1. Introduction
The process by which surviving tumor cells have the
ability to continue proliferation during fractionated radiotherapy
is known as tumor repopulation, as the cells are able to regenerate
the tumor. There is evidence that the repopulation of tumor cells
can lead to radioresistance and limit the effectiveness of
radiotherapy (1,2). Conventional methods for detecting
tumor-cell repopulation include tumor control probability, 50%
tumor control dose (TCD50), potential doubling time (Tpot) and
pathological proliferation parameters. However, it is difficult to
separate viable cells from those destined for apoptosis during
fractionated radiotherapy using these methods. In vivo
imaging, tracking and targeting the repopulation of clonogenic
tumor cells has been of clinical interest, with the aim to
administer a higher dose of radiotherapy to repopulation regions
through use of intensity-modulated radiotherapy (IMRT). Functional
imaging tracers, such as 3′-deoxy-3′-18F-fluorothymidine
(18F-FLT), can reflect the proliferation of tumor cells
by showing the activity of thymidine kinase, and have been a useful
tool in estimating proliferation and predicting the response of
increased sensitively during radiotherapy (3,4). In
the present review, the demonstration of tumor-cell repopulation,
the molecular imaging of tumor stem cells and the non-invasive,
quantitative functional imaging for detecting tumor repopulation
during fractionated radiotherapy is explored.
2. Demonstration of tumor repopulation
during radiotherapy
Tumor repopulation, a hypothetical mechanism, was
found in clinical practice and was then demonstrated by animal
experiments and further corroborated by clinical studies.
Conventional fractionated radiotherapy is delivered in small doses
(1.8–2.0 Gy), which are often administered daily on weekdays with 5
fractions a week. The reason for this schedule is to allow the
recovery of normal tissues from sublethal radiation damage between
treatments and to avoid severe toxic reactions; however,
repopulation of surviving tumor cells may also occur (2). A series of clinical studies identified
that in certain types of cancer, including tonsilar fossa, bladder
and cervical cancer, the tumor control rate decreased dramatically
when overall treatment time was prolonged (5–7). A
study by Withers et al (8)
found that rapid tumor regrowth occurred during extensions of
radiotherapy treatment from ~5–8 weeks in almost 500 patients with
oropharyngeal cancer. The study concluded that clonogen
repopulation in squamous cell carcinomas of the head and neck
accelerates following a lag period of 4±1 weeks subsequent to the
initiation of radiotherapy. The existence of the significant time
factor for tumor tissues during fractionated radiotherapy has also
been corroborated by a large number of randomized phase III trials,
which demonstrated an impact of overall treatment time on local
control for head and neck, non-small cell lung and esophageal
cancers (9–11). There are also certain studies that
have used the linear-quadratic model to estimate tumor repopulation
rate and its onset time during radiotherapy, and to measure the
extra radiation dose required to compensate for the additional
duration of the treatment (12–14).
The existence of the significant time factor
stimulated basic research in the laboratory, with the aim to
demonstrate tumor repopulation during radiotherapy. A series of
animal experiments with varied overall treatment times were
performed in various mouse xenograft models, which included human
FaDu squamous cell carcinoma (15),
human melanoma (16), human soft
tissue sarcoma (17) and MCA-4
mammary carcinoma (18). In these
experiments, the parameters, including TCD50, Tpot or S phase
fraction (SPF), were used to reflect the proliferation activity.
Similar results showed that the tumor control rate decreased as the
overall treatment time increased. The extra radiation dose was
required to compensate for the additional duration of treatment.
Thus, tumor repopulation was inferred from the extra radiation dose
and decreased the tumor control rate.
It is now generally accepted in clinical practice
that prolongation of overall treatment time can lead to tumor
repopulation and it is essential that is it avoided. At present,
accelerated fractionation schedules have been widely accepted by
clinicians to shorten the overall treatment time of radiotherapy in
order to counteract tumor-cell repopulation (9,11).
Additionally, a study by Gao et al (1) recently proposed a cellular Potts model
that simulates the kinetics of glioma stem cells (GSCs) and
non-stem cancer cells (CCs) in glioblastoma growth and radiation
response. The study found that CCs die and GSCs become enriched and
potentially increase in number during each fraction of radiation,
which may lead to accelerated repopulation following fractionated
radiation treatment.
A study by Petersen et al (19) proved tumor repopulation using a
typical animal experiment during fractionated radiotherapy with
pathological validation. In the study, human FaDu squamous cell
carcinomas in nude mice were irradiated daily or every second day
with 12–18 fractions, 3 Gy per fraction. At various time points,
the tumors were excised and then stained for Ki-67 and
bromodeoxyuridine (BrdUrd), and the labeling indices were shown to
initially decrease and then increased again at later times during
the course of the fractionated radiotherapy. The staining intensity
of the epidermal growth factor receptor (EGFR) produced a similar
kinetic pattern, and the histological results were notably matched
with the kinetics of clonogenic tumor cell repopulation. Several
other animal models, including mouse fibrosarcoma and mouse ovarian
tumor (20,21), and clinical studies based on human
breast carcinoma and rectal cancer (22,23),
also revealed similar results that Ki-67, BrdUrd labeling indices
or SPF decreased initially and increased again at a later time
during the course of radiotherapy. Again, the histological results
were consistent with the kinetics of clonogen repopulation.
3. Conventional methods for detecting tumor
repopulation during radiotherapy
Conventional methods of measuring tumor repopulation
are based on tumor volume or diameter changes measured visually,
Ki-67 and BrdUrd detection by immunohistochemical staining
(19) or SPF and Tpot determined by
flow cytometry (24). These methods
have been shown to provide useful clinical information in various
human cancers and, notably, the pathological diagnosis is the gold
standard that indicates the presence or absence of cancer, the type
of cancer and its classification. It is desirable that tumor
repopulation could be proven by proliferation parameters with
Ki-67, BrdUrd or SPF. Methods of measuring tumor growth are less
sensitive as tumor repopulation may happen independent of tumor
diameter or volume change underlining the mechanisms of cell loss
decrease, a difference in cell repair and cell reoxygenation. The
anticancer effect of radiotherapy is applied through the
accumulation of DNA damage in the tumor cells, which may result in
acute or delayed cell death known as mitotic catastrophe.
Therefore, measuring tumor cell proliferation, as assessed by the
uptake of markers of DNA synthesis, such as BrdUrd, or by using
flow cytometry to measure DNA content, may not distinguish viable
cells from those destined to die during fractionated radiotherapy
(25). Also, immunohistochemical
staining methods require tissue samples and are therefore invasive
and limited by sampling variability. In a recent study by Gerlinger
et al (26), it was
identified that intratumor heterogeneity using immunohistochemical
analysis, mutation functional analysis and profiling of mRNA
expression may lead to underestimation of the genomics as depicted
from a single tumor-biopsy sample and may create major challenges
for personalized medicine and biomarker development.
Therefore, identifying a functional imaging
technology that is non-invasive, accurate, well reproducible and in
particular can detect the proliferation activity and therapeutic
efficacy in vivo has become a hot research topic.
4. Detecting proliferation of clonogenic
CSCs with non-invasive molecular imaging technology
In essence, the mechanism of tumor repopulation
involves the continuing proliferation of clonogenic cancer stem
cells (CSCs). In 2012, three studies were published that used a
genetic cell-labeling technique to monitor the proliferation of
CSCs (27–29). It has been shown that CSCs in the
brain, skin or intestinal tumors are indeed the source of tumor
regrowth (27). In vivo
imaging, tracking and targeting of the proliferation activity of
CSCs appears to be of significance.
Molecular imaging is a novel and non-invasive
strategy that allows real-time monitoring of CSCs, which are
believed to be responsible for tumor development, metastasis and
relapse following conventional therapy (30) in vivo, through use of various
molecular-targeted imaging probes that are specific for cell
surface biomarkers. Evidence that various solid tumors are
organized by hierarchy and maintained by a clear subpopulation of
CSCs is increasing. Pioneering studies using spontaneous mouse
leukemias and lymphomas have identified that the frequency of
tumor-propagating cells can range from 1% to the majority of cells
(31,32). A study by Leyton et al
(33) revealed a humanized
radioiodinated minibody as a positron emission tomography (PET)
imaging agent for the detection of prostate stem cell
antigen-positive prostate cancer. A study by Yoshii et al
(34) proposed Cu-64-diacetyl-bis
(N4-methylthiosemicar bazone) (Cu-64-ATSM) as a PET imaging agent
for the detection of cluster of differentiation 133+
(CD133+) CSCs. Tsurumi et al (35) showed that a CD133-specific
monoclonal antibody, AC133.1, may be used for quantitative
fluorescence-based optical imaging of mouse xenograft models.
A recent study from Vlashi et al (36) revealed that 72 h following
irradiation with 5×3 Gy in a human glioma model, there was an
increase in the percentage of CSCs. The study used the absence of
26S proteasome activity as a marker for monitoring CSCs and
implemented modern real-time imaging techniques. The percentage of
proliferating cells was also measured by an increase in Ki-67 to a
higher extent in marker-positive vs. marker-negative cells, which
are interpreted as an effect of repopulation of CSCs. The
development of molecular imaging for tracking CSCs in vivo
may provide the possibility of detecting repopulation of clonogenic
CSCs. However, concerns remain for the limitations of a clinical
imaging technique, such as PET, with a limited spatial resolution
for the detection of clonogenic CSCs, even if an appropriate
molecular imaging tracer exists, as in certain cases CSCs may
constitute <1% of the tumor population (37).
There remain numerous unresolved problems, despite
the substantial evidence for the existence of CSCs in mouse and
human carcinomas. High-resolution imaging technology together with
stromal markers shows promise and will improve the understanding of
the cellular niche for various CSCs.
5. PET tracers for imaging tumor-cell
proliferation in vivo: Current status
PET is a molecular imaging technique that can
provide various quantitative measurements of the underlying tumor
biology, depending on the radiotracer used. The radiotracer is
injected through a vein, accumulates in the tumor and the
radioactive emissions are detected by the PET camera. PET tracers,
including 2-11C-thymidine,
76Br-bromofluorodeoxyuridine (76Br-BFU) and
11C-2′fluoro-5-methyl-1-β-D-arabinofuranosyluracil
(11C-FMAU), are labeled nucleotides that are directly
incorporated into DNA. The thymidine analog,
3′-deoxy-3′-fluorothymidine (FLT), is currently the most widely
used radiotracer, and all are considered to be proliferation
markers and are useful additions to the imaging, which can provide
additional diagnostic specificity and biological information for
treatment planning and response monitoring. However, the short
half-life of 11C (20.4 min) and the rapid catabolism of
thymidine following injection results in 2-11C-thymidine
being less conducive for routine clinical use. Compared with
11C, 18F has a longer half-life (109.8 vs.
20.4 min) and is now generally accepted in clinical practice
(38). Limitations of
76Br-BFU are the necessity for co-injection with
cimetidine, the rather cumbersome production of 76Br and
the high radiation dose of 76Br (half-life of 16 h) as
compared with 11C or 18F (38). The main limitation of
11C- or 18F-FMAU appears to be that it is a
relatively poor substrate for thymidine kinase 1 (TK1) and a
relatively good substrate for TK2. The use of 11C- or
18F-FMAU is dependent on the extent to which tumor
uptake is associated with TK1 vs. TK2 activity. 11C- or
18F-FMAU retention may be less sensitive in comparison
with 18F-FLT retention in cell proliferation change
(39). Therefore, the PET
radiotracer, 18F-FLT, may show promise in assessing the
proliferation activity of tumors in vivo and the feasibility
in detecting tumor-cell repopulation.
6. Imaging proliferation of tumor cells via
18F-FLT labeling
FLT is a pyrimidine analog which, following uptake
into the cell, is phosphorylated by TK-1 into 18F-FLT
monophosphate, but is not directly incorporated into DNA, thus
causing intracellular sequestration of radioactivity (3,4). TK-1
is the main enzyme in the salvage pathway of DNA synthesis, and
increases in activity during the S phase of the cell cycle.
18F-FLT uptake, therefore, reflects the cell
proliferation status (40). A study
has shown that 18F-FLT, as a positron tracer reflecting
cell proliferation, can be used in PET imaging to observe in
vivo tumor cell proliferation at a molecular level,
non-invasively, and quantitatively across the entire tumor. For
pre-clinical studies, FLT uptake as a measurement of TK-1 activity
correlates strongly with pathology-based cell proliferation
measurements (41). For clinical
studies, however, results are conflicting with certain studies
demonstrating a good association between FLT and Ki-67 (42–44),
whilst others present a negative association (45–47).
Biological explanations for the absence of FLT/Ki-67 correlation
include a loss of cell cycle-specific regulation of TK1 (48), cell adenosine triphosphate levels
(48), FLT representing only the
salvage pathway of thymidine metabolism (49) and difference in the phosphorylation
rate between FLT and thymidine (45). In addition, the accuracy of the
measurement of the biopsy samples will be subject to sampling
errors and reduced reproducibility, as it does not take into
account the degree of intratumor heterogeneity expression for this
marker. Chalkidou et al (50) recently conducted a systematic review
and meta-analysis of the correlation between FLT and Ki-67. The
study attributed variations between FLT and Ki-67 to the methods
used and the study design. Larger clinical studies with an improved
study design are justified for validation of these findings for
specific cancer types which have conflicting results.
18F-FLT PET has been reported to have
more of a cancer-specificity for diagnosing malignancy compared
with 18F-FDG PET in head and neck, pancreatic and
esophageal cancer (51–53). There are several available studies
in which 18F-FLT and 18F-FDG uptake have been
compared in inflammatory tissues. The studies confirm that
18F-FLT is a more cancer-specific tracer and they
indicate that fewer false-positive 18F-FLT PET scans
occur in the patient (54,55). 18F-FLT PET has also been
shown to be a more sensitive tool that can provide an early
identification of tumor response for radiotherapy, chemotherapy or
EGFR inhibitor drugs (56–58). It can also sensitively reflect
proliferation of normal tissues during radiotherapy (56).
Notably, 18F-FLT PET has been reported to
detect tumor repopulation during fractionated radiotherapy. A pilot
clinical study using serial 18F-FLT PET/computed
tomography (CT) scans to measure tumor proliferation has been
performed by Yue et al (59). In the study, two patients out of 21
had unplanned interruptions of the radiotherapy treatment and then
underwent 18F-FLT PET/CT scans, which had a
corresponding increase in 18F-FLT uptake, indicating
tumor repopulation. The classic understanding of repopulation is
that it usually occurs following ~4 weeks of radiotherapy (8); however Fowler (60) indicates that repopulation begins
earlier. Experimental data from a study by Schmidt-Ullrich et
al (61) supports this
hypothesis, showing that the molecular process of accelerated
repopulation is mediated through radiation-induced EGFR activation,
and it may occur following a single 2-Gy fraction. A study by
Everitt et al (62) also
observed a ‘flare’ of 18F-FLT uptake in primary
non-small cell lung cancer following only 2 Gy irradiation.
In order for the use of 18F-FLT PET for
detecting tumor repopulation to be accepted and introduced into
clinical studies, validation with tumor histology is mandatory. A
study by Fatema et al (63)
evaluated the sequential changes in intratumoral proliferative
activity in head and neck cancer xenografts (FaDu) using FLT. The
study found that 6 h following radiation treatment, the
intratumoral 3H-FLT level diffusely decreased and then
subsequently increased gradually with time. This is consistent with
the experimental results of tumor repopulation that was
pathologically proven by Petersen et al (19). Other than this, there is no
literature reporting the detection of tumor repopulation using
functional imaging together with pathological validation. Also,
CSCs markers, including CD44+ and CD133+,
together with high-resolution imaging, will improve the
understanding of tumor repopulation during fractionated
radiotherapy.
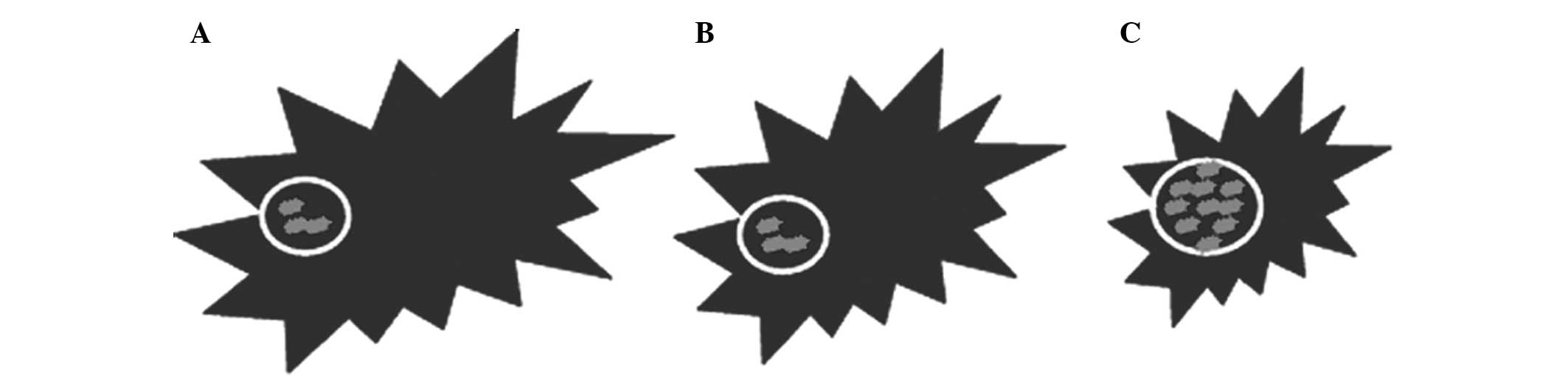
In addition, the reappearance of 18F-FLT
uptake is of great interest for investigation of the association
with the initial uptake prior to radiotherapy (Fig. 1). There is a difference in the
spatial correlation between the region of clonogenic tumor cells in
A and C in Fig. 1. If
18F-FLT PET/CT prior to treatment could predict
potential tumor repopulation, then it could also be used to
determine a biological target volume for radiotherapy. Thus, ‘dose
painting’ via IMRT may be applied to escalate dose to repopulation
regions.
7. Conclusion
The demonstration of tumor repopulation has
developed from clinical observation to animal experiments and human
cancer verification, which can be further corroborated and applied
in a clinical practice. Functional imaging, as a non-invasive,
quantitative method can be safely performed for any lesion and be
repeated multiple times, permitting the evaluation of an entire
tumor and providing information associated with the regional
heterogeneity in a tumor during radiotherapy. Functional imaging,
such as 18F-FLT PET, as a non-invasive, reliable and
promising functional imaging technique has been a useful tool in
oncology for estimating tumor proliferation change during
radiotherapy, with more specificity and sensitivity.
18F-FLT PET may present as one of the potential
molecular imaging modalities in vivo and for targeting the
repopulation of clonogenic tumor cells during fractionated
radiotherapy. Ongoing research based on pathology and modern
real-time imaging techniques together with CSC markers for tracking
of CSCs is underway in our institute to examine whether
18F-FLT PET can detect tumor repopulation during
radiotherapy in nude mice and humans.
Acknowledgements
This study was supported by the National Nature
Science Foundation of China (project no. 81101700).
References
|
1
|
Gao X, McDonald JT, Hlatky L and Enderling
H: Acute and fractionated irradiation differentially modulate
glioma stem cell division kinetics. Cancer Res. 73:1481–1490. 2013.
View Article : Google Scholar
|
|
2
|
Kim JJ and Tannock IF: Repopulation of
cancer cells during therapy: an important cause of treatment
failure. Nat Rev Cancer. 5:516–525. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Idema AJ, Hoffmann AL, Boogaarts HD, et
al: 3′-Deoxy-3′-18F-fluorothymidine PET-derived proliferative
volume predicts overall survival in high-grade glioma patients. J
Nucl Med. 53:1904–1910. 2012.
|
|
4
|
Herrmann K, Buck AK, Schuster T, et al: A
pilot study to evaluate 3′-deoxy-3′-18F-fluorothymidine pet for
initial and early response imaging in mantle cell lymphoma. J Nucl
Med. 52:1898–1902. 2011.
|
|
5
|
Maciejewski B and Majewski S: Dose
fractionation and tumour repopulation in radiotherapy for bladder
cancer. Radiother Oncol. 21:163–170. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Withers HR, Peters LJ, Taylor JM, et al:
Local control of carcinoma of the tonsil by radiation therapy: an
analysis of patterns of fractionation in nine institutions. Int J
Radiat Oncol Biol Phys. 33:549–562. 1995. View Article : Google Scholar
|
|
7
|
Petereit DG, Sarkaria JN, Chappell R, et
al: The adverse effect of treatment prolongation in cervical
carcinoma. Int J Radiat Oncol Biol Phys. 32:1301–1307. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Withers HR, Taylor JM and Maciejewski B:
The hazard of accelerated tumor clonogen repopulation during
radiotherapy. Acta Oncol. 27:131–146. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Baumann M, Herrmann T, Koch R, et al;
CHARTWEL-Bronchus studygroup. Final results of the randomized phase
III CHARTWEL-trial (ARO 97-1) comparing
hyperfractionated-accelerated versus conventionally fractionated
radiotherapy in non-small cell lung cancer (NSCLC). Radiother
Oncol. 100:76–85. 2011. View Article : Google Scholar
|
|
10
|
Wang JH, Lu XJ, Zhou J and Wang F: A
randomized controlled trial of conventional fraction and late
course accelerated hyperfraction three-dimensional conformal
radiotherapy for esophageal cancer. Cell Biochem Biophys.
62:107–112. 2012. View Article : Google Scholar
|
|
11
|
Nakamura K, Kodaira T, Shikama N, et al:
Accelerated fractionation versus conventional fractionation
radiation therapy for glottic cancer of T1-2N0M0 Phase III study:
Japan Clinical Oncology Group study (JCOG 0701). Jpn J Clin Oncol.
38:387–389. 2008. View Article : Google Scholar
|
|
12
|
Gao M, Mayr NA, Huang Z, Zhang H and Wang
JZ: When tumor repopulation starts? The onset time of prostate
cancer during radiation therapy. Acta Oncol. 49:1269–1275. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Huang Z, Mayr NA, Gao M, et al: Onset time
of tumor repopulation for cervical cancer: first evidence from
clinical data. Int J Radiat Oncol Biol Phys. 84:478–484. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang JZ and Li XA: Impact of tumor
repopulation on radiotherapy planning. Int J Radiat Oncol Biol
Phys. 61:220–227. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Petersen C, Zips D, Krause M, et al:
Repopulation of FaDu human squamous cell carcinoma during
fractionated radiotherapy correlates with reoxygenation. Int J
Radiat Oncol Biol Phys. 51:483–493. 2001. View Article : Google Scholar
|
|
16
|
Rofstad EK: Repopulation between radiation
fractions in human melanoma xenografts. Int J Radiat Oncol Biol
Phys. 23:63–68. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Allam A, Perez LA, Huang P, et al: The
effect of the overall treatment time of fractionated irradiation on
the tumor control probability of a human soft tissue sarcoma
xenograft in nude mice. Int J Radiat Oncol Biol Phys. 32:105–111.
1995. View Article : Google Scholar
|
|
18
|
Milas L, Yamada S, Hunter N, Guttenberger
R and Thames HD: Changes in TCD50 as a measure of clonogen doubling
time in irradiated and unirradiated tumors. Int J Radiat Oncol Biol
Phys. 21:1195–1202. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Petersen C, Eicheler W, Frömmel A, et al:
Proliferation and micromilieu during fractionated irradiation of
human FaDu squamous cell carcinoma in nude mice. Int J Radiat Biol.
79:469–477. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ramsay J, Suit HD, Preffer FI and Sedlacek
R: Changes in bromodeoxyuridine labeling index during radiation
treatment of an experimental tumor. Radiat Res. 116:453–461. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Thames HD, Ruifrok AC, Milas L, et al:
Accelerated repopulation during fractionated irradiation of a
murine ovarian carcinoma: downregulation of apoptosis as a possible
mechanism. Int J Radiat Oncol Biol Phys. 35:951–962. 1996.
View Article : Google Scholar
|
|
22
|
Kovarík J, Skry GD, Mikel J and Svoboda
VH: Changes of Ki67 index of various tumors during radiation
therapy. Neoplasma. 43:89–92. 1996.PubMed/NCBI
|
|
23
|
Gasinska A, Richter P, Darasz Z, et al:
Gender-related differences in repopulation and early tumor response
to preoperative radiotherapy in rectal cancer patients. J
Gastrointest Surg. 15:1568–1576. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Durand RE: Tumor repopulation during
radiotherapy: quantitation in two xenografted human tumors. Int J
Radiat Oncol Biol Phys. 39:803–808. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kummermehr JC: Tumour stem cells - the
evidence and the ambiguity. Acta Oncol. 40:981–988. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gerlinger M, Rowan AJ, Horswell S, et al:
Intratumor heterogeneity and branched evolution revealed by
multiregion sequencing. N Engl J Med. 366:883–892. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Gilbertson RJ and Graham TA: Cancer:
Resolving the stem-cell debate. Nature. 488:462–463. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen J, Li Y, Yu TS, McKay RM, et al: A
restricted cell population propagates glioblastoma growth after
chemotherapy. Nature. 488:522–526. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Schepers AG, Snippert HJ, Stange DE, et
al: Lineage tracing reveals Lgr5+ stem cell activity in mouse
intestinal adenomas. Science. 337:730–735. 2012.
|
|
30
|
Moncharmont C, Levy A, Gilormini M, et al:
Targeting a cornerstone of radiation resistance: cancer stem cell.
Cancer Lett. 322:139–147. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Furth J, Kahn MC and Breedis C: The
transmission of leukemia in mice with a single cell. Am J Cancer.
31:276–282. 1937.
|
|
32
|
Hewitt HB: Studies of the dissemination
and quantitative transplantation of a lymphocytic leukaemia of CBA
mice. Br J Cancer. 12:378–401. 1958. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Leyton JV, Olafsen T, Lepin EJ, et al:
Humanized radioiodinated minibody for imaging of prostate stem cell
antigen-expressing tumors. Clin Cancer Res. 14:7488–7496. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yoshii Y, Furukawa T, Kiyono Y, et al:
Internal radiotherapy with copper-64-diacetyl-bis
(N4-methylthiosemicarbazone) reduces CD133+ highly
tumorigenic cells and metastatic ability of mouse colon carcinoma.
Nucl Med Biol. 38:151–157. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Tsurumi C, Esser N, Firat E, et al:
Non-invasive in vivo imaging of tumor-associated CD133/prominin.
PLoS One. 5:e156052010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Vlashi E, Kim K, Lagadec C, et al: In vivo
imaging, tracking, and targeting of cancer stem cells. J Natl
Cancer Inst. 101:350–359. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Visvader JE and Lindeman GJ: Cancer stem
cells in solid tumours: accumulating evidence and unresolved
questions. Nat Rev Cancer. 8:755–768. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
van WA and Elsinga PH: Proliferation
markers for the differential diagnosis of tumor and inflammation.
Curr Pharm Des. 14:3326–3339. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Bading JR and Shields AF: Imaging of cell
proliferation: status and prospects. J Nucl Med. 49(Suppl 2):
64S–80S. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Soloviev D, Lewis D, Honess D and Aboagye
E: [(18)F]FLT: an imaging biomarker of tumour proliferation for
assessment of tumour response to treatment. Eur J Cancer.
48:416–424. 2012.
|
|
41
|
Leyton J, Latigo JR, Perumal M, Dhaliwal
H, He Q and Aboagye EO: Early detection of tumor response to
chemotherapy by 3′-deoxy-3′-[18F]fluorothymidine positron emission
tomography: the effect of cisplatin on a fibrosarcoma tumor model
in vivo. Cancer Res. 65:4202–4210. 2005.
|
|
42
|
Yamamoto Y, Nishiyama Y, Ishikawa S, et
al: Correlation of 18F-FLT and 18F-FDG uptake on PET with Ki-67
immunohistochemistry in non-small cell lung cancer. Eur J Nucl Med
Mol Imaging. 34:1610–1616. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yamamoto Y, Ono Y, Aga F, Kawai N, Kudomi
N and Nishiyama Y: Correlation of 18F-FLT uptake with tumor grade
and Ki-67 immunohistochemistry in patients with newly diagnosed and
recurrent gliomas. J Nucl Med. 53:1911–1915. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Vesselle H, Grierson J, Muzi M, et al: In
vivo validation of 3′deoxy-3′-[(18)F]fluorothymidine ([(18)F]FLT)
as a proliferation imaging tracer in humans: correlation of
[(18)F]FLT uptake by positron emission tomography with Ki-67
immunohistochemistry and flow cytometry in human lung tumors. Clin
Cancer Res. 8:3315–3323. 2002.
|
|
45
|
van Westreenen HL, Cobben DC, Jager PL, et
al: Comparison of 18F-FLT PET and 18F-FDG PET in esophageal cancer.
J Nucl Med. 46:400–404. 2005.
|
|
46
|
Benz MR, Czernin J, Allen-Auerbach MS, et
al: 3′-deoxy-3′-[18F]fluorothymidine positron emission tomography
for response assessment in soft tissue sarcoma: a pilot study to
correlate imaging findings with tissue thymidine kinase 1 and Ki-67
activity and histopathologic response. Cancer. 118:3135–3144.
2012.
|
|
47
|
Yamamoto Y, Kameyama R, Izuishi K, et al:
Detection of colorectal cancer using 18F-FLT PET: comparison with
18F-FDG PET. Nucl Med Commun. 30:841–845. 2009. View Article : Google Scholar
|
|
48
|
Kameyama R, Yamamoto Y, Izuishi K, et al:
Detection of gastric cancer using 18F-FLT PET: comparison with
18F-FDG PET. Eur J Nucl Med Mol Imaging. 36:382–388. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Schwartz JL, Tamura Y, Jordan R, Grierson
JR and Krohn KA: Monitoring tumor cell proliferation by targeting
DNA synthetic processes with thymidine and thymidine analogs. J
Nucl Med. 44:2027–2032. 2003.PubMed/NCBI
|
|
50
|
Chalkidou A, Landau DB, Odell EW,
Cornelius VR, O’Doherty MJ and Marsden PK: Correlation between
Ki-67 immunohistochemistry and 18F-fluorothymidine uptake in
patients with cancer: A systematic review and meta-analysis. Eur J
Cancer. 48:3499–3513. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Hoshikawa H, Kishino T, Mori T, Nishiyama
Y, Yamamoto Y and Mori N: The value of 18F-FLT PET for detecting
second primary cancers and distant metastases in head and neck
cancer patients. Clin Nucl Med. 38:e318–e323. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Herrmann K, Erkan M, Dobritz M, et al:
Comparison of 3′-deoxy-3′-[18F]fluorothymidine positron emission
tomography (FLT PET) and FDG PET/CT for the detection and
characterization of pancreatic tumours. Eur J Nucl Med Mol Imaging.
39:846–851. 2012.
|
|
53
|
Han D, Yu J, Zhong X, et al: Comparison of
the diagnostic value of 3-deoxy-3-18F-fluorothymidine and
18F-fluorodeoxyglucose positron emission tomography/computed
tomography in the assessment of regional lymph node in thoracic
esophageal squamous cell carcinoma: a pilot study. Dis Esophagus.
25:416–426. 2012. View Article : Google Scholar
|
|
54
|
van Waarde A, Cobben DC, Suurmeijer AJ, et
al: Selectivity of 18F-FLT and 18F-FDG for differentiating tumor
from inflammation in a rodent model. J Nucl Med. 45:695–700.
2004.PubMed/NCBI
|
|
55
|
Halter G, Buck AK, Schirrmeister H, et al:
[18F] 3-deoxy-3′-fluorothymidine positron emission tomography:
alternative or diagnostic adjunct to
2-[18f]-fluoro-2-deoxy-D-glucose positron emission tomography in
the workup of suspicious central focal lesions? J Thorac Cardiovasc
Surg. 127:1093–1099. 2004.
|
|
56
|
Agool A, Slart RH, Thorp KK, et al: Effect
of radiotherapy and chemotherapy on bone marrow activity: a
18F-FLT-PET study. Nucl Med Commun. 32:17–22. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Troost EG, Bussink J, Hoffmann AL, Boerman
OC, Oyen WJ and Kaanders JH: 18F-FLT PET/CT for early response
monitoring and dose escalation in oropharyngeal tumors. J Nucl Med.
51:866–874. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Scheffler M, Kobe C, Zander T, et al:
Monitoring reversible and irreversible EGFR inhibition with
erlotinib and afatinib in a patient with EGFR-mutated non-small
cell lung cancer (NSCLC) using sequential [18F]fluorothymidine
(FLT-)PET. Lung Cancer. 77:617–620. 2012.PubMed/NCBI
|
|
59
|
Yue J, Chen L, Cabrera AR, et al:
Measuring tumor cell proliferation with 18F-FLT PET during
radiotherapy esophageal squamous cell carcinoma: a pilot clinical
study. J Nucl Med. 51:528–534. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Fowler JF: Rapid repopulation in
radiotherapy: a debate on mechanism. The phantom of tumor treatment
- continually rapid proliferation unmasked. Radiother Oncol.
22:156–158. 1991. View Article : Google Scholar
|
|
61
|
Schmidt-Ullrich RK, Contessa JN, Dent P,
et al: Molecular mechanisms of radiation-induced accelerated
repopulation. Radiat Oncol Investig. 7:321–330. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Everitt S, Hicks RJ, Ball D, et al:
Imaging cellular proliferation during chemo-radiotherapy: a pilot
study of serial 18F-FLT positron emission tomography/computed
tomography imaging for non-small-cell lung cancer. Int J Radiat
Oncol Biol Phys. 75:1098–1104. 2009. View Article : Google Scholar
|
|
63
|
Fatema CN, Zhao S, Zhao Y, et al:
Monitoring tumor proliferative response to radiotherapy using
(18)F-fluorothymidine in human head and neck cancer xenograft in
comparison with Ki-67. Ann Nucl Med. 27:355–362. 2013. View Article : Google Scholar : PubMed/NCBI
|