Introduction
Malignant fibrous histiocytoma (MFH) was first
described as a distinct histological type of soft tissue sarcoma in
1964 (1). MFH may occur in the
extremities, retroperitoneum and trunk, however, it rarely
originates in the chest wall. Yoshida et al (2) reported that primary MFH of the chest
wall predominantly affects elderly male patients with a variable
clinical presentation.
Surgery is considered to be the most adequate
therapy for MFH and resection with negative microscopic margins
decreases the incidence of local recurrence (3). Therefore, the predominant modus
operandi is wide excision, however, it may, lead to a
considerably reduced quality of life. Radiotherapy (RT) has also
been described as a definitive treatment for patients with MFH and
unresectable or positive surgical margins (4). Furthermore, the advances in RT present
stereotactic body RT (SBRT) as a novel technique for the treatment
of human tumors. SBRT (for example CyberKnife® RT)
allows the delivery of a higher dose of radiation to the tumor
while reducing the quantity of irradiation to the surrounding
normal tissue (5). The current
study reports the treatment of a patient with an unresectable MFH
of the chest wall using CyberKnife® RT.
Case report
Patient presentation and diagnosis
The current study presents a patient who developed
an unresectable MFH in the chest wall. As the tumor was an
unresectable mass, CyberKnife® RT was conducted and,
following the treatment, a marked reduction in the tumor size was
observed with a tolerable level of toxicity. In addition, a
separate literature search was performed using PubMed on February
1, 2012. The search criteria used were ‘malignant fibrous
histiocytoma’ and ‘CyberKnife’, with the search ‘case reports’ used
as a limitation; the search criteria included all languages. Review
of the literature identified only one case of MFH with
Cyberknife® treatment and the tumor was reduced
following Cyberknife® treatment. Written informed
consent was obtained from the patient for the publication of this
case report and the accompanying images.
Treatment and clinical course
In August 2012, a 77-year-old male presented to the
Jingling Hospital (Nanjing, China) with a four-month history of a
gradually increasing painless mass in the right chest wall and
intermittent fever. The patient’s medical history included
prostatic hyperplasia, cholecystolithiasis and a cyst of the right
kidney. The patient had no history of smoking or asbestos exposure.
The tumor was elastic-hard, tender and characterized by a distinct
border between the tumor and the normal tissue. The laboratory
examinations showed mild anemia, hyponatremia, hypoalbuminemia and
a high C-reactive protein concentration. Additionally, the levels
of tumor markers, including carcinoembryonic antigen, carbohydrate
antigen 19-9, neuron specific enolase and squamous cell carcinoma
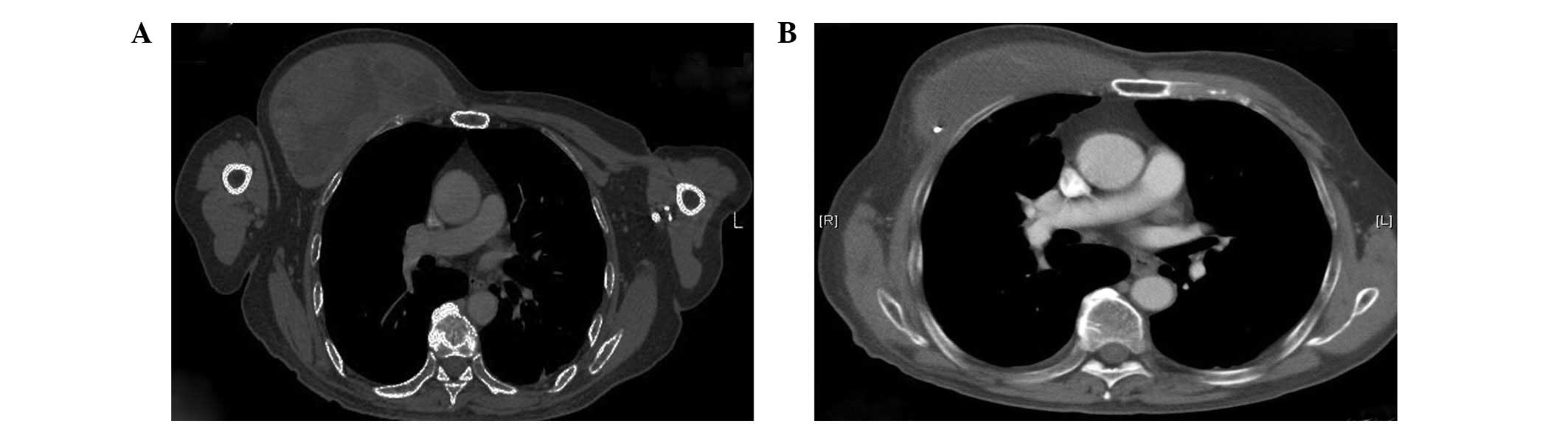
antigen, were within the normal limits. Computed tomography (CT)
revealed a well-defined inhomogeneous mass in the right chest wall
and the lesion showed a heterogeneous isointense signal on
T1-weighted magnetic resonance imaging (MRI) and a high-intensity
signal on T2-weighted MRI. The CT and MRI observations indicated
the diagnosis of MFH or myxoid type liposarcoma. In addition, a
percutaneous needle biopsy was performed and yielded three tissue
fragments from the mass; grossly, the tissues appeared red and
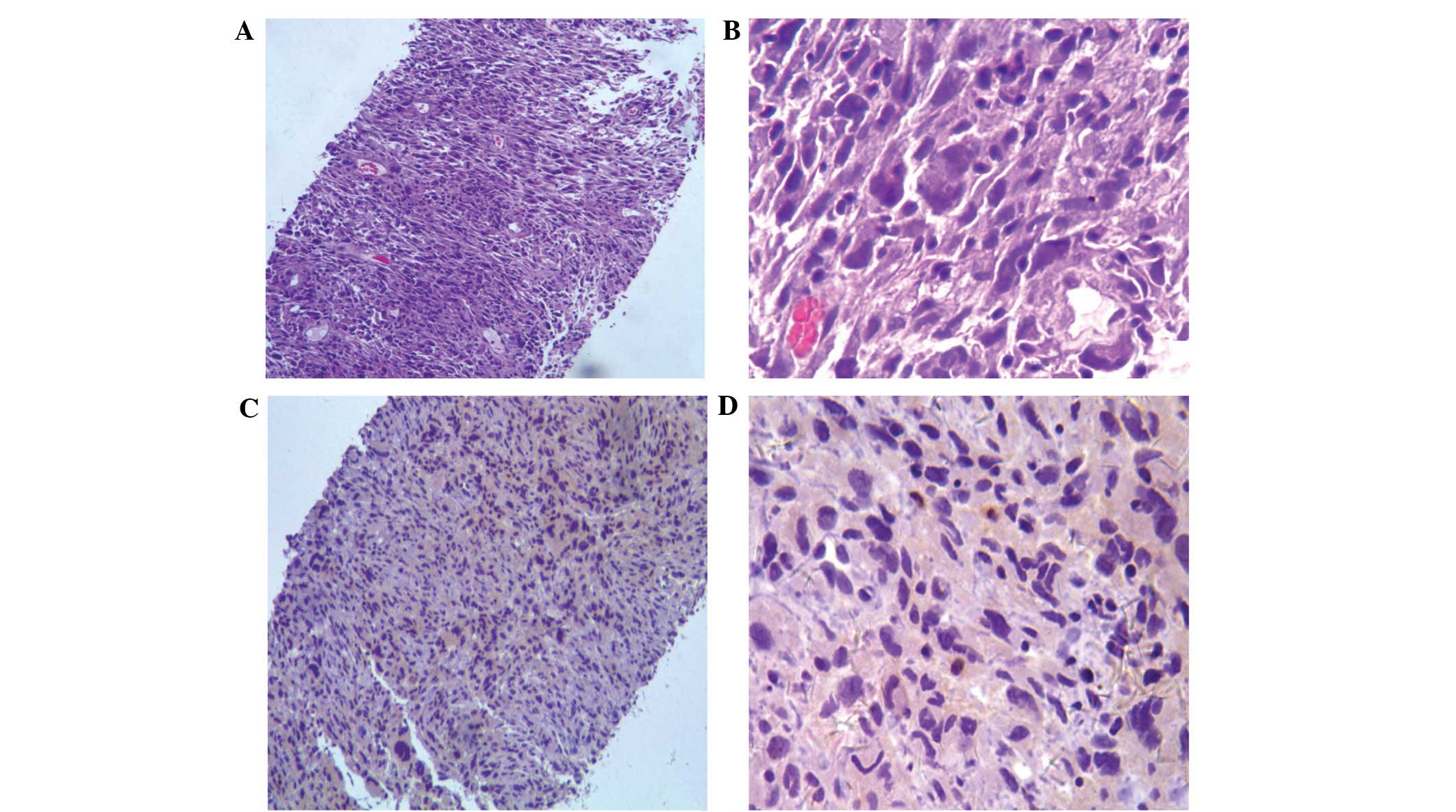
soft. The pathological slices was visualized using an Olympus BX31
microscope (Olympus, Tokyo, Japan) at ×100 and ×400 magnification.
Microscopically, a storiform pattern of spindle cells and
multinucleated giant cancer cells with atypical mitotic figures
were observed, as well as hemorrhaging and necrosis. Furthermore,
the immunohistochemical studies were negative for cytokeratin 5/6
and calretinin, but positive for vimentin (Fig. 1); therefore, MFH was diagnosed.
Since the tumor was regarded as unresectable, RT was proposed to
reduce the size of the tumor and ameliorate the symptoms associated
with tumor growth. Epidermal growth factor receptor (EGFR) mutation
tests were also performed to gain a better understanding. However,
the sequencing analysis showed that exon 19 of the EGFR gene
harbored a heterozygous in-frame deletion removing amino acids 746
to 750 (delE746-A750). Based on this result, gefitinib was
prescribed at a dose of 250 mg/day as maintenance therapy.
Radiosurgical planning
SBRT was performed using CyberKnife®
(Accuray Corporate, Sunnyvale, CA, USA) technology, which is a
robotic, image-guided, full-body RT system. The system was equipped
with the Synchrony® Respiratory Tracking Device
(Accuracy Corporate), which enables the CyberKnife®
technology to compensate for any tumor motion; however, the device
requires the insertion of gold fiducial markers close to the tumor.
Briefly, patients must have three gold fiducial markers
(3×0.8-mm gold seeds) implanted inside the tumor to
determine the tumor position. The fiducial markers may be placed by
percutaneous needle placement using an 18-/19-gauge coaxial needle
under image guidance and local anesthesia. Approximately one week
following the placement of the fiducial markers, CT simulation was
performed for the purpose of treatment planning. This time interval
is sufficient to allow resolution of the edema and to identify any
injury that may have occurred during the fiducial placement, as
well as to allow for fiducial stabilization. In the present study,
the MFH of the right chest wall measured 14.8×8.1 cm, with a
1,097-cm3 volume. The patient was subsequently
prescribed an RT dose of 75 Gy to the 75% isodose line, which was
delivered in five fractions. In addition, the volume of the right
lung receiving ≥20 Gy was 15%.
Clinical outcome
At four months following the CyberKnife®
RT, the tumor had reduced from 14.8×8.1 to 10.9×4.5 cm in size and
notably, the solid lesion of the mass had significantly reduced
(Fig. 2). The treatment-associated
toxicity was assessed according to the Radiation Therapy Oncology
Group (6) and the patient
experienced grade 1 acute toxicity fatigue and mild
radiodermatitis. Furthermore, late grade 1 toxicity radiodermatitis
and pneumonitis were observed at four months following the
CyberKnife® RT.
Discussion
MFH is the most common type of soft tissue sarcoma
in adults accounting for 10% of all soft tissue sarcomas and
predominantly occurs in males. Furthermore, MFH most commonly
arises in the extremities (68%), trunk (16%) and retroperitoneum
(16%), however, rarely presents in the chest wall (3). The majority of MFH tumors in adults
can be classified according to a specific line of differentiation
into the following five subtypes: Pleomorphic storiform, myxoid,
giant cell, inflammatory and angiomatoid (7). The pleomorphic storiform and myxoid
subtypes are generally high-grade neoplasms, while the others are
usually low-grade sarcomas (8). The
mean age of patients with primary MFH of the chest wall is 64.9
years (age range, 6–94 years) (2).
Furthermore, the most common complaints are a non-painful mass
(75%), a painful mass (13%) and pain alone (10%) (9). The present patient was older than the
average MFH patient (77 years), and the patient’s initial
presentation was a gradually increasing painless mass in the right
chest wall, with intermittent fever. The features of the MFH
identified by imaging of the chest wall were non-specific. The CT
demonstrated a heterogeneous enhancing mass and the MRI showed
signal intensities that were similar to, or lower than, that of
muscle on T1-weighted images, which are often inhomogeneous and
similar to, or greater than, that of adipose tissue on T2-weighted
images (10).
MFH has a high propensity for local recurrence and
distant metastasis; however, resection with negative microscopic
margins decreases the incidence of local recurrence. Complete
surgical resection at the time of primary tumor presentation
remains the most effective therapy and additional chemotherapy may
aid in the treatment of MFH (11,12).
Mauri et al (13) also
reported that the tyrosine kinase inhibitor may effectively
function on patients affected by advanced stage MFH. In the current
case, the EGFR mutation test was performed as a compassionate
attempt. However, the sequencing analysis showed an in-frame
deletion (delE746-A750) in exon 19 of the EGFR gene. Based on this
result, gefitinib was administered at a dose of 250 mg/day and
subsequently, the patient’s condition remained stable. RT has also
been described as a definitive treatment for MFH patients with
unresectable or positive surgical margins (14). The CyberKnife® RT
combined with respiratory gating in patients, as well as high
total-dose RT with hypofractionation may be used to achieve
permanent local control (5). In
addition, Nagano et al (15)
reported a patient with MFH presenting in the buccal region who
underwent irradiation using a CyberKnife® system
following the failure of external RT at a dose of 38 Gy. The
CyberKnife® irradiation was performed twice at doses of
37 and 25 Gy. In the present case, the CyberKnife®
irradiation was delivered at a dose of 75 Gy in five fractions over
five days. Following the treatment, the tumor gradually reduced in
size with tolerable levels of toxicity.
In conclusion, the present study reports the
feasibility of SBRT (specifically, CyberKnife® RT) for
the palliation of a patient with an MFH arising in the chest wall.
No grade 3 or higher toxicity was observed in the patient, which
indicates that this technique may be a useful treatment for
unresectable MFH of the chest wall. However, further study is
required to determine the optimal target dose, long-term toxicity
and efficacy of this approach.
References
|
1
|
O’Brien JE and Stout AP: Malignant fibrous
xanthomas. Cancer. 17:1445–1455. 1964.
|
|
2
|
Yoshida N, Miyanari N, Yamamoto Y and
Egami H: Successful treatment of malignant fibrous histiocytoma
originating in the chest wall: report of a case. Surg Today.
36:714–721. 2006. View Article : Google Scholar
|
|
3
|
Shikada Y, Yoshino I, Fukuyama S, Kameyama
T and Maehara Y: Completely wide resection of malignant fibrous
histiocytoma of the chest wall: expect for long survival. Ann
Thorac Cardiovasc Surg. 12:141–144. 2006.PubMed/NCBI
|
|
4
|
Raut CP and Pisters PW: Retroperitoneal
sarcomas: Combined-modality treatment approaches. J Surg Oncol.
94:81–87. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mintz A and Heron DE: CyberKnife(R)
robotic stereotactic radiosurgery and stereotactic body radiation
therapy. Technol Cancer Res Treat. 9:539–540. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cox JD, Stetz J and Pajak TF: Toxicity
criteria of the Radiation Therapy Oncology Group (RTOG) and the
European Organization for Research and Treatment of Cancer (EORTC).
Int J Radiat Oncol Biol Phys. 31:1341–1346. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Al-Agha OM and Igbokwe AA: Malignant
fibrous histiocytoma: between the past and the present. Arch Pathol
Lab Med. 132:1030–1035. 2008.PubMed/NCBI
|
|
8
|
Anagnostopoulos G, Sakorafas GH,
Grigoriadis K and Kostopoulos P: Malignant fibrous histiocytoma of
the liver: a case report and review of the literature. Mt Sinai J
Med. 72:50–52. 2005.PubMed/NCBI
|
|
9
|
Sawai H, Kamiya A, Kurahashi S, Yamanaka Y
and Manabe T: Malignant fibrous histiocytoma originating from the
chest wall: report of a case and collective review of cases. Surg
Today. 28:459–463. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
O’Sullivan P, O’Dwyer H, Flint J, Munk PL
and Muller N: Soft tissue tumours and mass-like lesions of the
chest wall: a pictorial review of CT and MR findings. Br J Radiol.
80:574–580. 2007.PubMed/NCBI
|
|
11
|
Abe T, Yamanaka K, Nakata W, Mori N, Sekii
K, Yoshioka T and Itatani H: A case of retroperitoneal malignant
fibrous histiocytoma with marked response to concurrent cisplatin
and radiation therapy: a case report. Hinyokika Kiyo. 53:241–246.
2007.(In Japanese).
|
|
12
|
Lehnhardt M, Daigeler A, Homann HH,
Schwaiberger V, Goertz O, Kuhnen C and Steinau HU: MFH revisited:
outcome after surgical treatment of undifferentiated pleomorphic or
not otherwise specified (NOS) sarcomas of the extremities - an
analysis of 140 patients. Langenbecks Arch Surg. 394:313–320. 2009.
View Article : Google Scholar
|
|
13
|
Mauri D, Panou C, Valachis A, Kamposioras
K and Tsali L: Tyrosine kinase inhibitors in treatment of fibrous
histiocytoma. Exp Oncol. 31:60–61. 2009.PubMed/NCBI
|
|
14
|
Gutierrez JC, Perez EA, Franceschi D,
Moffat FL Jr, Livingstone AS and Koniaris LG: Outcomes for
soft-tissue sarcoma in 8249 cases from a large state cancer
registry. J Surg Res. 141:105–114. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nagano H, Deguchi K and Kurono Y:
Malignant fibrous histiocytoma of the bucca: a case report. Auris
Nasus Larynx. 35:165–169. 2008. View Article : Google Scholar : PubMed/NCBI
|