Introduction
Extranodal non-Hodgkin’s lymphomas (NHLs) are
lymphomas that arise from tissues other than lymph nodes and
exhibit a higher incidence in developing countries. The
gastrointestinal tract (GIT) is the most frequent primary
extranodal localization of NHL. Primary gastrointestinal lymphoma
accounts for 4–20% of NHL cases and 30–40% of all extranodal sites,
which are predominantly of B-cell origin. Furthermore, the
intestine accounts for one-third of all GIT sites involved during
the clinical course (1).
The majority of NHL patients are diagnosed with the
complaint of diarrhea, or occur secondary to enteropathy. In
contrast to B-cell lymphoma, enteropathy-associated T-cell lymphoma
(ETCL) is a highly aggressive T-cell lymphoma with a poor prognosis
(2) and due to non-specific
clinical and endoscopic observations, early diagnosis and
appropriate treatment may be delayed (3).
The current study presents a case of intestinal
T-cell lymphoma, as well as a case of secondary B-cell lymphoma
complicated by intestinal Crohn’s disease (CD), to investigate the
clinicopathological features and immunophenotype of lymphoma and
its differentiation with CD. The study was approved by the ethics
committee of the Tianjin Medical University General Hospital.
Patients provided written informed consent.
Case report
Case one
In December 2011, a 16-year-old male with complaints
of abdominal pain and bloody diarrhea for one day was admitted to
the Tianjin General Hospital (Tianjin, China). The patient had a
history of low-grade fever and intermittent abdominal pain without
diarrhea of one month. No enlarged lymph nodes or hepatomegaly and
splenomegaly were identified by physical examination and color
Doppler ultrasonography (Prosound SSD-α5; Aloka Co., Ltd., Tokyo,
Japan) revealed no lymph node enlargement in the chest or pelvic
cavity. In addition, an abdominal computed tomography (CT) scan
revealed thickening of the wall of the initial segment of the
ascending colon without evidence of intraabdominal lymph node
enlargement. The laboratory tests revealed moderate anemia with a
hemoglobin concentration of 60–80 g/l, a normal erythrocyte
sedimentation rate and a C-reactive protein concentration of 2.3
mg/l. The acid-fast stain of the colonic biopsies was negative for
acid-fast bacilli and the purified protein derivative test was
negative with antibody positive results. The patient was also
negative for human immunodeficiency virus (HIV), cytomegalovirus
(CMV) and hepatic virus infection. However, the patient was EB-IgG
(+) with Epstein-Barr virus (EBV) negative DNA.
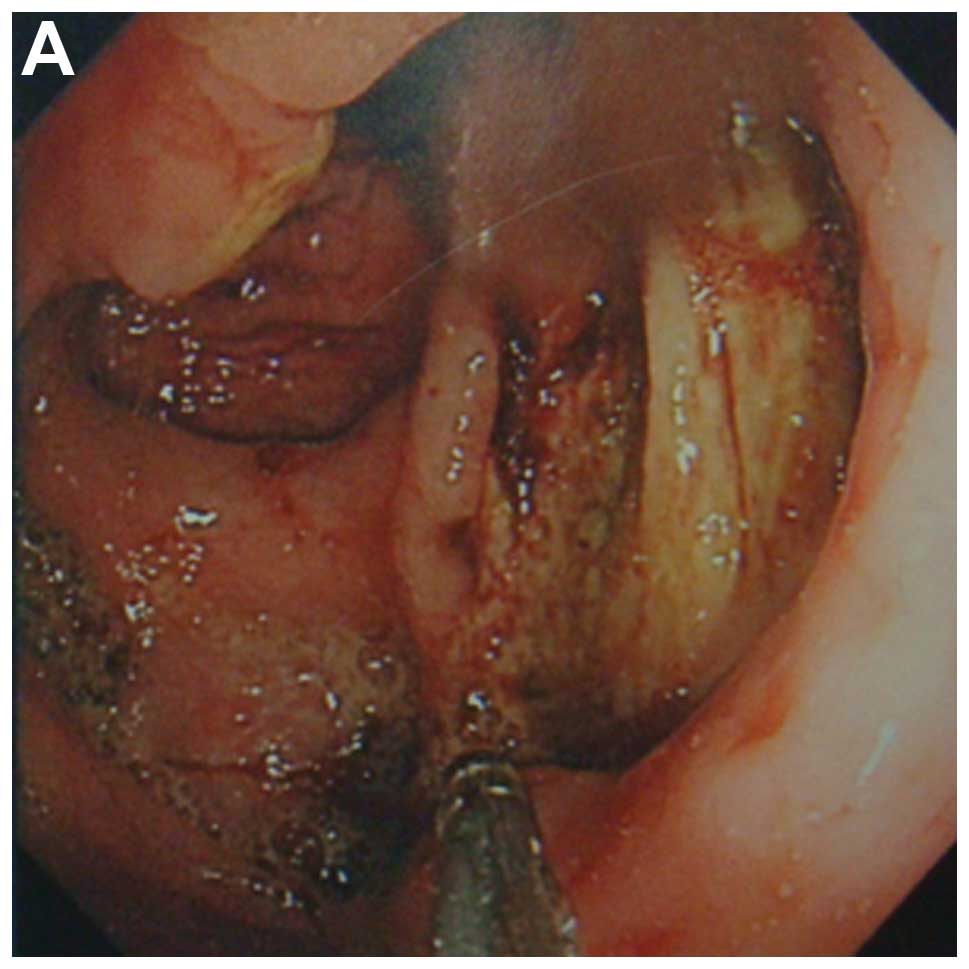
The gastroendoscopy identified chronic gastritis and
total colonoscopy on admission revealed a 2×3.5-cm ulcer in the
ileocecum with multifocal irregular ulcers distributed
circumferentially or transversely in the distal intestine (Fig. 1A). Furthermore, the histological
observations of the specimens revealed active chronic colitis
characterized by lymphocyte infiltration. Based on these results,
the patient was diagnosed with CD and mesalazine (1 g) was orally
administered three times daily as a maintenance therapy, which
improved the abdominal pain. However, the patient continued to
exhibit a fever, which fluctuated between 37 and 40°C, as well as
bloody diarrhea and the occasional presentation of bradycardia,
which suggested the possibility of malignant lesions. Four days
later, the colonoscopy was repeated and revealed an increased
number of irregular ulcers between the ileocecum and the descending
colon than previously observed.
The multifocal biopsy specimens revealed extensive
suppurative colitis accompanied by focal necrosis. Atypical
granuloma and diffuse proliferation of large-sized atypical
lymphoid cells were also identified in the section. In addition,
mixed inflammatory infiltrates containing small lymphocytes,
plasmacytes, neutrophils, eosinophils and histiocytes were
identified in the histological background. Furthermore,
immunohistochemistry confirmed these atypical cells to be positive
for CD3 and negative for CD20 (Fig.
1B), implicating T-cell lymphoma, however, a bone marrow smear
revealed no infiltrate of abnormal cells.
Thus, lymphoma was suspected and mesalazine was
replaced by prednisone (40 mg daily). However, the patient’s
symptoms persisted and liver function continued to deteriorate with
severe, ongoing hematochezia. The patient succumbed to hemorrhagic
shock two weeks following admission.
Case two
In January 2011, a 62-year-old male was admitted to
the Tianjin General Hospital (Tianjin, China) due to haematemesis
and melena with abdominal pain of one month. The patient had a
history of NHL of >10 years, which was treated by hematopoietic
stem cell transplantation (HST) followed by radiotherapy, which had
achieved a sustained response. The patient had no history of
diarrhea or malabsorption. The laboratory tests revealed mild
hypoalbuminemia and moderate anemia, however, the patient’s liver
and renal function test results were within the normal limits. In
addition, no evidence of HIV, CMV, EBV or human T-lymphotropic
virus infection was identified and among the serum tumor markers,
only ferritin was elevated to >2,000 ng/dl.
The patient had intermittent vomiting and anorexia
and contrast-enhanced CT of the abdomen and pelvis revealed
pneumatosis in the intestine and colon with segmental thickening of
the duodenum and ascending colon. In addition, the
gastroduodenoscopy revealed a huge duodenal ulcer with stricture,
which exhibited no malignant cells or characteristics of
enteropathy, as confirmed by biopsy. Masalazine (ASA; 1 g)
treatment was resumed, which allowed diarrhea control but no
obstruction recovery.
Following supportive treatment, the patient
continued to have a fever of >38°C, however, the symptoms
improved following nasojejunal nutrition tube implantation. The
enteroscopy was repeated and the multifocal biopsy specimens
revealed dense lymphocyte and plasma cell infiltration in the
mucosal layer. Additionally, immunohistochemistry and flow
cytometry revealed that the intraepithelial lymphocytes were
predominantly CD20+ and CD79a+, but negative
for CD3, CD117, CD34 and CK20. The patient was subsequently
diagnosed with B-cell lymphoma and thus received seven cycles of
chemotherapy based on the R-CHOP modality (rituximab,
cyclophosphamide, doxyorubicin, vincristine, prednisolone)
determined by the Institute of Hematology and Hospital of Blood
Diseases, Chinese Academy of Medical Sciences (Tianjin, China).
A follow-up CT scan six months after diagnosis
revealed remission of the bowel wall, however, swollen lymph nodes
in the mesentery and para-aorta were observed. The
gastroduodenoscopy identified ulcers and stricture as previously
observed and intestinal biopsies revealed lymphadenosis in the
lamina propria with CD3-positive cells and Bcl-2 expression. The
patient completed the seven cycles of chemotherapy and achieved a
complete response and remains disease free at present. The patient
continues to be monitored for disease recurrence during the
therapeutic process.
Discussion
The two cases presented in the current study
highlight the importance of correctly diagnosing NHLs of the GIT in
patients with different prognoses. The limited pathological data
obtained from the biopsies presented a challenge, however, the
clinical course provided more information.
In Asia, T-cell lymphoma predominantly arises in
young males with a poor prognosis (4). The intestinal T-cell lymphoma is
endoscopically characterized by focally, multifocally or diffusely
distributed polymorphic irregular ulcers, which most frequently
involve the ileocecum and colon. Its location in the intestine is
associated with enteropathy and develops from the intraepithelial
T-lymphocytes of the intestine (5).
ETCL is an aggressive malignancy and if left untreated, leads
invariably to mortality due to multifocal intestinal perforation
caused by refractory malignant ulcers. The first case presented in
the current study progressively deteriorated clinically with a poor
nutritional and immunological condition, which prevented the use of
adequate and opportune treatment. However, it is possible to
speculate late diagnosis and poor performance status at the time of
presentation (6). Bulky lesions,
stage, histology, immunophenotype, B-cell symptoms and lactate
dehydrogenase have all been recognized as the main prognostic
indicators and thus, the adverse prognostic features exhibited by
this patient caused the colonoscopy to be repeated and a final
diagnosis to be reached.
Notably, the patient suffered bradycardia associated
with EBV infection and according to previous studies, T-cell
lymphoma is markedly associated with EBV infection, with the
infectious frequencies ranging between 76.0 and 97.6% in certain
Asian populations (7). It has also
been recognized that EBV may exhibit a ‘start-up and promotion’
function in the pathogenesis of natural killer/T-cell lymphoma
rather than a secondary event. EBV is often implicated in the
pathogenesis of lymphoma in primary immunodeficiencies, although,
the presence of virus is not always detected, as observed in case
one of the present study (8).
Notably, Dayharsh et al (9)
revealed that irritable bowel disease patients who were treated
with thiopurines and subsequently developed lymphoma were more
likely to exhibit tumors positive for EBV.
In Asian countries, including China, intestinal
T-cell lymphoma and tuberculosis are prevalent and the incidence of
CD has also increased over recent decades. Askling et al
(10) suggested that patients with
CD carry a risk of malignant lymphoma, which is 30% higher than
that of the general population. However, differential diagnosis
based on the clinical, endoscopic and histological presentations
has become challenging. Although ulcers in lymphoma mimic those of
CD, they are transverse in direction as opposed to the usual
longitudinal ulcers observed in CD (11). Clinically, intestinal T-cell
lymphoma has an aggressive course with poor prognosis, whereas CD
exhibits a remitting/relapsing or persistent course and usually
remains for life. The administration of immunosuppressive
treatments due to a misdiagnosis of CD may delay the diagnosis of
malignant lymphoma in such patients. In the current study, it was
difficult to reach the lesion in the intestine and obtain the
specimen by forceps, however, the histological appearance was
atypical. This made it difficult to determine a diagnosis. Thus,
close endoscopic surveillance and repetitive inspections may be of
great importance in intestinal ulcerative lesions.
In long standing cases, such as the second case
presented in the current study, a primary deficiency in B-cell
function may be speculated. The majority of primary intestinal
lymphomas are of B-cell lineage and predominantly high-grade
tumors. In addition, the majority of patients exhibit B symptoms,
including weight loss and poor performance status and present with
advanced stage lymphoma (12). This
may imply that it is a defect in the immunosurveillance, in the
detection and destruction of neoplastic cells, which gives rise to
the secondary lymphoma. Case two presented in the current study was
diagnosed with duodenal B-cell lymphoma 10 years following the
initial clinical manifestation of NHL with progressive fever and
anemia, as well as clinical symptoms similar to those of
inflammatory bowel disease.
This case was also atypical, as the initial
colonoscopy and abdominal imaging were negative for any malignancy
or lesions. The patient remained disease-free following HST for a
relatively long time period. However, within several weeks, the
lymphoma had progressed with stricture extension in the duodenum.
In the first endoscopy performed on admission, although the mucosa
showed diffuse infiltration of lymphocytes with lymphoepithelial
lesions on endoscopic biopsy, immunohistochemical stains for B- and
T-cell markers were negative. However, the diagnosis of lymphoma
was suspected based on the therapeutic presentation of the patient
on 5-ASA medication. The second endoscopy was performed to achieve
a deeper view of the pathogenesis. The chemotherapy administered
for the lymphoma achieved an improved response and the clinical
symptoms subsided following the seven cycles of chemotherapy.
However, biopsy of the colon mucosa revealed mild proliferation of
small lymphocytes.
The aforementioned intestinal diffuse B-cell
lymphoma with stricture and causing abdominal pain mimicked the CD
pathogenesis. This lymphoma and is likely to be secondary to the
immunodeficiency which developed due to a pre-existing lymphoma
diagnosed >10 years earlier. Such an uncommon association must
be considered when diagnosing and treating patients (13). Previous studies have suggested that
to differentiate lymphoma clinically simulating CD, gene
rearrangement analysis may aid in the diagnosis of malignant
lymphoma when traditional histological and immunohistochemical
studies fail to provide a definitive diagnosis (14).
In conclusion, intestinal T/B-cell lymphomas may
masquerade as CD or infectious disorders. However, there may be a
potential causal association between CD and malignant lymphomas. To
address these questions, revealing the nature of lymphomagenesis in
association with inflammation is of great significance (15). The current study presents two cases
with different outcomes and the manner in which clinicians can
acknowledge the crucial point for early diagnosis or optimal
intervention must be investigated. To the best of our knowledge,
the initial clinically suspected malignant lymphoma with negative
histological evidence must not be ignored completely. When the
clinical condition appears medically unresponsive, repeated
endoscopy with deep biopsies is recommended. Furthermore,
immunophenotypic studies and gene analysis may aid clinical
decisions, as well as for surgery.
References
|
1
|
Ibrahim EM, Ezzat AA, El-Weshi AN, et al:
Primary intestinal diffuse large B-cell non-Hodgkin’s lymphoma:
clinical features, management, and prognosis of 66 patients. Ann
Oncol. 12:53–58. 2001.
|
|
2
|
Chandesris MO, Malamut G, et al:
Enteropathy-associated T-cell lymphoma: a review on clinical
presentation, diagnosis, therapeutic strategies and perspectives.
Gastroenterol Clin Biol. 34:590–605. 2010.
|
|
3
|
Zheng S, Xu H, Ouyang Q, et al: A case of
rapid growing colonic NK/T cell lymphoma complicated by Crohn’s
disease. Chin J Cancer Res. 25:119–123. 2013.
|
|
4
|
van de Water JM, Cillessen SA, Visser OJ,
Verbeek WH, Meijer CJ and Mulder CJ: Enteropathy associated T-cell
lymphoma and its precursor lesions. Best Pract Res Clin
Gastroenterol. 24:43–56. 2010.
|
|
5
|
Ko YH, Cho EY, Kim JE, et al: NK and
NK-like T-cell lymphoma in extranasal sites: a comparative
clinicopathological study according to site and EBV status.
Histopathology. 44:480–489. 2004.
|
|
6
|
Busto Bea V, Crespo Pérez L,
Rodríguez-Gandía MÁ, et al: Enteropathy-associated T-cell lymphoma:
a diagnostic challenge. Gastroenterol Hepatol. 34:686–689. 2011.(In
Spanish).
|
|
7
|
Ng SB, Lai KW, Murugaya S, et al:
Nasal-type extranodal natural killer/T-cell lymphomas: a
clinicopathologic and genotypic study of 42 cases in Singapore. Mod
Pathol. 17:1097–1107. 2004.
|
|
8
|
Bautista-Quach MA, Ake CD, Chen M and Wang
J: Gastrointestinal lymphomas: Morphology, immunophenotype and
molecular features. J Gastrointest Oncol. 3:209–225. 2012.
|
|
9
|
Dayharsh GA, Loftus EV Jr, Sandborn WJ,
Tremaine WJ, Zinsmeister AR, Witzig TE, Macon WR and Burgart LJ:
Epstein-Barr virus-positive lymphoma in patients with infammatory
bowel disease treated with azathioprine or 6-mercaptopurine.
Gastroenterology. 122:72–77. 2002.
|
|
10
|
Askling J, Brandt L, Lapidus A, et al:
Risk of haematopoietic cancer in patients with infammatory bowel
disease. Gut. 54:617–622. 2005.
|
|
11
|
Kang HY, Hwang JH, Park YS, et al:
Angioimmunoblastic T-cell lymphoma mimicking Crohn’s disease. Dig
Dis Sci. 52:2743–2747. 2007.
|
|
12
|
Radić-Kristo D, Planinc-Peraica A, Ostojić
S, et al: Primary gastrointestinal non-Hodgkin lymphoma in adults:
clinicopathologic and survival characteristics. Coll Antropol.
34:413–417. 2010.
|
|
13
|
Chera R, Gupta AA, Bailey D, et al: Small
intestinal B-cell lymphoma in a patient with lymphangiectasia
secondary to abdominal lymphangioma. J Clin Oncol. 26:675–678.
2008.
|
|
14
|
Nishimura M and Tomo K: A case of
enteropathy-associated T-cell lymphoma: diagnosis by flow
cytometric immunophenotyping and genome analysis using ascitic
fluid. Int J Clin Oncol. 16:778–782. 2011.
|
|
15
|
Malamut G, Verkarre V, Callens C, et al:
Enteropathy-associated T-cell lymphoma complicating an autoimmune
enteropathy. Gastroenterology. 142:726–729. 2012.
|