Introduction
Pilomatrix carcinoma is a locally aggressive tumor,
usually occurring on the head and neck. A literature review
revealed that the mean age of diagnosis with pilomatrix carcinoma
is 45 years, and it occurs more often in middle-aged males, with a
male to female ratio of 4:1 (1). In
numerous patients diagnosed with pilomatrix carcinoma, a direct
invasion to the adjacent bone has been observed (2,3). Local
recurrence is expected if the tumor has not been excised with a
wide surgical margin. However, despite its limited metastatic
potential, the tumor may occasionally present rapid progression and
widespread metastases. Aggressive surgical treatment consisting of
wide local excision is indicated for pilomatrix carcinoma and the
goal of the surgery is to obtain negative surgical margins,
however, wide surgical excision is not an adequate intervention.
Adjuvant radiotherapy may be administered following surgery
(4). In addition, patients with
local invasion or metastatic properties may be treated with
chemotherapy and radiotherapy (5).
The current study reports a rare case of pilomatrix carcinoma. The
patient provided written informed consent.
Case report
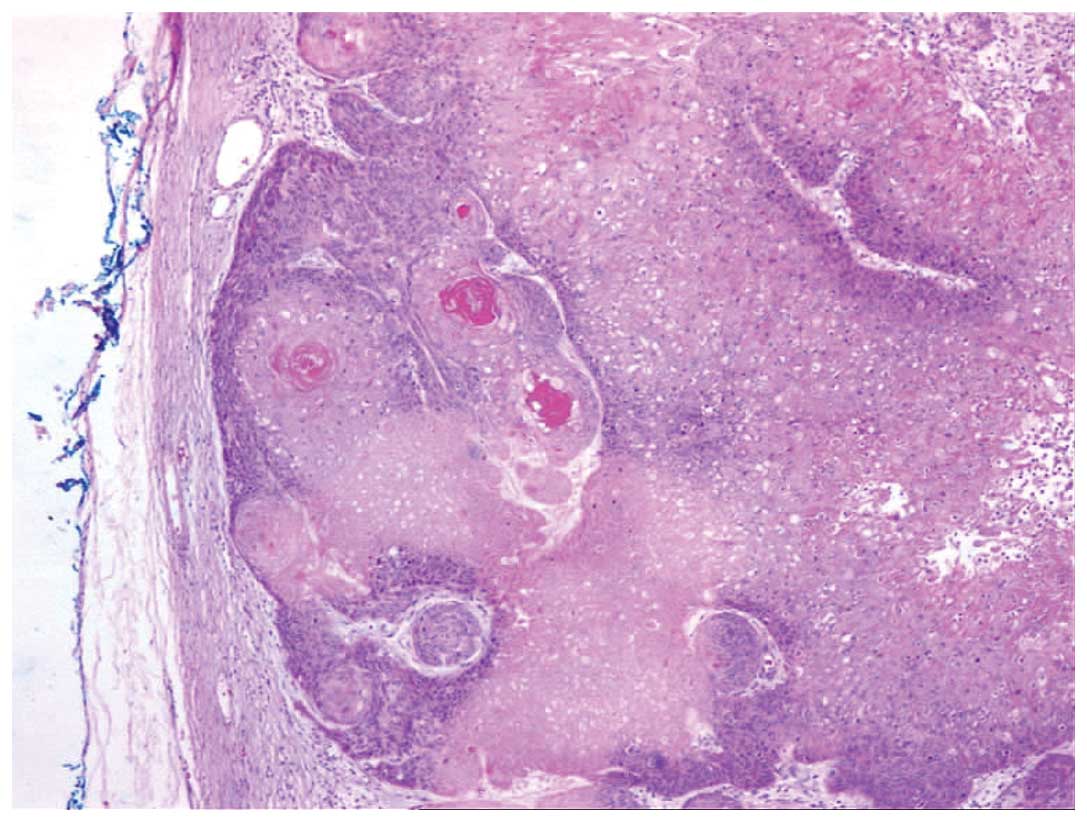
A 76-year-old male was referred to the Department of
Oncology, Akdeniz University Hospital (Konyaalti, Turkey) following
an excisional biopsy of a painless palpable mass located on the
patient’s scalp, and the diagnosis of pilomatrix carcinoma was
confirmed (Fig. 1). The physical
examination revealed a surgical scar measuring ~3×3 cm in diameter
on the left temporal region. Other systemic examination findings
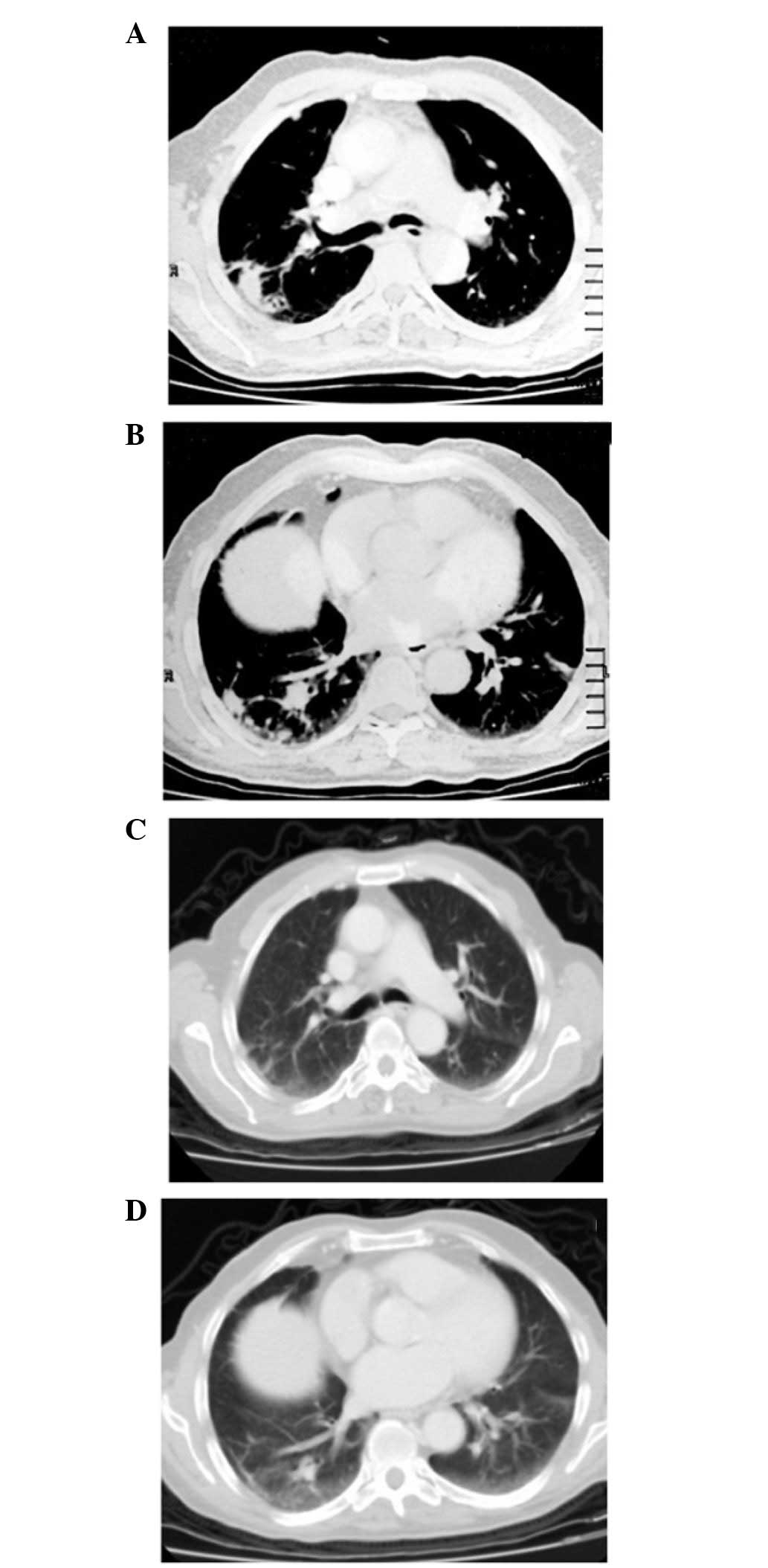
were within normal limits. A thoracic computed tomography (CT) scan
showed lymph nodes with pathologically negative surgical margins in
the right paratracheal mediastinal region, left paratracheal,
subcarinal and bilateral hilar regions. The short-axis diameter of
the largest lymph node measured 12–13 mm. The CT scan also
demonstrated multiple bilateral large nodular lesions throughout
the lung parenchyma, the largest of which was 2×1.5 cm (Fig. 2A and B), confirming pilomatrix
carcinoma with multiple lung metastases. The patient history
revealed that the patient received steroid therapy one year
previously for autoimmune hemolytic anemia (AIHA). The blood and
biochemical parameters of the patient were analyzed and the
complete blood count, transaminase, γ-glutamyl transferase,
alkaline phosphatase, blood, urea and nitrogen, and creatinine
levels were found to be within the normal limits.
Following the diagnosis of metastatic pilomatrix
carcinoma, the patient began combination chemotherapy with 50 mg
oral cyclophosphamide (1×1) everyday and 50 mg etoposide (2×1) for
five days, repeating treatment every 21 days for six courses.
Following six cycles of systemic chemotherapy, a follow-up thorax
CT scan showed mediastinal lymph nodes with a short-axis diameter
of >10 mm and segmental linear atelectasia in the parenchymal
window. The disappearance of all metastatic nodular lesions on the
follow-up CT scan was evaluated as a complete response. The patient
has been monitored in remission for six months.
Discussion
Pilomatrix carcinoma is a very rare tumor with, to
the best of our knowledge, ~90 cases reported in the literature. It
is a skin adnexal tumor originating from hair-follicle matrix
cells. While usually exhibiting locally invasive behavior, such as
basal-cell skin cancer, there are numerous studies reporting
patients with lung metastases. Gould et al (3) published the first known metastatic
pilomatrix carcinoma, reporting the distant metastasis to the lungs
that occurred four years following surgical excision (6,7). In
the present case, pulmonary metastasis had already occurred. The
patient of the present study was diagnosed with AIHA one year prior
to the diagnosis of pilomatrix carcinoma, and the hemoglobin levels
of the patient were within the normal range during
immunosuppressive therapy. To the best of our knowledge, there is
no study in the literature reporting a pilomatrix carcinoma case
that was complicated by AIHA.
In the differential diagnosis, pilomatrix carcinoma
should be differentiated from its more common counterparts,
pilomatrixoma and basaloid cell lesions. Pilomatrix carcinoma may
arise as a solitary lesion de novo or through transformation
of a pilomatrixoma over a long period. They are slow-growing tumors
of the skin, which are predominantly located in the dermis and
subcutaneous fat of the neck and scalp (1). As in the present case,
histopathological analysis demonstrates positive staining of
pilomatrix carcinoma cells with β-catenin and epithelial membrane
antigen, and hyper-proliferation and atypia observed in basaloid
cells. Malignant transformation into squamous cells with
translucent appearance and necrotic areas is common.
The predominant site of pilomatrix carcinoma is the
head and neck, occurring in 60% of the patients that have been
reported in the literature. There are also studies that have
reported less common sites, including the upper extremities, torso,
lower extremities and popliteal fossa (8,9). In
the present case, the primary lesion was found in the scalp.
Studies in the relevant literature report tumors of
various sizes. The most comprehensive data regarding tumor sizes
has been provided in a study by Sau et al (1), in which 20 patients with tumors
varying in size is reported, from 1–10 cm (mean, 4.6 cm). The tumor
of the patient in the present study was 2.5 cm at its greatest
diameter.
Although pilomatrix carcinoma usually demonstrate
locally aggressive invasion and its metastatic potential is
limited, numerous cases with metastases to the lungs, bone and
lymph node have been reported. For this reason, a whole body CT
scan should be performed as a diagnostic test, in order to detect
all possible distant metastases. In the patient of the present
study, pulmonary metastasis was detected at diagnosis. As reported
in the relevant literature, the primary lesion may be a metastatic
tumor despite a negative excision margin (3), which was also observed in the patient
of the present study. Since this type of tumor has a strong
tendency for recurrence, patient follow-up should be performed
thoroughly for the timely detection of local recurrence or systemic
metastasis (3).
In conclusion, there is no standard treatment
protocol for pilomatrix carcinoma. While locally advanced
(non-metastatic) early-stage tumors are treated by surgical
resection with wide margins, various alternatives, including
chemotherapy and radiation therapy, are applied to reduce the size
of advanced stage tumors (4,5). A
literature review revealed several cases reporting the use of
various cytotoxic and immune-modulating antitumor agents (including
bleomycin, 5-fluorouracil, cisplatin, vinblastine and interferon)
(10). However, it is hypothesized
that the complete response, which was achieved in the present case,
via combination chemotherapy with oral cyclophosphamide and
etoposide for lung metastases, will provide a significant
contribution to the pilomatrix carcinoma literature.
References
|
1
|
Sau P, Lupton GP and Graham JH: Pilomatrix
carcinoma. Cancer. 71:2491–2498. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Niedermeyer HP, Peris K and Höfler H:
Pilomatrix carcinoma with multiple visceral metastases. Report of a
case. Cancer. 77:1311–1314. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gould E, Kurzon R, Kowalczyk AP and
Saldana M: Pilomatrix carcinoma with pulmonary metastasis. Report
of a case. Cancer. 54:370–372. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Veliath AJ, Reddy KS and Gomathinayagam D:
Malignant pilomatrixoma. Report of a case. Acta Radiol Oncol.
23:429–431. 1984. View Article : Google Scholar
|
|
5
|
Miyahara H, Imayama S, Hashizume T,
Takeishi M, Hori Y and Kohda H: Two cases of pilomatrix carcinoma.
J Dermatol. 17:322–325. 1990.
|
|
6
|
Omidi AA, Bagheri R and Tavassolian H:
Pilomatrix carcinoma with subsequent pulmonary metastases: a case
report. Tanaffos. 5:57–60. 2006.
|
|
7
|
Aherne NJ, Fitzpatrick DA, Gibbons D and
Armstrong JG: Pilomatrix carcinoma presenting as an extra axial
mass: clinicopathological feature. Diagn Pathol. 3:472008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kotasthane DS, Kotasthane VD and
Koteeswaran G: Pilomatrix carcinoma at the popliteal fossa: a case
report with a review of the literature. Strahlenther Onkol.
13:32012.
|
|
9
|
Bassarova A, Nesland JM, Sedloev T,
Danielsen H and Christova S: Pilomatrix carcinoma with lymph node
metastases. J Cutan Pathol. 31:330–335. 2004. View Article : Google Scholar
|
|
10
|
Tselis N, Heyd R, Vogt HG and Zamboglou N:
Pilomatrix carcinoma with lymph node and pulmonary metastases.
Strahlenther Onkol. 182:727–732. 2006. View Article : Google Scholar : PubMed/NCBI
|