Introduction
Paraganglioma is a tumor that develops from the
paraganglionic system, which may be classified as a symptomatic or
asymptomatic type based on the presence or absence of endogenous
hormone secretion, respectively. Head and neck paraganglioma (HNP)
is a rare and typically asymptomatic tumor. Germline variations in
succinate dehydrogenase (SDH) genes, such as the SDHx mutation, may
be significant in sporadic HNP and familial paraganglioma. Positron
emission tomography (PET)/computed tomography (CT) have been
highlighted in the diagnosis of HNPs; however, immunohistochemical
analysis remains the primary diagnostic method. Furthermore,
complete resection of the tumor is directly associated with the
positive prognosis. In the present study, we report the case of a
50-year-old female presenting with asymptomatic HNP located between
the left common carotid artery and the left thyroid. To the best of
our knowledge, only two previous cases of HNP located at this site
have been reported (2,3). Patient provided written informed
consent.
Case report
A 50-year-old female was admitted to the Department
of Endocrinology and Metabolism, Shaoxing People’s Hospital
(Shaoxing, China) due to weight loss over a period of nine months.
The patient had no previous history of hypertension or diabetes and
no family history of paraganglioma. On admission, the patient did
not exhibit proptosis. A physical examination revealed palpable
thyroid nodules (size, 1.0×1.0 cm) with a medium texture, clear
boundaries and the nodules were moving freely during swallowing.
Furthermore, no enlarged neck lymph nodes were palpable. Auxiliary
examinations, including a chest X-ray, electrocardiogram,
gastroscopy, blood glucose testing, cancer screening panels,
thyroid function panels and parathyroid hormone measurements, did
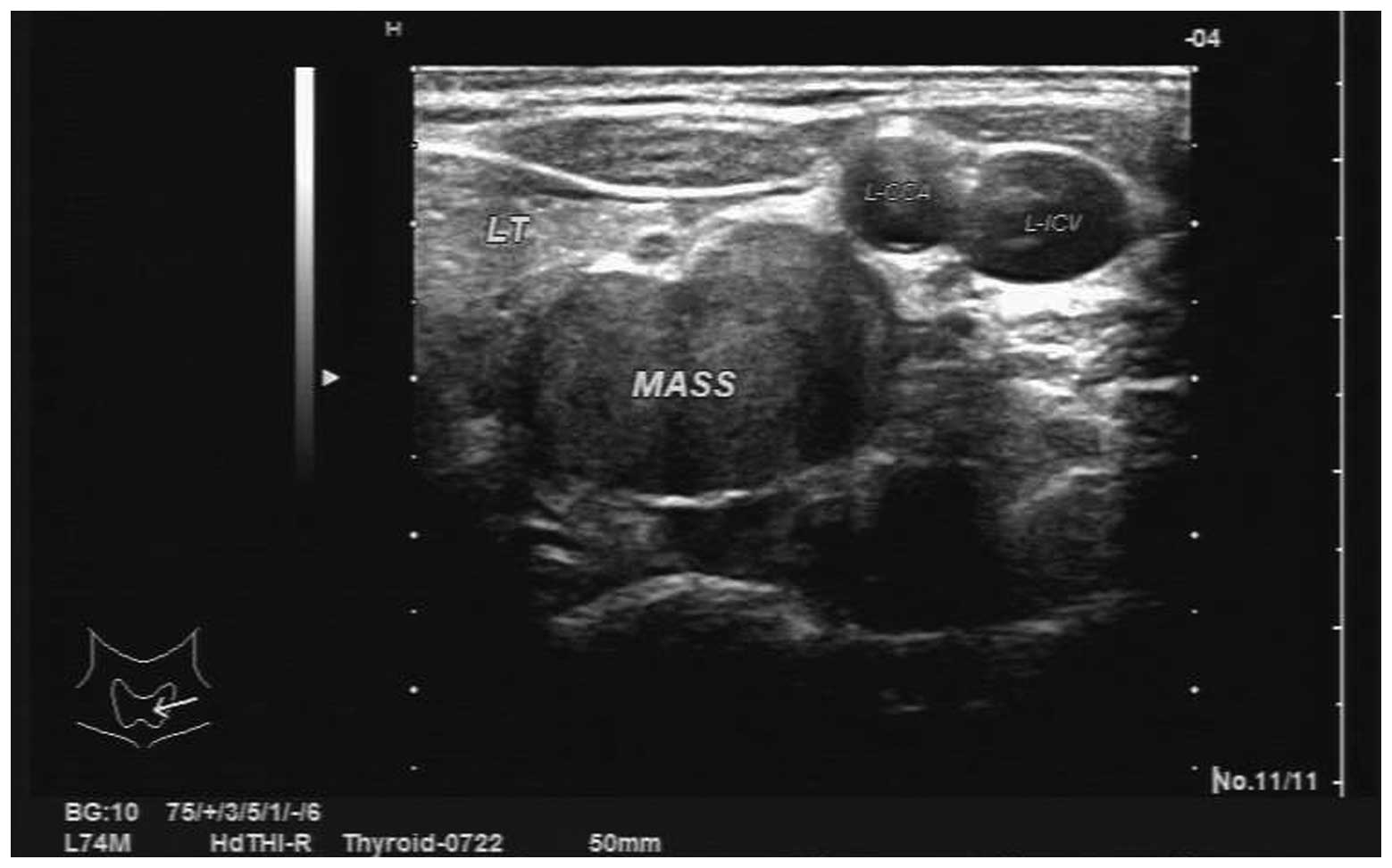
not reveal any abnormalities. However, an ultrasound scan
identified multiple bilateral thyroid nodules and a hypoechoic mass
in the left side of the neck, which was considered to be a
neurogenic tumor (Fig. 1). Plain
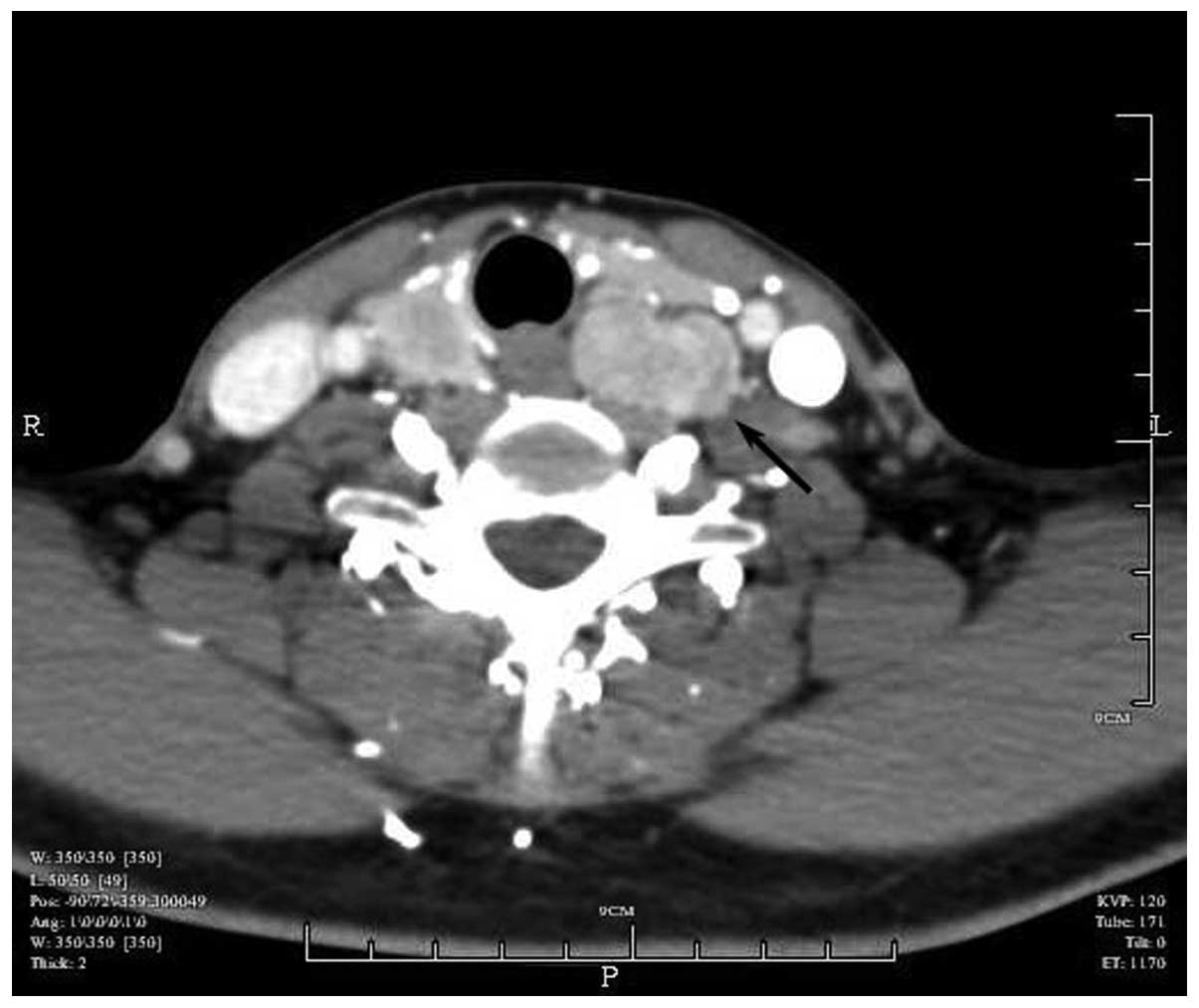
and enhanced CT scanning revealed a soft tissue mass in the left
posterior side of the thyroid (Fig.
2). The patient was transferred to the Department of Breast and
Thyroid Surgery (Shaoxing People’s Hospital, Shaoxing, China)
following identification of the thyroid nodules and a hypoechoic
mass in the left side of the neck. Bilateral partial thyroidectomy
combined with a resection of the left neck mass was performed under
general anesthetic. During surgery, multiple solid, encapsulated
masses of varying sizes (diameter, 0.5–1.0 cm) were observed in the
two sides of the thyroid; a pale red solid mass (size, ~2.5×2.0 cm)
with a rich blood supply was identified posterior to the middle and
lower poles of the left thyroid gland, which bled and shrank
following compression. The encapsulated mass had a gray/red
appearance along the resected surface, without adherence to the
left thyroid or adjacent vessels, and was located deep in the
prevertebral fascia. Intraoperative analysis of frozen sections of
the mass revealed a nodular goiter with fibrotic nodules; the left
neck mass was considered to be a paraganglioma (size, 2.4×2.2×1.2
cm). The surgery was successfully completed and postoperative
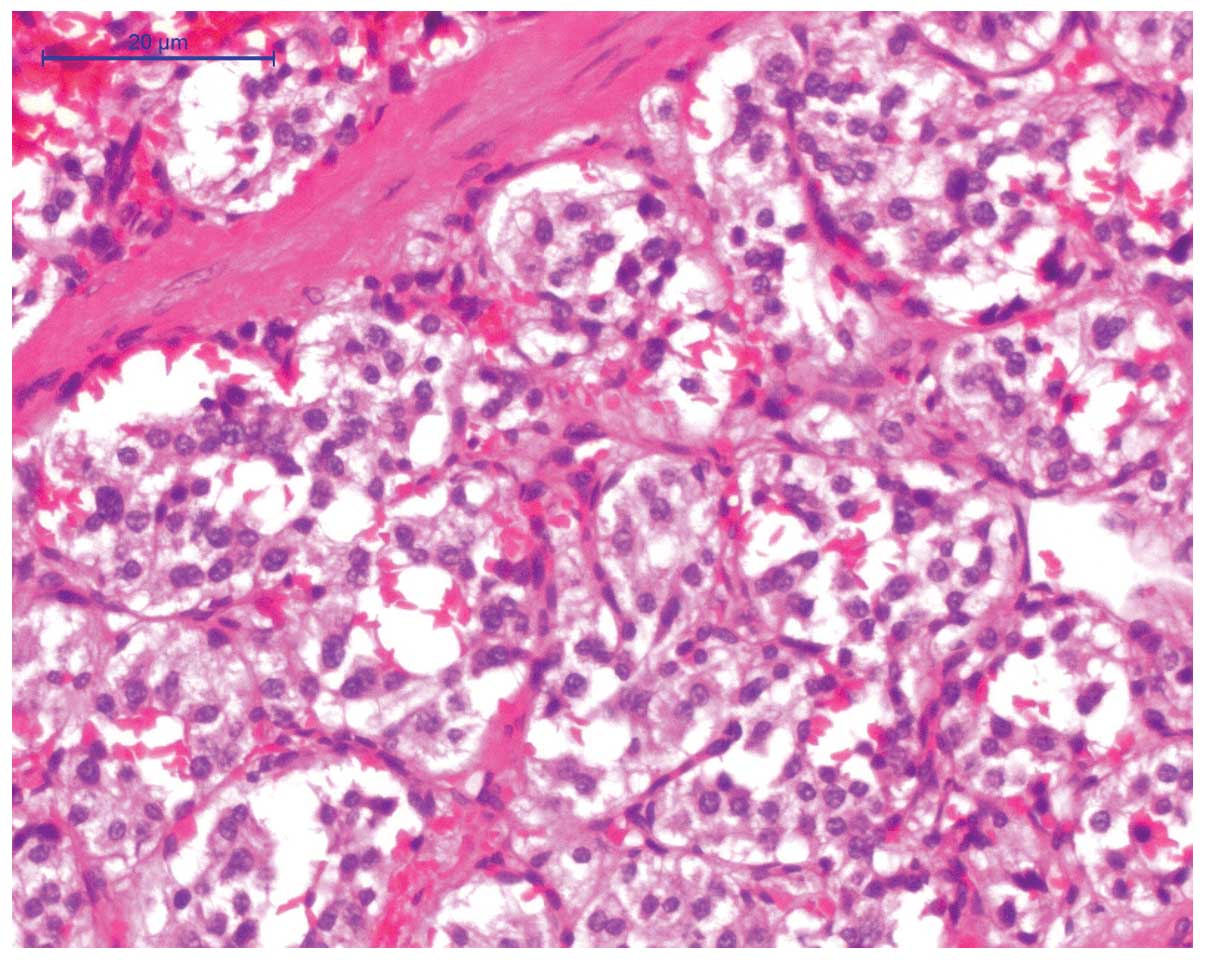
recovery was uneventful with no complications. Light microscopy
(DM3000; Leica, Manheim, Germany) revealed that the tumor consisted
of epithelial main cells in a nest-like structure on a
paraffin-embedded section, which were separated by enlarged
fibrovascular stroma (Fig. 3).
Supporting cells were observed surrounding the tumor and reactive
hyperplasia was observed in three lymph nodes. Pathological
diagnosis confirmed nodular goiter with interstitial collagen and
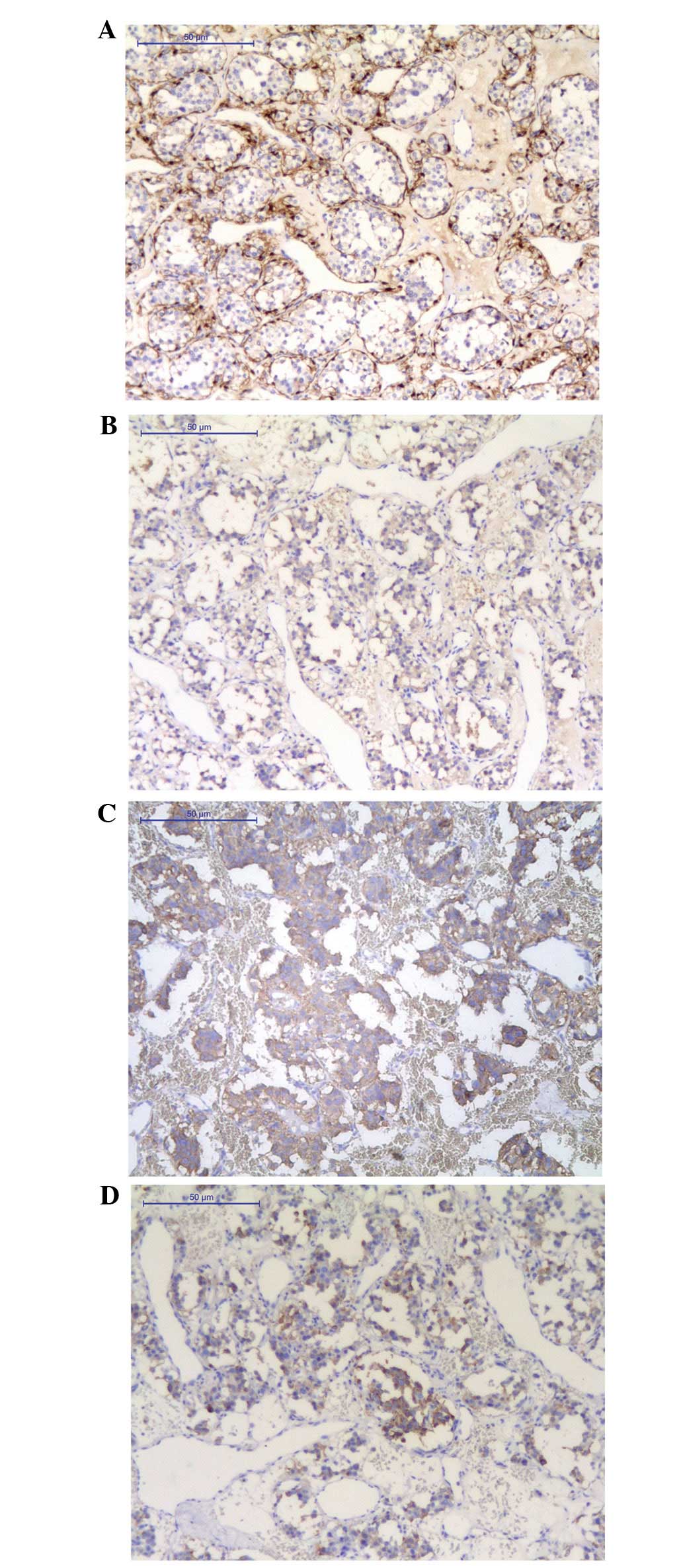
paraganglioma in the left side of the neck. Immunohistochemical
analysis revealed that neuron-specific enolase (NSE), S-100
supporting cells, vimentin, smooth muscle actin blood vessels,
synaptophysin (Syn) and chromogranin A (CgA) were positively
stained (Fig. 4), while
cytokeratin, DM, epithelial membrane antigen (EMA), Ki-67, nuclear
factor, myelin basic protein and p53 were negatively stained
(Table I). The postoperative
recovery was uneventful and follow-up enhanced abdominal CT and
adrenal ultrasound examinations identified no abnormalities. The
patient was followed up for 12 months and her condition was
considered to be very satisfactory.
 | Table IImmunohistochemical analysis of
antigen expression. |
Table I
Immunohistochemical analysis of
antigen expression.
| Antigen | Staining |
|---|
| NSE | Positive |
| S-100 | Positivea |
| VM | Positive |
| SMA | Positive |
| Syn | Positive |
| CgA | Positive |
| CK | Negative |
| DM | Negative |
| EMA | Negative |
| Ki-67 | Negative |
| NF | Negative |
| MBP | Negative |
| p53 | Negative |
Discussion
Originating from the parasympathetic ganglia,
paragangliomas consist of either chromaffin or non-chromaffin
cells, which are defined by the response of the main cells to
chromium salts (1). The tumor may
be classified as a symptomatic or asymptomatic type based on the
presence or absence of endogenous hormone secretion, respectively.
HNPs are rare, typically asymptomatic and often identified due to
compression of the surrounding tissues or during a physical
examination. This report presents a case of asymptomatic
paraganglioma located between the left common carotid artery and
the left thyroid. To the best of our knowledge, only two cases of
paraganglioma located at this site have previously been reported
(2,3).
In the majority of cases, paragangliomas are
sporadic without an obvious family history, although there have
been an increasing number of reports based on hereditary cases.
Baysal et al (4) first
reported the association between SDH subunit D germline mutations
and hereditary paragangliomas. Using candidate gene analysis,
subsequent studies confirmed the correlation of SDH subunit B
(5) and C (6) germline mutations with the occurrence
of hereditary paragangliomas, however, not with that of sporadic
paragangliomas (7).
CT and/or magnetic resonance imaging (MRI) are
significant in the preoperative diagnosis of paragangliomas
(8) and PET/CT scans have also been
highlighted for the diagnosis and prognosis of this disease. In a
study of 26 cases of HNP diagnosed with PET/CT scanning, Sharma
et al (9) reported that
68Ga-DOTA-NOC PET/CT was superior to 131I-meta-iodobenzylguanidine
imaging and conventional CT/MRI in terms of baseline assessment.
Gabriel et al (10)
confirmed that, regardless of the tumor gene status,
6-(18)F-fluoro-l-dopa PET provided sensitive functional imaging for
HNPs. In addition, the preoperative use of fine needle aspiration
(FNA) biopsy (11) has been
reported, although its specific role has not been clearly
demonstrated. As paragangliomas are hypervascular with a high risk
of hematoma following aspiration, further studies are required to
support the clinical application of FNA.
The pathological characteristics of paragangliomas
include ovoid, marginally lobulated, elastic masses with a smooth
surface, incomplete capsules and local infiltration in the majority
of cases. The surgical surface appears to be a gray/brown/red
color, with a rich supply of blood vessels. Under a light
microscope, the tumor consists of epithelial main cells arranged in
a nest-like structure, which are separated by abundant enlarged
fibrovascular stroma. Although supporting cells are visible around
the nest, nerve fibers are difficult to observe (12). Immunohistochemical markers
associated with neuroendocrine tumors, such as Syn, CgA and NSE,
were positively stained. S-100 staining showed the supporting cells
clearly and negative expression of EMA, cluster of differentiation
10 and renal cell carcinoma (RCC) aided the exclusion of negative
metastatic RCC. Therefore, a negative expression of epithelial
markers may exclude epithelial malignancies. Currently, there is no
definitive histological evidence to distinguish benign from
malignant paragangliomas. The presence of atypia in tumor cells
does not necessarily signify malignancy, however, evident necrosis
and frequent mitotic figures in the center of the tumor cell nest,
vascular invasion, as well as the capsular status are all useful in
predicting a possible malignancy. Moreover, a lack of S-100 may
indicate a strong invasive potential of paragangliomas (13). Generally, it is accepted that
malignant paragangliomas are associated with lymph node or distant
metastases.
Surgery remains the common treatment method for
paragangliomas and complete resection of the lesions is the most
critical component for remission. Our patient had an intact tumor
capsule without significant adhesions to the surrounding tissues
and surgery was successfully completed. Although adjuvant
radiotherapy may be included for malignant paragangliomas,
overtreatment and undertreatment are common in certain cases as no
standard criteria are currently available (14). As a result, the treatment strategies
for paragangliomas require careful development by a
multidisciplinary team (15).
In conclusion, the present report described a case
of a paraganglioma in a rare location between the thyroid gland and
the left common carotid artery. With the continuous development of
immunohistochemical technology and the discovery of unusually
located paragangliomas, the clinical data provided in this report
will contribute to a greater understanding of this type of
tumor.
References
|
1
|
Strosberg JR: Update on the management of
unusual neuroendocrine tumors: pheochromocytoma and paraganglioma,
medullary thyroid cancer and adrenocortical carcinoma. Semin Oncol.
40:120–133. 2013.
|
|
2
|
Pinto FR, Capelli Fde A, Maeda SA, et al:
Unusual location of a cervical paraganglioma between the thyroid
gland and the common carotid artery: case report. Clinics (Sao
Paulo). 63:845–848. 2008.
|
|
3
|
Schmit GD, Gorman B, van Heerden JA and
Gharib H: Inferior laryngeal paraganglioma mimicking a primary
thyroid tumor. Endocr Pract. 12:432–435. 2006.
|
|
4
|
Baysal BE, Ferrell RE, Willett-Brozick JE,
et al: Mutations in SDHD, a mitochondrial complex II gene, in
hereditary paraganglioma. Science. 287:848–851. 2000.
|
|
5
|
Astuti D, Latif F, Dallol A, et al: Gene
mutations in the succinate dehydrogenase subunit SDHB cause
susceptibility to familial pheochromocytoma and to familial
paraganglioma. Am J Hum Genet. 69:49–54. 2001.
|
|
6
|
Niemann S and Müller U: Mutations in SDHC
cause autosomal dominant paraganglioma, type 3. Nat Genet.
26:268–270. 2000.
|
|
7
|
Bayley JP, van Minderhout I, Weiss MM, et
al: Mutation analysis of SDHB and SDHC: novel germline mutations in
sporadic head and neck paraganglioma and familial paraganglioma
and/or pheochromocytoma. BMC Med Genet. 7:12006.
|
|
8
|
Havekes B, King K, Lai EW, et al: New
imaging approaches to phaeochromocytomas and paragangliomas. Clin
Endocrinol (Oxf). 72:137–145. 2010.
|
|
9
|
Sharma P, Thakar A, Suman KS, et al:
68Ga-DOTANOC PET CT for baseline evaluation of patients with head
and neck paraganglioma. J Nucl Med. 54:841–847. 2013.
|
|
10
|
Gabriel S, Blanchet EM, Sebag F, et al:
Functional characterization of nonmetastatic paraganglioma and
pheochromocytoma by F-FDOPA PET: focus on missed lesions. Clin
Endocrinol (Oxf). 79:170–177. 2013.
|
|
11
|
Schreiner AM, Fried K and Yang GC:
Interconnecting cytoplasmic processes on fine-needle aspiration
smears of carotid body paraganglioma. Diagn Cytopathol. 38:507–508.
2010.
|
|
12
|
Tischler AS: Pheochromocytoma and
extra-adrenal paraganglioma: updates. Arch Pathol Lab Med.
132:1272–1284. 2008.
|
|
13
|
Thompson LD: Pheochromocytoma of the
Adrenal gland Scaled Score (PASS) to separate benign from malignant
neoplasms: a clinicopathologic and immunophenotypic study of 100
cases. Am J Surg Pathol. 26:551–566. 2002.
|
|
14
|
Offergeld C, Brase C, Yaremchuk S, et al:
Head and neck paragangliomas: clinical and molecular genetic
classification. Clinics (Sao Paulo). 67:19–28. 2012.
|
|
15
|
Lahlou-Laforêt K, Consoli SM, Jeunemaitre
X, et al: Presymptomatic genetic testing in minors at risk of
paraganglioma and pheochromocytoma: our experience of oncogenetic
multidisciplinary consultation. Horm Metab Res. 44:354–358.
2012.
|