,
Montironi R and Cheng L: Soft tissue tumors of the urinary bladder,
part I: myofibroblastic proliferations, benign neoplasms, and
tumors of uncertain malignant potential. Hum Pathol. 38:807–823.
2007. View Article : Google Scholar
|
|
7
|
Micci F, Haugom L, Abeler VM, Bjerkehagen
B and Heim S: Trisomy 7 in postoperative spindle cell nodules.
Cancer Genet Cytogenet. 174:147–150. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shanks JH and Iczkowski KA: Spindle cell
lesions of the bladder and urinary tract. Histopathology.
55:491–504. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Eyden B: Electron microscopy in the study
of myofibroblastic lesions. Semin Diagn Pathol. 20:13–24.
2003.PubMed/NCBI
|
|
10
|
Iczkowski KA, Shanks JH, Gadaleanu V,
Cheng L, Jones EC, Neumann R, Nascimento AG and Bostwick DG:
Inflammatory pseudotumor and sarcoma of urinary bladder:
differential diagnosis and outcome in thirty-eight spindle cell
neoplasms. Mod Pathol. 14:1043–1051. 2001. View Article : Google Scholar
|
|
11
|
Spiess PE, Tuziak T, Tibbs RF, Bassett R,
Tamboli P, Brown GA, Grossman HB, Ayala AG and Czerniak B:
Pseudosarcomatous and sarcomatous proliferations of the bladder.
Hum Pathol. 38:753–761. 2007. View Article : Google Scholar
|
|
12
|
Lo JW, Fung CH, Yonan T and DiMauro J:
Postoperative spindle-cell nodule of urinary bladder with unusual
intracytoplasmic inclusions. Diagn Cytopathol. 8:171–176. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wick MR, Brown BA, Young RH and Mills SE:
Spindle-cell proliferations of the urinary tract. An
immunohistochemical study. Am J Surg Pathol. 12:379–389. 1988.
View Article : Google Scholar : PubMed/NCBI
|