Introduction
Carcinoma of the parotid gland represents ~2% of all
head and neck cancers (1). Cancer
of the parotid gland is classified into several histological types,
and the grade of parotid cancer varies with the histological type.
As a result, certain tumors are slow growing, while others are more
aggressive. Treatment is typically surgery, which may be followed
by radiation therapy, while chemotherapy can be effective in
treating later stage cancers.
Cervical nodal metastases are a major adverse
prognostic factor (2,3). High tumor grade, extraparotid
extension, a tumor size of ≥4 cm and facial nerve involvement are
associated with nodal disease (4).
Even if the option of selective neck dissection is determined on
the basis of histological grade or primary tumor stage (T stage),
an accurate pre-operative assessment of the histological grade may
be difficult in patients with parotid carcinoma (5,6). In
previous studies, it has been reported that more than half of
T4-staged parotid carcinoma patients exhibit neck node metastasis
(6). As a result, we recommend
surgery with elective neck dissection (END) for T4-staged parotid
carcinoma. However, the treatment of T1–T3-staged patients remains
controversial.
The National Comprehensive Cancer Network guidelines
(7) show that the characteristics
of a benign tumor include a mobile superficial lobe, slow growth
and no pain, as well as a lack of or intact neck nodes. This has
shown that in addition to neck nodes and facial nerve paralysis,
clinical symptoms are also significant. The present study was
conducted to determine the correlation between clinical symptoms
and nodal metastasis and clinical outcome in patients with T1-3
parotid cancers. The specific point of interest was the
investigation of the pretreatment clinical symptoms of regional
lymph node stage (N stage), and in particular clinical N0
(cN0)-staged patients at a high risk for occult metastasis who may
potentially benefit from selective neck treatment.
Patients and methods
Population data
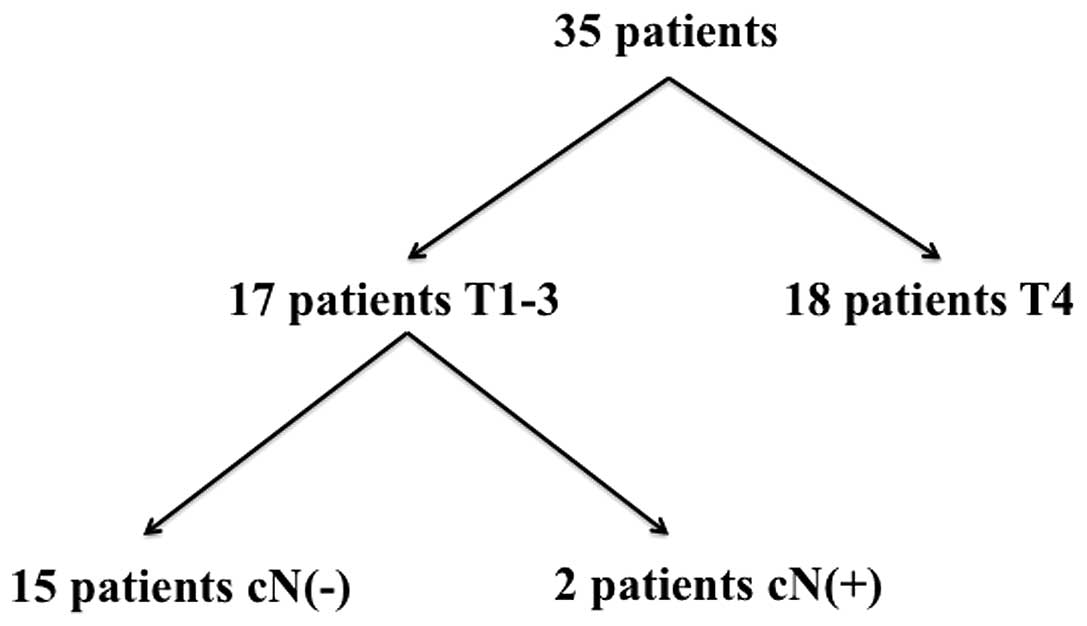
Between 2003 and 2011, 35 previously untreated
patients with carcinoma of the parotid gland received definitive
treatment at the Nagoya University Hospital (Nagoya, Japan). In the
present study, 17 T1-3-staged patients (Fig. 1, Table
I) of the 35 patients were analyzed according to the inclusion
critearia of T and N stage, including 11 males and six females who
ranged in age between 27 and 80 years. The median follow-up
duration was 47 months. T and N staging, histological type and four
clinical findings (tumor mobility, neck pain, facial palsy and skin
invasion) were analyzed. The clinical findings were compared with
the presence of lymph node metastasis and histological type grade.
Patients provided written informed consent.
 | Table IAnalysis of patients with parotid
cancer. |
Table I
Analysis of patients with parotid
cancer.
| Patient no. | Gender | Age, years | T stage | N stage |
|---|
| 1 | Male | 72 | 2 | 0 |
| 2 | Male | 65 | 3 | 0 |
| 3 | Male | 44 | 1 | 0 |
| 4 | Male | 62 | 1 | 0 |
| 5 | Female | 60 | 2 | 0 |
| 6 | Male | 53 | 2 | 0 |
| 7 | Male | 59 | 3 | 2b |
| 8 | Male | 80 | 2 | 0 |
| 9 | Male | 58 | 3 | 2b |
| 10 | Female | 42 | 2 | 0 |
| 11 | Female | 43 | 2 | 0 |
| 12 | Male | 65 | 1 | 0 |
| 13 | Male | 27 | 1 | 0 |
| 14 | Female | 75 | 1 | 0 |
| 15 | Male | 64 | 1 | 0 |
| 16 | Female | 65 | 1 | 0 |
| 17 | Female | 66 | 3 | 0 |
TN staging, histological grades and
diagnosis
Seven of the 17 patients (41.2%) were classified as
T1, six (35.3%) as T2 and four (23.5%) as T3 (Table I). In addition, 15 patients were
regarded as cN0 and two as N2b (Fig.
1). Selective neck dissection was performed for all surgical
parotid cancer patients, including stage N0 patients. The
histological grade classified patients into three groups: High,
intermediate and low grade. Of the 17 patients, two patients were
classified as high, eight (47.1%) as intermediate and seven (41.2%)
as low grade. Each histological type for all the patients and the
grade-dependent classification are shown in Table II.
 | Table IIHistological types and grade
classified into three groups. |
Table II
Histological types and grade
classified into three groups.
| Patient no. | Histological
type | Grade |
|---|
| 1 | Adenoid cystic
carcinoma | Intermediate |
| 2 | Adenoid cystic
carcinoma | Intermediate |
| 3 | Adenoid cystic
carcinoma | Intermediate |
| 4 | Mucoepidermoid
carcinoma | Low |
| 5 | Carcinoma ex
pleomorphic adenoma | Low |
| 6 | Mucoepidermoid
carcinoma | Low |
| 7 | Salivary duct
carcinoma | High |
| 8 | Epithelial
myoepithelial carcinoma | Intermediate |
| 9 | Salivary duct
carcinoma | High |
| 10 | Mucoepidermoid
carcinoma | Intermediate |
| 11 | Adenoid cystic
carcinoma | Intermediate |
| 12 | Adenocarcinoma
NOS | Low |
| 13 | Epithelial
myoepithelial carcinoma | Intermediate |
| 14 | Mucoepidermoid
carcinoma | Low |
| 15 | Adenocarcinoma
NOS | Low |
| 16 | Mucoepidermoid
carcinoma | Intermediate |
| 17 | Adenoid cystic
carcinoma | Low |
Evaluation of clinical symptoms and
findings
All the symptoms of the T1-3 N0 patients (n=15) were
analyzed, and tumor mobility was analyzed in 11 patients. As the
clinical reports of four patients did not contain adequate data,
they were excluded from the analysis. In total, five of the 11
patients exhibited poor tumor mobility, and five out of 15 patients
exhibited pain. None of the patients exhibited facial palsy or skin
invasion (Table III). The
correlation between these symptoms, and LN metastasis and
histological grade were evaluated.
 | Table IIIPatient findings and symptoms. |
Table III
Patient findings and symptoms.
| Clinical
symptoms | n |
|---|
| Pain (n=15) | 5 |
| Poor mobility
(n=11) | 7 |
| Skin invasion
(n=15) | 0 |
Treatment
All patients were initially treated by parotid
resection. Neck dissection was performed on all patients, including
N0 patients, in which levels I, II and III were resected and
examined histologically. Facial nerves without tumor invasion were
preserved when possible. Post-surgical irradiation was performed in
five patients (29.4%) with a high-grade tumor or positive surgical
margin.
Statistical analysis
The statistical analysis was performed using
Pearson’s χ2 test, and the survival expectation was
calculated by the Kaplan-Meier test. P<0.05 was considered to
indicate a statistically significant difference. All statistical
analyses were performed using JMP 8.0 software (SAS Institute,
Inc., Cary, NC, USA).
Results
Pathological staging
According to the histological examination of the
neck node at the pretreatment examination, 13 patients were
determined as pathological N0 (pN0), 15 patients as cN0 and two
patients as pN1 (Table IV).
 | Table IVN staging following pathological
examination of resected lymph node (pN). |
Table IV
N staging following pathological
examination of resected lymph node (pN).
| pN status, n |
|---|
|
|
|---|
| cN status | pN0 | pN1 | pN2 | pN3 | Total |
|---|
| cN0 | 13 | 2 | 0 | 0 | 15 |
Comparison between clinical findings and
neck metastases
Three patients presented with pain, but without neck
metastases, while two patients presented with neck metastasis. In
addition, 10 patients were without pain and neck metastasis. No
patients were identified without pain, but with neck metastasis. A
significant correlation was identified between pain and neck
metastasis (P<0.05; Table
V).
 | Table VSymptoms compared with pN status. |
Table V
Symptoms compared with pN status.
| A, Pre-operative pain
symptoms |
|---|
|
|---|
| Variable | Neck metastasis (+),
n | Neck metastasis (−),
n | Total, n | P-valuea |
|---|
| Pain | 2 | 3 | 5 | <0.05 |
| No pain | 0 | 10 | 10 | |
| Total | 2 | 13 | 15 | |
|
| B, Pre-operative
tumor mobility |
|
| Variable | Neck metastasis (+),
n | Neck metastasis (−),
n | Total, n | P-valuea |
|
| Poor mobility | 2 | 3 | 5 | 0.08 |
| Good mobility | 0 | 6 | 6 | |
| Total | 2 | 9 | 11 | |
Six patients with good tumor mobility were without
neck metastasis, while no patients were identified with neck
metastasis. Three of the 11 patients exhibited poor mobility of the
tumor without neck metastasis, and two patients with poor mobility
and neck metastasis. No significant correlation was identified
between the mobility of the tumor and neck metastasis (P=0.08;
Table V).
Comparison between clinical findings and
histological grade
Two patients with pain had a low histological grade
tumor, while three patients had an intermediate grade tumor. In
addition, five patients without pain had a low histological grade
tumor and five patients had an intermediate grade tumor. No
significant correlation was identified between pain symptoms and
the histological tumor grade (P=0.14; Table VI).
 | Table VIPain and mobility symptoms compared
with histological grade. |
Table VI
Pain and mobility symptoms compared
with histological grade.
| Grade | Pain, n | No pain, n | Poor mobility,
n | Good mobility,
n |
|---|
| Low | 2 | 5 | 2 | 4 |
| Intermediate | 3 | 5 | 3 | 2 |
| High | 0 | 0 | 0 | 0 |
Furthermore, four patients with good mobility of the
tumor had a low histological grade tumor and two patients had an
intermediate grade tumor. Two patients presented with poor tumor
mobility and a low histological grade tumor, and three with an
intermediate grade tumor. No significant correlation was identified
between the mobility of the tumor and the histological tumor grade
(P=0.37; Table VI).
Discussion
Previous studies have suggested several prognostic
factors for parotid carcinoma. In particular, histological grade
and T and N staging have been analyzed in a number of studies
(8–12). In the present study, N staging was
evaluated as a prognostic factor, and it was considered whether END
should be added to the parotid resection. It is commonly accepted
that END must be performed in patients with a histologically
high-grade malignancy, T3 or higher stage, facial palsy or
extraparotid invasion, however, the indication of neck dissection
is controversial (5).
The incidence of cervical nodal disease in parotid
carcinoma is 14–16% (13). High
tumor grade, extraparotid extension, a tumor size of ≥4 cm, pain
and facial nerve involvement are associated with nodal disease
(13,14).
Stodulski et al (15) analyzed the clinical signs and
symptoms (facial palsy, skin invasion, neck lymphadenopathy, pain,
tumor fixation and rapid tumor growth) as prognostic factors, and
as a result, concluded that facial nerve palsy and skin
infiltration are significant independent prognostic factors. In the
current study, the patient findings and symptoms were considered to
be of possible prognostic value for N status. Therefore, pain,
tumor mobility, facial palsy and skin invasion of the tumor were
analyzed.
In these analyses, only pain exhibited a significant
correlation with N status. In previous studies, pain symptoms have
shown no significant prognostic value (15). The current study is the first to
report that pain symptoms exhibit a significant correlation with
patients with or without neck metastasis. In particular, no
patients without pain were identified with neck metastasis. This
result indicated that T1-3, cN0-staged parotid carcinoma patients
without pain may be treated by parotid resection only, without END.
Other studies have also reported that pain symptoms can be divided
into two types; earache and headache (16,17).
The current study did not investigate pain in this manner and
therefore, these types of pain must be analyzed in the future.
A number of studies have also reported that
histological grade is a significant prognostic factor (1,10,11,18).
However, histological types and grades are difficult to evaluate
prior to surgery. The histological grades are often classified into
three types (high, intermediate and low grade), and have show
significant differences in prognosis in previous studies (1,19,20).
However, in the present study, no significant difference was
identified between pain symptoms and tumor grade. The lack of
high-grade tumors in T1-3, N0 patients may have led to this result
and thus, follow-up and analysis are required.
The results of the current study indicate that T1-3,
cN0-staged patients without pain exhibit no neck metastasis. It may
be possible that selective neck dissection can be omitted for T1-3,
cN0-staged patients without pain. By contrast, T1-3, cN0-staged
patients with pain may exhibit occult neck metastasis and a poor
prognosis. In conclusion, pain may be the only prognostic symptom
that is useful in the pretreatment diagnosis of parotid
carcinoma.
Acknowledgements
This study was supported by the Grants-in-Aid from
the Research Committee of the Development and Standardization of
Surgical Techniques in the Head and Neck Region, Japan (grant no.
23-A-26).
References
|
1
|
Spiro RH: Salivary neoplasms: overview of
a 35-year experience with 2,807 patients. Head Neck Surg.
8:177–184. 1986.
|
|
2
|
Carrillo JF, Vázquez R, Ramírez-Ortega MC,
et al: Multivariate prediction of the probability of recurrence in
patients with carcinoma of the parotid gland. Cancer.
109:2043–2051. 2007.
|
|
3
|
Bhattacharyya N and Fried MP: Nodal
metastasis in major salivary gland cancer: predictive factors and
effects on survival. Arch Otolaryngol Head Neck Surg. 128:904–908.
2002.
|
|
4
|
Régis De Brito Santos I, Kowalski LP,
Cavalcante De Araujo V, Flávia Logullo A and Magrin J: Multivariate
analysis of risk factors for neck metastases in surgically treated
parotid carcinomas. Arch Otolaryngol Head Neck Surg. 127:56–60.
2001.
|
|
5
|
Medina JE: Neck dissection in the
treatment of cancer of major salivary glands. Otolaryngol Clin
North Am. 31:815–822. 1998.
|
|
6
|
Kawata R, Koutetsu L, Yoshimura K,
Nishikawa S and Takenaka H: Indication for elective neck dissection
for N0 carcinoma of the parotid gland: a single institution’s
20-year experience. Acta Otolaryngol. 130:286–292. 2010.
|
|
7
|
National Comprehensive Cancer Network.
Clinical Practice Guidelines in Oncology™ Head and Neck Cancer
Version 1.2012. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
Accessed April 26, 2012
|
|
8
|
Hocwald E, Korkmaz H, Yoo GH, et al:
Prognostic factors in major salivary gland cancer. Laryngoscope.
111:1434–1439. 2001.
|
|
9
|
Lima RA, Tavares MR, Dias FL, et al:
Clinical prognostic factors in malignant parotid gland tumors.
Otolaryngol Head Neck Surg. 133:702–708. 2005.
|
|
10
|
Spiro RH, Huvos AG, Berk R and Strong EW:
Mucoepidermoid carcinoma of salivary gland origin. A
clinicopathologic study of 367 cases. Am J Surg. 136:461–468.
1978.
|
|
11
|
Hicks MJ, el-Naggar AK, Flaitz CM, Luna MA
and Batsakis JG: Histocytologic grading of mucoepidermoid carcinoma
of major salivary glands in prognosis and survival: a
clinicopathologic and flow cytometric investigation. Head Neck.
17:89–95. 1995.
|
|
12
|
Frankenthaler RA, Luna MA, Lee SS, et al:
Prognostic variables in parotid gland cancer. Arch Otolaryngol Head
Neck Surg. 117:1251–1256. 1991.
|
|
13
|
Armstrong JG, Harrison LB, Thaler HT, et
al: The indications for elective treatment of the neck in cancer of
the major salivary glands. Cancer. 69:615–619. 1992.
|
|
14
|
Kelley DJ and Spiro RH: Management of the
neck in parotid carcinoma. Am J Surg. 172:695–697. 1996.
|
|
15
|
Stodulski D, Mikaszewski B and Stankiewicz
C: Signs and symptoms of parotid gland carcinoma and their
prognostic value. Int J Oral Maxillofac Surg. 41:801–806. 2012.
|
|
16
|
Pohar S, Gay H, Rosenbaum P, et al:
Malignant parotid tumors: presentation, clinical/pathologic
prognostic factors, and treatment outcomes. Int J Radiat Oncol Biol
Phys. 61:112–118. 2005.
|
|
17
|
Rafla S: Malignant parotid tumors: natural
history and treatment. Cancer. 40:136–144. 1977.
|
|
18
|
Fordice J, Kershaw C, El-Naggar A and
Goepfert H: Adenoid cystic carcinoma of the head and neck:
predictors of morbidity and mortality. Arch Otolaryngol Head Neck
Surg. 125:149–152. 1999.
|
|
19
|
Pedersen D, Overgaard J, Søgaard H,
Elbrønd O and Overgaard M: Malignant parotid tumors in 110
consecutive patients: treatment results and prognosis.
Laryngoscope. 102:1064–1069. 1992.
|
|
20
|
Therkildsen MH, Christensen M, Andersen
LJ, Schiødt T and Hansen HS: Salivary gland carcinomas - prognostic
factors. Acta Oncol. 37:701–713. 1998.
|