Introduction
Pulmonary aspergilloma is classified as non-invasive
pulmonary aspergillosis, and is a chronic debilitating disease with
clinical symptoms that include a chronic cough, slight fever and
bloody sputum. However, a number of patients are asymptomatic
(1). A series of typical chest
computed tomography (CT) findings, including cavitary lesions with
fungus ball-like shadows, air crescent signs, meniscus signs and
double arches, are mostly caused by inflammatory lung diseases such
as mycetoma, lung abscess, pulmonary tuberculosis and
echinococcosis (2). These findings,
typical for pulmonary aspergilloma, are frequently found in the
upper lobes of the lungs (3).
Imaging examinations are therefore considered to be an essential
diagnostic tool for this condition. By contrast, it is quite rare
that metastatic lung cancer makes a cavity lesion (4). Furthermore, a fungus ball-like
structure is rarely found inside the lung cavity, particularly in
transitional cell cancer (5). The
present study reports a case of lung metastasis of transitional
cell cancer of the urothelium in an asymptomatic patient who was
initially diagnosed with pulmonary aspergilloma based on air
crescent signs in the right upper lung. The patient provided
written informed consent.
Case report
Patient history
The 67-year-old female patient of the present study
had previously been diagnosed with transitional cell cancer of the
urothelium (non-invasive, pT1N0M0), which had been treated with
total cystectomy, ileal conduit diversion and urostomy at the age
of 63. The patient had smoked 10 cigarettes a day between the ages
of 30 and 60 and had then quit. The patient had no documented
hypertension or diabetes mellitus. Subsequent to the finding of an
abnormal shadow in the right upper lung, based on X-rays taken
during the follow-up post-operative testing in April 2012, the
patient visited the Department of Respiratory and Infection Control
(Tokai University Hachioji Hospital, Tokyo, Japan) for a detailed
examination. No such shadow had been detected in the lung during
testing the previous year.
Examination
The patient’s blood pressure was 156/93, the heart
rate was 79 bpm and regular, percutaneous oxygen saturation was 95%
(room air) and there were no cardiopulmonary symptoms such as
coughs and sputum. The patient had previously undergone a urostomy
in the right lower abdomen. The blood tests, including those for
tumor markers, were normal except for a slightly elevated white
blood cell count. The aspergillus antigen and antibody were not
present, and the β-D glucan level was also normal. The sputum
culture detected no fungus or mycobacterial colonies throughout an
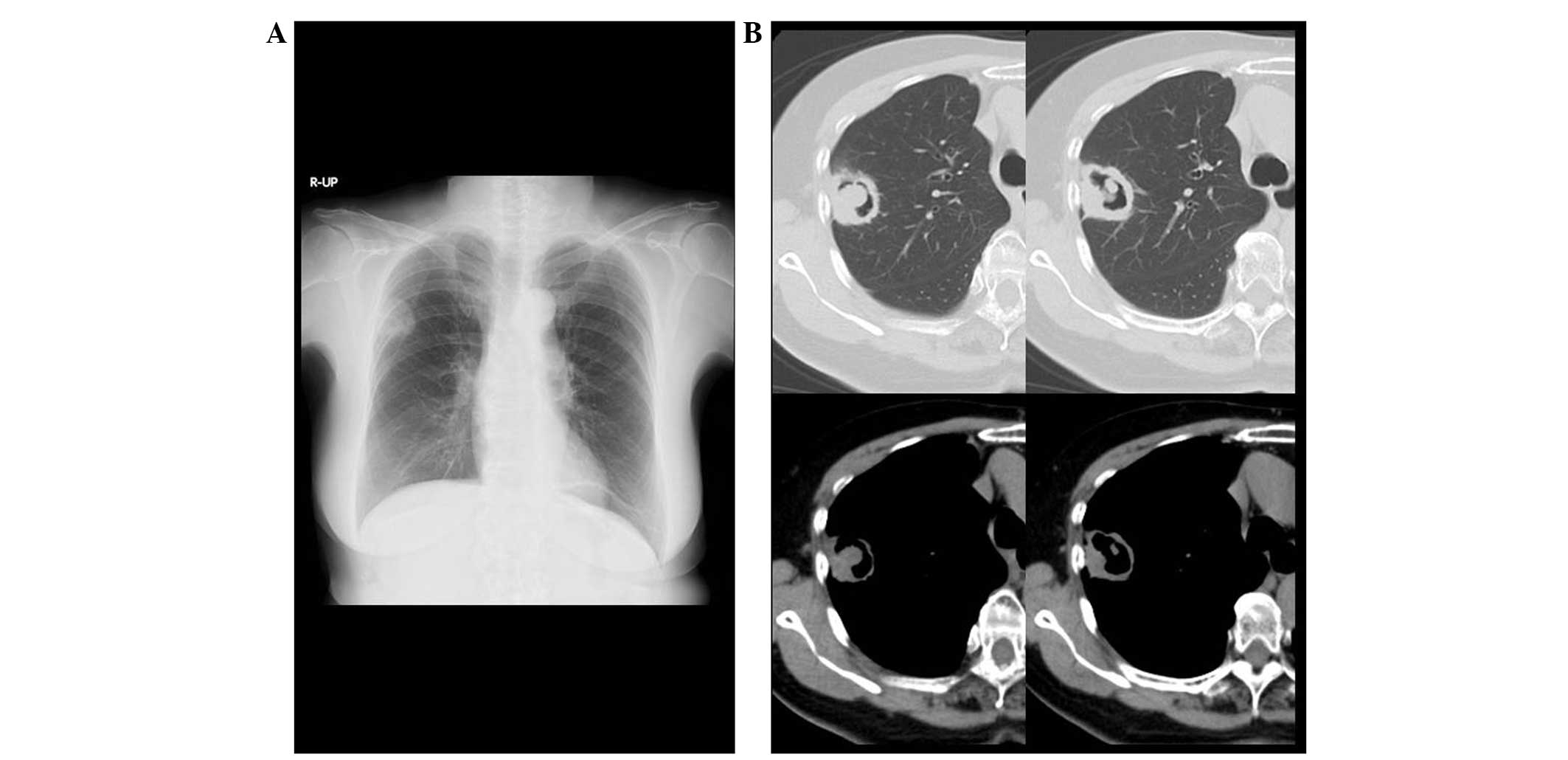
8-week incubation period. The chest CT showed a cavitary lesion
that was 3.5 cm in diameter, with fungus ball-like shadows and air
crescent signs next to the pleura in the right upper lung (Fig. 1). No nodular density was noted in
the other lung fields. No pleural effusion or enlargement of the
mediastinal lymph node was found. Based on the clinical and imaging
findings, the patient was temporarily diagnosed with aspergilloma
with a cavitary lesion and fungus ball-like shadows in the right
upper lung.
Treatment
The primary treatment of aspergilloma is surgical
removal, and the differentiation of a lung cancer is also required,
therefore, video-assisted thoracic surgery was performed in May
2012, rather than a bronchoscopy, on the basis of the patient’s
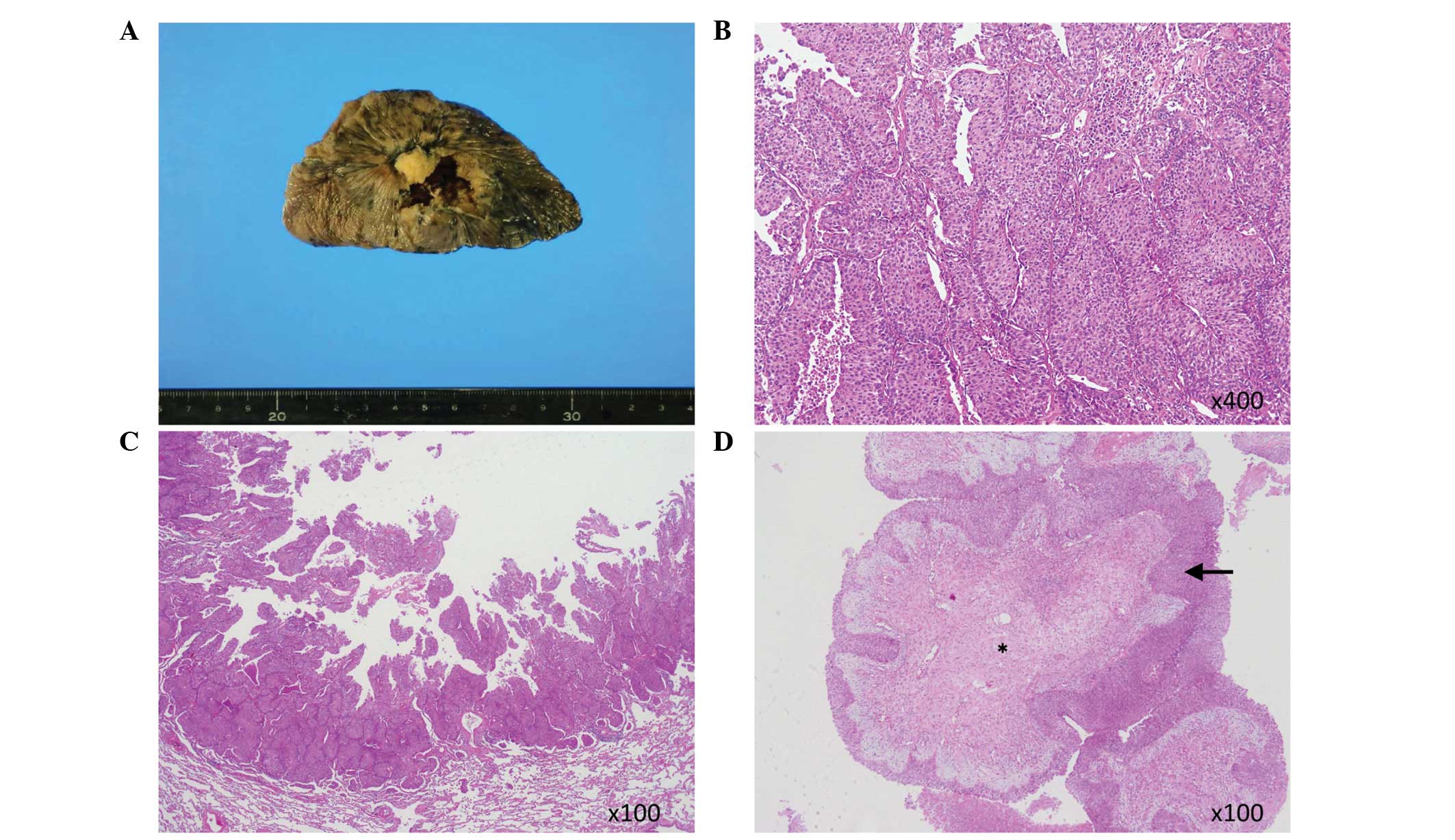
approval. The lesion was histopathologically identified as lung
metastasis of transitional cell cancer of the urothelium (Fig. 2A). The histopathology confirmed that
the tissues extended to the internal cavity wall and inner cavity,
and that they were transitional cell cancer of the urothelium
(Fig. 2B and C). The center of the
fungus ball-like structure consisted of tumor stromal tissue
covered with urothelial transitional cell cancer, not lung
interstitial tissue (Fig. 2D).
Mycetes, including Aspergillus sp., were not detected in the
isolated tissue.
Discussion
Pulmonary aspergilloma is caused by
Aspergillus sp., a naturally existing fungus (with conidia
of 2 to 4 μm in diameter). The fungus is inhaled and delivered to
the abnormal lung cavities formed due to post-tuberculosis
infection, pulmonary cysts, pulmonary fibrosis, open-chest surgery
or dilated bronchi. The fungus then saprophytically proliferates
and forms fungus balls. Aspergilloma typically affects residual
cavities subsequent to lung tuberculosis and its complications are
found in 11 to 17% of cases (6).
Immunocompetent patients with aspergilloma are generally
asymptomatic and usually aspergillus antigen-negative. Microscopic
detection of the fungus in the sputum is difficult. Air crescent
signs formed by the fungus balls in the cavitary lesion in the
upper lung are typical (2),
Isolated aspergilloma in a patient with no underlying disorders,
such as the present case, should be primarily treated with curative
surgical removal (7). Lung
disorders with cavitary lesions requiring a differential diagnosis
include lung tuberculosis, lung suppuration, pulmonary mycosis
(aspergillosis), Wegener’s granulomatosis and primary lung cancer.
However, the frequency of cavitation tumors in the lung is 2–5%;
2/3 to 4/5 of these are squamous cell cancer (8), whilst the remainder are adenocarcinoma
(9). Possible mechanisms of tumor
cavity formation include internal tissue necrosis, air trapping by
the check valve, local extension by the elastic traction and bullae
(10–13). However, there is never an apparent
structure involved in lung cavities caused by these mechanisms.
In addition, pulmonary cavitation occurs in 4% of
metastatic lung cancers (4).
Pulmonary metastases of transitional cell carcinomas are normally
found as solitary masses, multiple nodules or interstitial
micronodules (14). Transitional
cell cancer of the urothelium is only cited ~0.6% of the time as a
cause of cavitary metastases (9,14–16).
The present review of the literature classified differentiation of
cavities with fungus ball-like structures into the following 3
categories: i) Cancer-associated cavitary lesions complicated with
aspergilloma (17,18); for each case in the literature, the
cavity was made with a primary lung adenocarcinoma, the mycotic
infection happened internally and the fungus ball was created. ii)
Lung cancer with cavitary lesions, including a fungus ball-like
structure that was not a mycete (19–21);
the studies reporting this witnessed fungus ball-like structures in
cavities formed secondary to the internal necrosis of primary lung
cancer, and the internal structure and the cavity-wall tissue had
the same type of cancer cells, e.g., squamous cell carcinoma
(19,20) or adenocarcinoma (21). However, these examples involved
primary lung cancer, and not transitional cell cancer or metastatic
cancer. iii) Pulmonary metastasis of transitional cell cancer;
there are several studies in the literature on cavity formation
associated with lung metastasis of transitional cell cancer of the
urothelium (9,14–16,22–25).
However, these are all studies of the cavity without fungus
ball-like structures. Alexander et al (9) reported that the fungus ball-like
structure appeared to be in the cavity at the time of the chest
roentgenogram, but this was unclear. The present case involved lung
metastasis of transitional cell cancer of the urothelium involving
fungus ball-like structures in an isolated cavity with an air
crescent sign, closely resembling aspergilloma. The histopathology
confirmed that the tissue extended to the internal cavity wall and
the inner cavity. Metastasis of transitional cell cancer with tumor
stromal tissue around the primary lesion to the lung was indicated.
There were no necrotic tissues or fungus ball-like structures in an
intracavernous area. The central part of the fungus ball-like
structure was tumor stromal tissue, and the surrounding tissue was
a transitional cell carcinoma. The metastasized transitional cell
cancer may have grown along the internal cavity wall, covered the
later-growing tumor stromal tissue and formed the fungus ball-like
structures in the cavity.
In conclusion, metastatic lung cancer that builds a
fungus ball (aspergilloma)-like structure inside a cavity is quite
rare. Since fungus balls/aspergilloma in an immunocompetent patient
lack clinical symptoms and signs, a differential diagnosis of
cancer and a surgical approach (26) will always be crucial for
physicians.
References
|
1
|
Ueda H, Okabayashi K, Ondo K and Motohiro
A: Analysis of various treatments for pulmonary aspergillomas. Surg
Today. 31:768–773. 2001.
|
|
2
|
Abramson S: The air crescent sign.
Radiology. 218:230–232. 2001.
|
|
3
|
Kawamura S, Maesaki S, Tomono K, Tashiro T
and Kohno S: Clinical evaluation of 61 patients with pulmonary
aspergilloma. Intern Med. 39:209–212. 2000.
|
|
4
|
Grant LA, Babar J and Griffin N: Cysts,
cavities, and honeycombing in multisystem disorders: differential
diagnosis and findings on thin-section CT. Clin Radiol. 64:439–448.
2009.
|
|
5
|
Rovirosa A, Salud A, Felip E, Capdevila F,
Giralt J and Bellmunt J: Cavitary pulmonary metastases in
transitional cell carcinoma of the urinary bladder. Urol Int.
48:102–104. 1992.
|
|
6
|
Fishman AP, Elias JA, Fishman JA, Grippi
MA, Kaiser LR and Senior RM: Aspergillus syndromes, mucormycosis
and pulmonary candidiasis. Fishman’s Pulmonary Disease and
Disorders. 3rd edition. McGraw Hill; New York, NY: pp. 2265–2288.
1998
|
|
7
|
Brik A, Salem AM, Kamal AR, et al:
Surgical outcome of pulmonary aspergilloma. Eur J Cardiothorac
Surg. 34:882–885. 2008.
|
|
8
|
Kolodziejski LS, Dyczek S, Duda K,
Góralczyk J, Wysocki WM and Lobaziewicz W: Cavitated tumor as a
clinical subentity in squamous cell lung cancer patients.
Neoplasma. 50:66–73. 2003.
|
|
9
|
Alexander PW, Sanders C and Nath H:
Cavitary pulmonary metastases in transitional cell carcinoma of
urinary bladder. AJR Am J Roentgenol. 154:493–494. 1990.
|
|
10
|
Koizumi N, Akita S, Sakai K, et al:
Classification of air density areas in CT-pathologic correlation of
pulmonary adenocarcinoma. Radiat Med. 13:279–284. 1995.
|
|
11
|
Weisbrod GL, Chamberlain D and Herman SJ:
Cystic change (pseudocavitation) associated with bronchioloalveolar
carcinoma: a report of four patients. J Thorac Imaging. 10:106–111.
1995.
|
|
12
|
Weisbrod GL, Towers MJ, Chamberlain DW,
Herman SJ and Matzinger FR: Thin-walled cystic lesions in
bronchioalveolar carcinoma. Radiology. 185:401–405. 1992.
|
|
13
|
Yoshida T, Harada T, Fuke S, et al: Lung
adenocarcinoma presenting with enlarged and multiloculated cystic
lesions over 2 years. Respir Care. 49:1522–1524. 2004.
|
|
14
|
Fiorelli A, Vicidomini G, Messina G and
Santini M: Metastasis from transitional cell carcinoma of urinary
bladder as cystic pulmonary lesion. J Thorac Dis. 3:71–73.
2011.
|
|
15
|
Angulo JC, Lopez JI and Flores N:
Cavitation of lung metastases from bladder cancer. Report of two
cases. Tumori. 79:141–143. 1993.
|
|
16
|
Hisamatsu H and Yamashita S: A case of
metastatic lung cancer with cavitation due to urothelial carcinoma.
Hinyokika Kiyo. 56:269–272. 2010.(In Japanese).
|
|
17
|
Smahi M, Serraj M, Ouadnouni Y, Chbani L,
Znati K and Amarti A: Aspergilloma in combination with
adenocarcinoma of the lung. World J Surg Oncol. 9:272011.
|
|
18
|
Saleh W, Ostry A and Henteleff H:
Aspergilloma in combination with adenocarcinoma of the lung. Can J
Surg. 51:E3–E4. 2008.
|
|
19
|
Bandoh S, Fujita J, Fukunaga Y, et al:
Cavitary lung cancer with an aspergilloma-like shadow. Lung Cancer.
26:195–198. 1999.
|
|
20
|
Goto T, Kato R, Maeshima A and Oyamada Y:
Cavitary lung cancer with an aspergilloma-like shadow. J Thorac
Oncol. 5:580–581. 2010.
|
|
21
|
Wang LF, Chu H, Chen YM and Perng RP:
Adenocarcinoma of the lung presenting as a mycetoma with an air
crescent sign. Chest. 131:1239–1242. 2007.
|
|
22
|
Dougherty DW, Gonsorcik VK, Harpster LE,
Trussell JC and Drabick JJ: Superficial bladder cancer metastatic
to the lungs: two case reports and review of the literature.
Urology. 73:210.e3–210.e5. 2009.
|
|
23
|
Kurian A, Lee J and Born A: Urothelial
bladder cancer with cavitary lung metastases. Can Respir J.
18:e46–e47. 2011.
|
|
24
|
Padmore DE, Millard OH and Mason W:
Cavitary pulmonary metastases in transitional cell carcinoma. Can J
Urol. 3:251–253. 1996.
|
|
25
|
Koh KB, Rogawski K and Smith PH:
Cavitating pulmonary metastases from superficial transitional cell
carcinoma of urinary bladder. Case report. Scand J Urol Nephrol.
28:201–202. 1994.
|
|
26
|
Schweigert M, Dubecz A, Beron M, Ofner D
and Stein HJ: Pulmonary infections imitating lung cancer: clinical
presentation and therapeutical approach. Ir J Med Sci. 182:73–80.
2013.
|