Introduction
Actinomycosis is a chronic suppurative granulomatous
infection characterized by abscess and fistula formation, and
caused by aerobic or microaerophilic bacteria (1,2).
Actinomyces is a gram-positive bacteria without a capsule
and spores (3). Injury to the
mucosal barrier is of critical importance to the pathogenesis of
the disease (1), since this is the
primary entrance for actinomycosis to invade (4). Dental procedures, surgery, endoscopic
interventions and trauma may result in impairment to the mucosal
barriers (5). Poor oral hygiene,
immune-suppression and long-term intra-uterine devices are the
predisposing conditions for this infection (6,7).
Actinomycosis has been reported in patients with lymphoma,
leukemia, renal failure and renal transplantation, and long-term
steroid users due to immune-suppression (8,9).
Primary actinomycosis of the anterior abdominal wall is uncommon.
The current study presents a case of primary abdominal wall
actinomycosis in a 63-year-old male with multiple myeloma, as well
as a review of the literature. Patient provided written informed
consent.
Case report
A 63-year-old male was admitted to the Department of
Medical Oncology of the Medical Faculty of Çukurova University
(Adana, Turkey) with abdominal pain and weight loss (10 kg) for two
months. The patient had been diagnosed with multiple myeloma and
had been treated by three cycles of vincristine, doxorubicin and
dexamethasone plus zoledronic acid. A suprapubic mass (3 cm
diameter) was found by physical examination, and computerized
tomographic scans showed a cystic mass on the rectus abdominis
muscle. Repeated fine needle aspirations were non-diagnostic and a
biopsy showed fibro-adipous tissue. An excision of the mass was
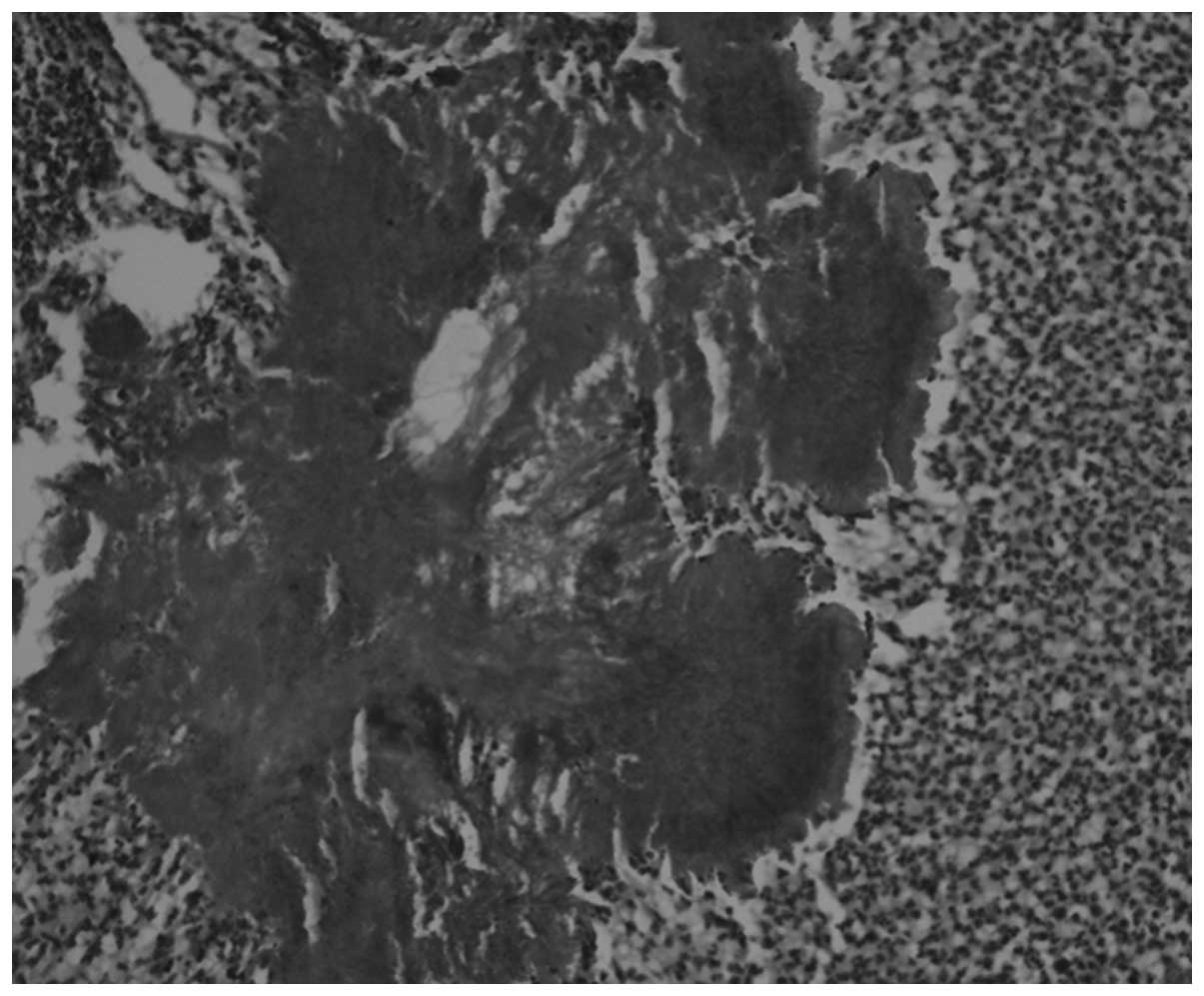
performed under general anesthesia, and a mass biopsy was reported
as an active chronic suppurative infection and actinomycosis
(Figs. 1 and 2). Parenteral ampicillin was prescribed,
which resulted in an improvement of the condition. Following the
treatment of actinomycosis, bortezomib treatment was started for
multiple myeloma.
Discussion
Actinomyces are a member of oropharyngeal
flora and Actinomyces israelii is the most frequently found
microorganism (1). A.
israelii has been identified in the female genital tract,
gastrointestinal system and bronchi, and is thought to be an
opportunistic organism (5,10,11).
Actinomyces penetrate the mucosae and promote the generation
of a slow-growing abscess, pseudo-tumor formation and fistulization
(10). Infections progress locally
rather than hematogenously (5). The
most frequently observed clinical presentations are
oral-cervico-facial, thoracic, abdominal and pelvic disease but
disseminated and central nervous system infections may be seen
(1,2,4,6,7).
Primary hepatic, splenic, gastric, pancreatic, biliary tract or
intestinal infections are rare, but these forms may be seen in
patients with underlying immune-suppressive disorders including
leukemia, auto-immune disease, alcoholism and diabetes mellitus
(11,12). In unusual cases, the disease may
present as an abdominal wall involvement simulating a soft tissue
tumor, as seen in the presented case study. Local infection of the
abdominal wall may be detected primarily or may be secondary to
clinical interventions, including surgical catheter, paracentesis
catheter, endoscopic interventions and long-term intrauterine
devices (10,13). In the present case, there were no
signs of trauma or surgical approach performed, and the patient was
therefore diagnosed with a primary abdominal wall
actinomycosis.
Abdominal actinomycosis initially presents with
insidious symptoms, and may appear to be appendicitis,
diverticulitis, intestinal perforation, trauma, intra-abdominal
foreign body, inflammatory bowel disease following colon surgery
and even may simulate malignant tumors. Pelvic actinomycosis may be
seen in those using an intra-uterine device, which can often cause
abdomino-pelvic actinomycosis (4,6,14–17).
Other risk factors include an horseshoe kidney, reno-duodenal
fistula and urachal remnants (18–21).
There are no specific clinical symptoms. Abdominal pain, cramps,
weight loss, fatigue, fever and diarrhea may be observed (13). Lymphatic dissemination is not usual
due to the diameter of the bacteria or may be detected at a late
stage of the disease (7). An acute
abdomen occurs in the presence of fistulization (10). The duration of symptoms are variable
between one month and two years (13). Generally there is a long interval
between the onset of symptoms and an accurate diagnosis (20). In the present case, the interval
between the onset of symptoms and an accurate diagnosis was two
months due to the use of steroids and tumor suspicion due to
underlying multiple myeloma.
The diagnosis of actinomycosis is based on samples
or tissue biopsies taken from lesions (4). Diagnosis is difficult due to the
anaerobic culture conditions that require a specific incubation
from fresh samples. With the use of specialized techniques, culture
positivity is <25% (13).
Histopathological examination is more useful as compared to the
other methods, for an accurate diagnosis; however, in the majority
of the cases, as in the present case, the diagnosis is verified
following surgical procedures. Fine needle aspirations are
generally insufficient, as in the present case, and therefore an
excisional biopsy is necessary (19,22).
Actinomycotic granules may be seen in hematoxylin and eosin stained
preparations (12,13,19).
The presence of sulfur granules is typical for actinomycosis but
not pathognomonic, and may be seen in Nocardia,
Streptomyces, Aspergillus and some
Staphylococcus strains (3,14,19).
Masses containing abscesses and/or low-density foci may be detected
by ultrasound or computed tomography scans, but these findings may
be wrongly reported as a malignant tumor (13,19,23).
Nonspecific inflammatory and serological markers may be elevated
but are not diagnostic (24).
Preoperative diagnosis is possible in <10% of the cases due to
the difficulty of culture conditions, unusual clinical
presentation, lack of radiological specificity and a low suspicion
index for the disease (13).
Omental solid masses must be considered in the differential
diagnosis. These masses may be associated with primary/secondary
neoplasia or inflammatory/infectious processes (chronic
appendicitis, ameboma, diverticular disease and Crohn’s disease).
The most frequently observed infection is tuberculosis (14). Additionally, inflammatory
pseudotumors, carcinomatosis and soft tissue sarcomas must
additionally be considered in the differential diagnosis (25).
The optimal therapy for actinomycosis is the wide
excision of necrotic materials and long-term antibiotic treatment
(26). Surgical debridement is
useful both for diagnosis and treatment of this condition (4,10,14).
Currently, the first choice antibiotic treatment is penicillin
(4,27). Recurrence, however, is frequent in
cases treated by antibiotics without surgical debridement.
Preoperative antibiotics may affect the width of the surgical
margins (13) and surgeons must be
aware of this entity to prevent any unnecessary procedures.
Primary abdominal actinomycosis must be considered
in cases presenting with abdominal masses and underlying
hematologic neoplasias. An asymptomatic and/or nonspecific
presentation may lead to clinical complications.
References
|
1
|
Russo TA: Agents of actinomycosis.
Principle and practice of infectious diseases. Mandell GL, Bennet
JE and Dolin R: Churchill Livingstone; New York: pp. 2924–2934.
2005
|
|
2
|
Weese WC and Smith IM: A study of 57 cases
of actinomycosis over a 36-year period. A diagnostic ‘failure’ with
good prognosis after treatment. Arch Int Med. 135:1562–1568.
1975.
|
|
3
|
Akgün Y: Actinomyces species.
Infection Diseases and Microbiology. Topçu AW, Söyletir G and
Doğanay M: 2nd edition. Nobel Medical Publishers; İstanbul: pp.
1701–1705. 2002, (In Turkish).
|
|
4
|
Hocaoğlu B, Fikretler M, Aras A and
Gürkaynak GŞ: Omental actinomycosis with abdominal wall invasion
treated by penicillin G: A case report. Klimik Journal. 24:135–137.
2011.(In Turkish).
|
|
5
|
Wang YH, Tsai HC, Lee SS, et al: Clinical
manifestations of actinomycosis in Southern Taiwan. J Microbiol
Immunol Infect. 40:487–492. 2007.
|
|
6
|
Laurent T, de Grandi P and Schnyder P:
Abdominal actinomycosis associated with intrauterine device: CT
features. Eur Radiol. 6:670–673. 1996.
|
|
7
|
Bennhoff DF: Actinomycosis: diagnostic and
therapeutic considerations and a review of 32 cases. Laryngoscope.
94:1198–1217. 1984.
|
|
8
|
Dominguez DC and Antony SJ:
Actinomyces and Nocardia infections in
immunocompromised and non immunocompromised patients. J Natl Med
Assoc. 91:35–39. 1999.
|
|
9
|
Cocuroccia B, Gubinelli E, Fazio M and
Girolomoni G: Primary cutaneous actinomycosis of the forehead. J
Eur Acad Dermatol Venereol. 17:331–333. 2003.
|
|
10
|
Acquaro P, Tagliabue F, Confalonieri G,
Faccioli P and Costa M: Abdominal wall actinomycosis simulating a
malignant neoplasm: Case report and review of the literature. World
J Gastrointest Surg. 2:247–250. 2010.
|
|
11
|
Simsek A, Perek A, Cakcak IE and Durgun
AV: Pelvic actinomycosis presenting as a malignant pelvic mass: a
case report. J Med Case Rep. 5:402011.
|
|
12
|
Wang HK, Sheng WH, Hung CC, et al:
Hepatosplenic actinomycosis in an immunocompetent patient. J Formos
Med Assoc. 111:228–231. 2012.
|
|
13
|
Filipović B, Milinić N, Nikolić G and
Ranthelović T: Primary actinomycosis of the anterior abdominal
wall: case report and review of the literature. J Gastroenterol
Hepatol. 20:517–520. 2005.
|
|
14
|
Kaya D, Demirezen Ş and Beksac MS:
Actinomycosis: An overview. Türkiye Klinikleri J Med Sci.
29:510–519. 2009.(In Turkish).
|
|
15
|
Erkaya S, Kutlar IA, Kosan I, et al:
Pelvic actinomycosis (presentation of two cases). TKlin J Gynecol
Obst. 9:284–287. 1999.(In Turkish).
|
|
16
|
Williams CE, Lamb GH and Lewis-Jones HG:
Pelvic actinomycosis: beware the intrauterine contraceptive device.
Br J Radiol. 63:134–137. 1990.
|
|
17
|
Koren R, Dekel Y, Ramadan E, Veltman V and
Dreznik V: Periappendiceal actinomycosis mimicking malignancy
report of a case. Pathol Res Pract. 198:441–443. 2002.
|
|
18
|
Dogan NU, Salman MC, Gultekin M, Kucukali
T and Ayhan A: Bilateral actinomyces abscesses mimicking pelvic
malignancy. Int J Gynaecol Obstet. 94:58–59. 2006.
|
|
19
|
Şakrak O, Müderrisoğlu I, Bedirli A, İnce
O and Canöz O: Abdominal actinomycosis appearing as an
intra-abdominal tumoral mass. Turk J Med Sci. 33:53–55. 2003.
|
|
20
|
Marella VK, Hakimian O, Wise GJ and Silver
DA: Pelvic actinomycosis: Urologic perspective. Int Braz J Urol.
30:367–376. 2004.
|
|
21
|
Gotoh S, Kura N, Nagahama K, et al:
Actinomycosis of urachal remnants. J Urol. 140:1534–1535. 1988.
|
|
22
|
Pusiol T, Morichetti D, Pedrazzani C and
Ricci F: Abdominal-pelvic actinomycosis mimicking malignant
neoplasm. Infect Dis Obstet Gynecol. 2011:7470592011.
|
|
23
|
Wagenlehner FM, Mohren B, Naber KG and
Männl HF: Abdominal actinomycosis. Clin Microbiol Infect.
9:881–885. 2003.
|
|
24
|
Das N, Lee J, Madden M, et al: A rare case
of abdominal actinomycosis presenting as an inflammatory
pseudotumour. Int J Colorectal Dis. 21:483–484. 2006.
|
|
25
|
Chaitra V, Rajalakshmi T, Mohanty S, et
al: Actinomycosis in urachal remnants: A rare cause of pseudotumor.
Indian J Urol. 27:545–546. 2011.
|
|
26
|
Ozcan R, Mammadov E, Aydın E, et al:
Actinomycosis presenting as an abdominal mass in a child. APSP J
Case Rep. 2:42011.
|
|
27
|
Mert A, Tabak F, Dumankar A, et al: A case
of pelvic actinomycosis treated with penicillin. Klimik Journal.
9:68–69. 1996.(In Turkish).
|