Introduction
Despite advances in detection and therapeutic
strategies, breast cancer remains the most common type of
malignancy in females worldwide (1). MCF-7 (estrogen receptor (+),
progesterone receptor (+), human epidermal growth factor receptor 2
(−) and wild-type p53) is one of the most representative
non-invasive breast cancer cells in vitro. Doxorubicin, as
an anthracycline antibiotic, possesses the ability to intercalate
into DNA and block DNA topoisomerase II activity resulting in DNA
double-strand breaks (2). Due to
its high cytotoxic action towards tumor cells, doxorubicin-based
chemotherapy remains a central component of current treatments for
non-invasive breast cancer. Furthermore, doxorubicin is used as an
adjunct to surgery in the majority of cases (3).
The ataxia telangiectasia mutated (ATM) protein is
considered to directly or indirectly regulate the repair of
double-strand breaks via cell cycle checkpoint control, and
inhibition or absence of ATM increases radiosensitivity, indicating
that it is critical for the cellular response to DNA damage
(4,5). In a previous study, KU60019 was
identified as a potent and specific ATP competitive inhibitor of
ATM with regards to the inhibition of other members of the
phosphoinositide 3-kinase family. KU60019 was shown to increase the
sensitivity of breast cancer cells to ionizing radiation (IR),
alter their cell cycle profile and inhibit the phosphorylation of a
panel of ATM targets (6).
The current study was designed as a preclinical
evaluation of the ATM inhibitor, KU60019, to investigate whether
the compound affects cell physiological activities and strengthens
the efficacy of doxorubicin-induced DNA damage.
Materials and methods
KU60019
The highly specific and potent ATM inhibitor,
KU60019, was purchased from Selleck Chemicals (Houston, TX, USA).
KU60019 was dissolved in 100% dimethyl sulfoxide (DMSO) and stored
at −20°C.
Cell culture
The MCF-7 human breast cancer cell line was obtained
from the American Type Culture Collection (Rockville, MD, USA). The
cells were cultured in Dulbecco’s modified Eagle’s medium
(Gibco-BRL, Grand Island, NY, USA) and supplemented with 10% fetal
bovine serum (Gibco-BRL) in a humidified atmosphere of 5%
CO2 at 37°C.
Cell survival analysis
Cells were seeded into 96-well plates
(6×103/well) and following attachment for 12 h, the
cells were exposed to 0.25 mg/l doxorubicin (Zhejiang Hisun
Pharmaceutical Co., Ltd., Taizhou, China) and/or 3 μM KU60019
(Selleck Chemicals) for 24 h. The Cell Counting kit-8 (CCK-8) assay
(Dojindo, Kunamoto, Japan) was used to determine relative cell
growth, according to the manufacturer’s instructions. The data
shown are representative of three independent experiments.
Apoptosis assay
The MCF-7 cells were incubated with 0.25 mg/l
doxorubicin and/or 3 μM KU60019 for 24 h. In total,
1×106 cells were later collected and washed twice with
ice-cold phosphate-buffered saline (PBS). Cells were dual-stained
using fluorescein isothiocyanate Annexin V apoptosis detection kit
I (BD Biosciences, Franklin Lakes, NJ, USA), according to the
manufacturer’s instructions. The stained cells were immediately
analyzed using a flow cytometer (BD Accuri™ C6; BD
Biosciences).
Cell cycle analysis
The cells were collected, washed twice with PBS
supplemented with 1 ml ethanol (75%) and maintained at −20°C
overnight. The cells were resuspended with PBS supplemented with
propidium iodide and RNase A, incubated for 30 min at 37°C and
analyzed using flow cytometry.
In vitro migration and invasion
assays
For the migration assays, the blank cells or chemo
survival fractions (MCF-7 cells) were detached and aliquots of
2×105 cells/ml were plated onto the inserts of the 8-μM
pore size Transwell chambers (Corning Inc., Corning, NY, USA). For
Transwell invasion assays, 1×106 cells were plated onto
inserts containing a polycarbonate membrane with a thin layer of BD
Matrigel matrix (BD Biosciences). Migration and invasion were
detected 24 h later by counting the number of cells that had
migrated or invaded through the membrane.
Western blot analysis
Cells were extracted and prepared in modified radio
immunoprecipitation assay buffer (Beyotime, Jiangsu, China).
Proteins were separated by 10% SDS-PAGE, transferred to
polyvinylidene difluoride membranes (Bio-Rad, Hercules, CA, USA)
and incubated with primary antibodies against human BCL-2 (1:500;
Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA),
phosphorylated (p)-p53 (Ser15; 1:1,000; Cell Signaling Technology,
Inc., Danvers, MA, USA), p53 (1:500; Bioworld Technology, Inc., St.
Louis Park, MN, USA) and phosphorylated (p)-Akt (Ser473), ATM and
E-cadherin (all 1:1,000; Cell Signaling Technology, Inc.) overnight
at 4°C. The horseradish peroxidase-conjugated secondary antibody
was purchased from DakoCytomation (Glostrup, Denmark).
Immunoreactive bands were visualized by chemiluminescence with
pierce enhanced chemiluminescence detection reagent (Millipore,
Billerica, MA, USA) and β-actin (1:4,000; Bioworld Technology,
Inc.) served as an internal loading control. Data shown are
representative of individual experiments that were repeated at
least three times.
Statistical analysis
The results presented are the average of at least
three experiments each performed in triplicate with standard
errors. Statistical analyses were performed by analysis of
variance, followed by unpaired one- or two-tailed t-tests, using
the SPSS 20.0 statistical package (IBM, Armonk, NY, USA). P<0.05
was considered to indicate a statistically significant
difference.
Results
Effect of KU60019 on cell viability in
MCF-7 cells
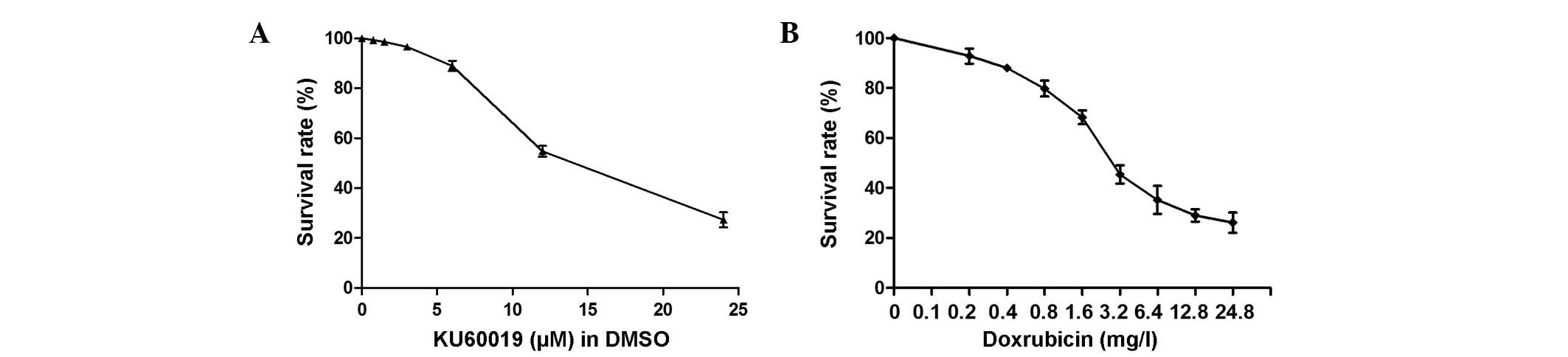
Results of the dose-dependent study are shown in
Fig. 1A and indicated that KU60019
has an antiproliferative effect on MCF-7 cells, as assessed by
CCK-8 assay. Treatment with KU60019 for 24 h significantly
suppressed the proliferation of MCF-7 at concentrations of >6 μM
(P<0.05, data not shown).
KU60019 is a potent chemosensitizer in
combination with doxorubicin
A gradual decrease in cell survival was identified
in response to increased concentrations of doxorubicin (Fig. 1B). The IC50 values of
doxorubicin and KU60019 were 2.5 mg/l and 12.4 μM, respectively.
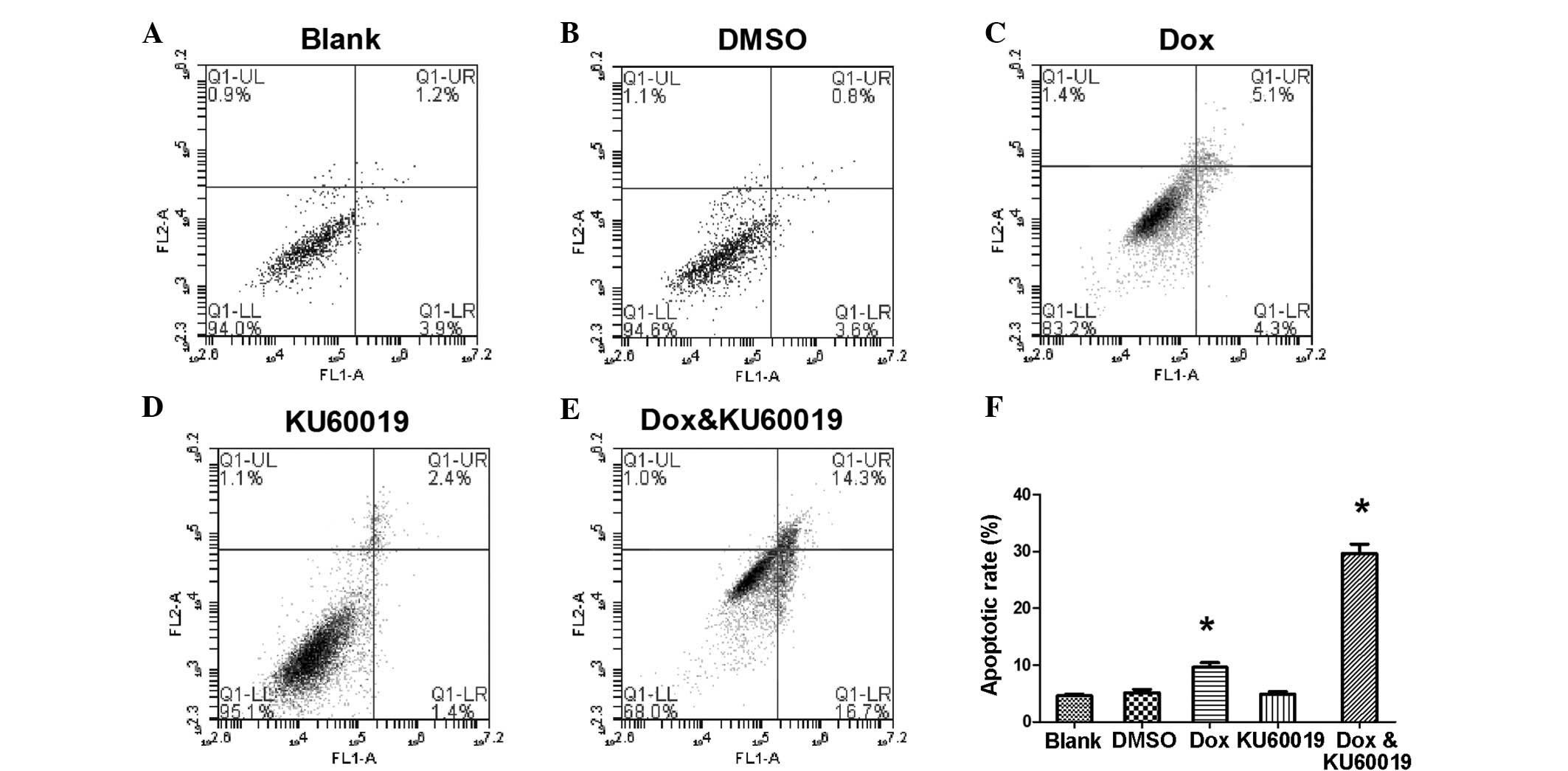
The response to a fixed concentration of each compound was
subsequently investigated (Fig. 2).
When the apoptosis rate of MCF-7 cells was measured, it appeared
that the cells were much more sensitive to the combination of the
two compounds rather than KU60019 or doxorubicin alone. At a
concentration of 0.25 mg/l, doxorubicin induced only 9.6±0.83% of
cell apoptosis (Fig. 2C).
Similarly, no marked difference was identified between the cells
that were treated with KU60019 at a concentration of 3 μM and the
control groups (Fig. 2A, B and D).
However, combining the two inhibitors significantly increased the
chemosensitization of MCF-7 cells, which indicated an advanced role
of doxorubicin-based chemotherapy in non-invasive breast cancer
(Fig. 2E and F).
Blocking the cell cycle may be a key
mechanism of KU60019 at a concentration of 3 μM
It was of interest in the present study whether
KU60019 induced alteration of the cell cycle in MCF-7 cells. The
results presented in Table I
demonstrate that, compared with the control groups, the vast
majority of MCF-7 cells were arrested at G1/S phase
(62.2±2.9%) following treatment with 3 μM KU60019. In the
combination group, the two compounds caused
G1/G2 phase arrest (G1/S,
41.8±3.1%; and G2/M, 35.5±2.4%).
 | Table ICell cycle distribution in MCF-7
cells. |
Table I
Cell cycle distribution in MCF-7
cells.
| Phase | Blank, % | DMSO, % | Dox, % | KU60019, % | Dox and KU60019,
% |
|---|
|
G0G1 | 44.3±0.96 | 43.8±2.12 | 48.4±2.07a | 69.2±0.93a | 54.8±1.08a |
| S | 34.0±0.33 | 34.2±0.54 | 21.1±0.76 | 8.7±0.22 | 13.5±0.93 |
| G2/M | 21.9±1.07 | 21.7±1.82 | 30.4±1.03a | 21.6±0.94 | 30.1±1.02a |
KU60019 affects the ability of migration
and invasion in the MCF-7 cell line in vitro
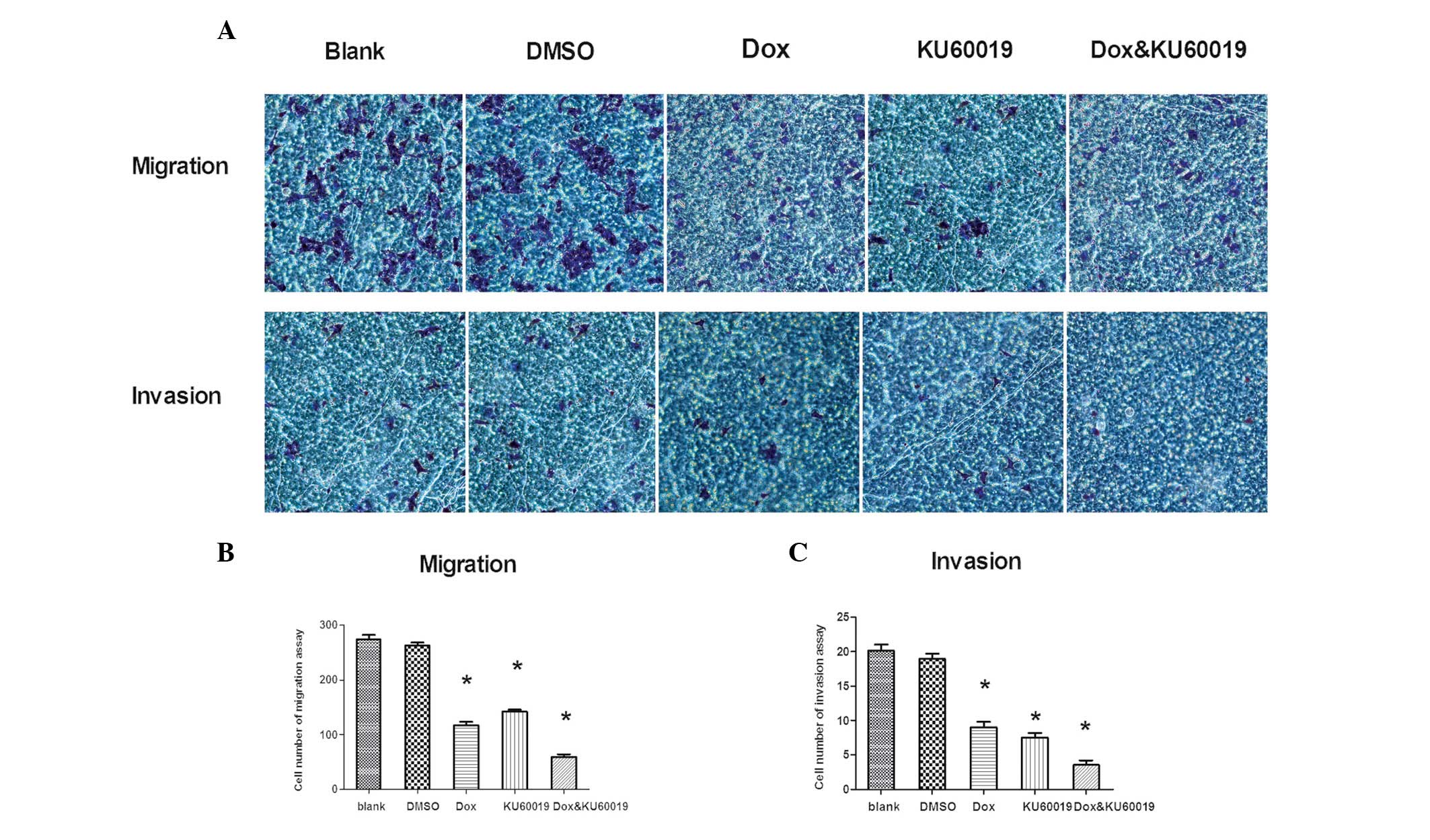
It was hypothesized that KU60019 may restrict MCF-7
cell migration and invasion. Thus, migration and invasion assays of
MCF-7 cells were performed and established in vitro
conditions (Fig. 3A). Fewer
KU60019-treated cells crossed the membrane compared with control
group cells (KU60019 group [142.2±3.4] vs. blank [274±7.3] and DMSO
[263±5.1] groups; P<0.01, Fig.
3B). Compared with the control groups, following treatment with
KU60019, the number of MCF-7 cells that invaded the Matrigel-coated
filter was significantly lower (KU60019 group [7.5±0.6] vs. blank
[19.0±0.7] and DMSO [20.1±0.9] groups; P<0.01, Fig. 3C). In addition to its negative
effects on migration and invasion, KU60019 weakened these abilities
when it was combined with doxorubicin at a concentration of 0.25
mg/l. For the migration assay, the cell numbers were; doxorubicin
group (117±6.2) vs. combination group (60±4.4) as shown in Fig. 3B (P<0.01). For the invasion
assay, the cell numbers were; doxorubicin group (9±0.8) vs.
combination group (3.5±0.7) as shown in Fig. 3C (P<0.01).
Various kinases are involved in the
doxorubicin/KU6- 0019-dependent signaling pathway
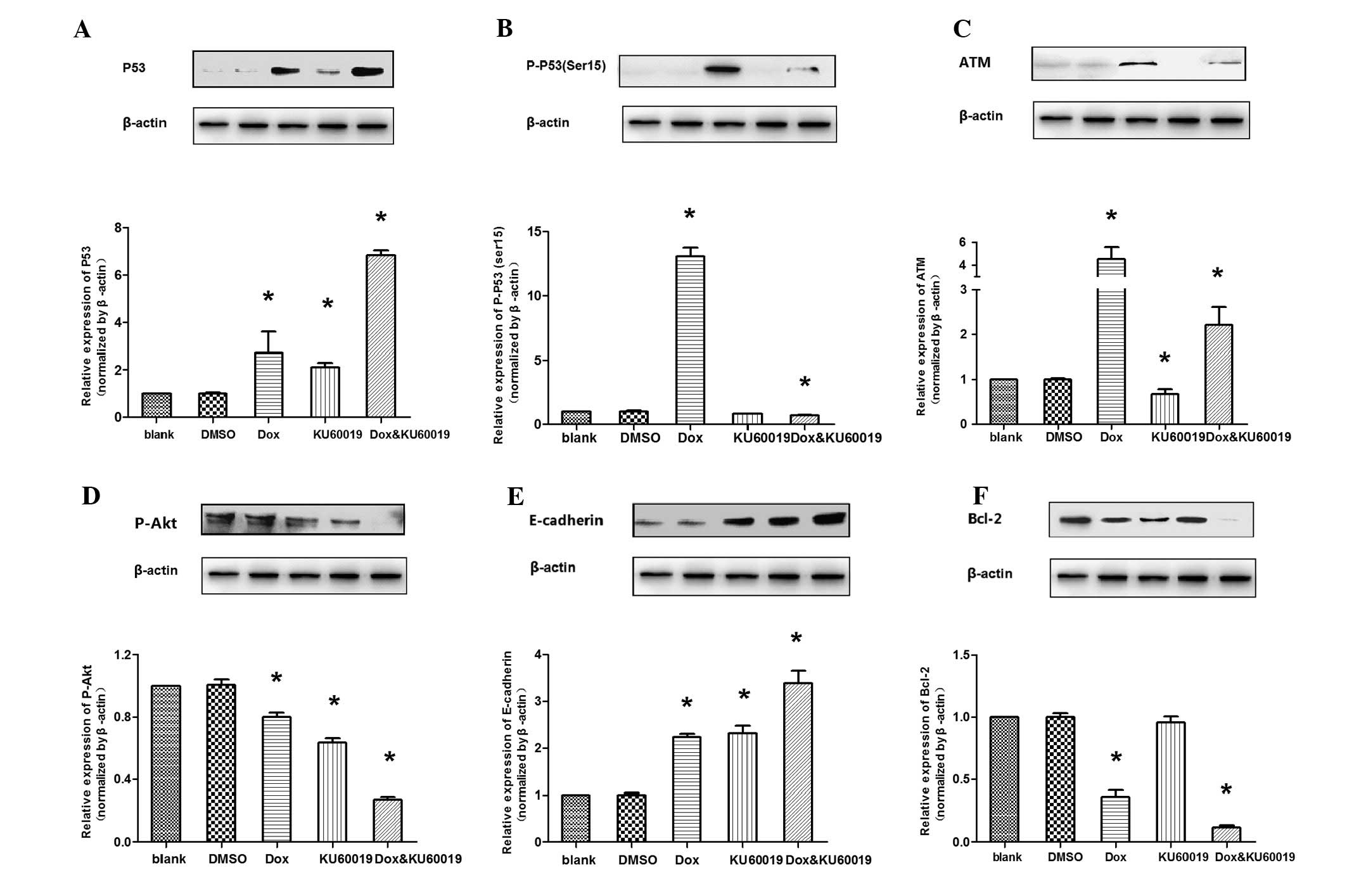
The expression levels of proteins regulated by
doxorubicin and/or KU60019 were examined. Compared with the control
groups, following treatment with doxorubicin and/or KU60019, the
accumulation of wild-type p53 and E-cadherin was observed, whereas
the p-Akt (Ser473) level decreased. The results are presented as
the ratio of Δp-p53 (Ser15)/Δp53. It was evident that this ratio
was always >1.0 (mean ± standard deviation, 1.9±0.3), which
indicated that treatment with doxorubicin, while leading to a rise
of total p53, induced a much greater rise in the proportion of
p-p53 at Ser15. It was evident that the key intracellular targets
of the ATM kinase and doxorubicin-induced p53 phosphorylation
(Ser15) were inhibited or almost completely abrogated in the
presence of low micromolar concentrations of KU60019. Additionally,
it was identified that the anti-apoptotic protein, Bcl-2, was only
marginally inhibited by KU60019 alone, whereas it was significantly
suppressed by the combination of the two compounds (Fig. 4).
Discussion
Surgery and chemoradiation significantly hinder the
progression of breast cancer, however, more effective treatments
for doxorubicin-based therapy remain a crucial requirement.
Doxorubicin-induced DNA damage response (DDR) involves numerous
highly conserved checkpoint pathways that are activated by
genotoxic stress. Checkpoint activation triggers a cascade of
events, which ultimately lead to cell cycle arrest or apoptosis.
One of key components of this response is ATM kinase, which
typically functions as a sensor of DNA damage (7).
The robust DNA repair capacity of cancer cells
results in a resistance to therapies, such as IR and cytotoxic
drugs, which are intended to cause lethal DNA damage (8). Specific improved ATM kinase inhibitors
have been developed in the context of the classic role of ATM in
DNA repair, with the rationale that inhibition of DNA repair is
likely to increase the efficacy of radiation or chemical therapy
(6). A previous study indicated
that KU60019, a highly effective radiosensitizer, inhibits DDR and
blocks radiation-induced phosphorylation of key ATM targets in
human glioma cells (9). The present
study demonstrated that the ATM kinase-specific inhibitor, KU60019,
effectively inhibits migration and invasion as well as
chemosensitization in the non-invasive MCF-7 human breast cancer
cell line.
An upregulation of the level of total p53 and p-p53
(Ser15) that was concurrent with an increased expression of ATM,
was observed in the cells that were treated with doxorubicin.
Previous studies showed that phosphorylation of p53 at Ser15, in
response to DNA double-strand breaks, was by the ATM protein kinase
(10). Furthermore, other
N-terminal sites may be phosphorylated by kinases that require the
prior phosphorylation of p53 at Ser15 (11). As hypothesized in the present study,
blocking of doxorubicin-induced ATM phosphorylation by KU60019
markedly reduced the level of p-p53 (Ser15). This indicated that
the loss of ATM and p-p53 (Ser15) may marginally inhibit
doxorubicin-induced DNA repair. However, similar to the alteration
observed in the apoptosis rate, exposure to KU60019 alone did not
suppress the expression of the anti-apoptotic protein, BCL-2, and
combining the two compounds induced an increased expression of
BCL-2. In certain cases, KU60019 and doxorubicin may synergize in
apoptosis. Thus, the combined use of the compounds (by inhibiting
the ATM-mediated DNA repair pathway and enhancing apoptosis) was
anticipated to produce a larger repair deficit and a corresponding
greater chemosensitization compared with each compound alone.
In glioma cells, KU60019 inhibits the
migration/motility and invasion of cells via deregulated receptor
tyrosine kinase-mediated signaling (9). Similarly, the expression of activated
Akt in fibrosarcoma or pancreatic cancer cells increases cell
invasion through Matrigel (12–14),
an effect that is recapitulated by an overexpression of Akt2 in
breast and ovarian cancer cells (15). In addition, the expression of Akt
promotes epithelial-mesenchymal transition, a process that is
closely associated with tumor progression to invasive and
metastatic carcinoma (16). Akt is
activated by a dual regulatory mechanism whereby maximal activation
requires additional phosphorylation at Ser473 (17,18).
Furthermore, E-cadherin is a calcium-dependent cell adhesion
molecule that mediates cell-cell adhesion and modulates cell
migration and tumor invasiveness (19). Compelling evidence exists, which
indicates that treating cells with KU60019 and/or doxorubicin
results in a decrease of p-Akt Ser473 and the increased expression
of E-cadherin, which is consistent with the diminished capacity of
migration and invasion exhibited by MCF-7 cells.
Another focus of the present study was to understand
the mechanism by which the combination of the two compounds
affected cell cycle arrest. Upon genotoxic damage, p53 contributes
to cell cycle arrest at the G1/S and/or G2/M
checkpoints via various mechanisms (9). Treatment with KU60019 alone was found
to markedly induce G1/S phase arrest and doxorubicin
resulted in G1/S and G2/M phase arrest via
activation of p53 (20,21). The cell cycle was halted at the
transition from the G1/S to the G2/M phase
that was induced by the combination of the two compounds, which may
also be involved in ATM and the downstream signaling of ATM
pathways. This indicated that the damage induced by the combination
of the two compounds provoked p53- and ATM-mediated cell cycle
arrest in MCF-7 cells (22).
In conclusion, the present study demonstrated that
KU60019 is a specific ATM kinase inhibitor, which is capable of
chemosensitizing MCF-7 cells when it is combined with doxorubicin.
Chemosensitization may result from the ability of KU60019 to
inhibit the phosphorylation of ATM and p53 (Ser15), alter cell
cycle checkpoints, decrease DNA repair (via inhibiting the
phosphorylation of p53; Ser15) and increase cell apoptosis.
Additionally, the results indicated that KU60019 (without
doxorubicin) inhibits MCF-7 cell motility and invasion, potentially
by acting on the p-Akt and E-cadherin signaling pathways. Thus,
KU60019 may be developed into a highly effective, cancer
therapeutic agent, acting as a chemosensitizer and curtailing tumor
dispersal. Furthermore, accelerated pharmaceutical development of
KU60019 is critical to expand the available treatment strategies
for non-invasive breast cancer.
Acknowledgements
The current study was supported by a grant from the
National Natural Science Foundation of China (grant no.
81272470).
References
|
1
|
Jeng KS, Sheen IS, Jeng WJ, et al: High
expression of Sonic Hedgehog signaling pathway genes indicates a
risk of recurrence of breast carcinoma. Onco Targets Ther. 7:79–86.
2013.
|
|
2
|
Binaschi M, Capranico G, Dal Bo L and
Zunino F: Relationship between lethal effects and topoisomerase
II-mediated double-stranded DNA breaks produced by anthracyclines
with different sequence specificity. Mol Pharmacol. 51:1053–1059.
1997.
|
|
3
|
Violet JA and Harmer C: Breast cancer:
improving outcome following adjuvant radiotherapy. Br J Radiol.
77:811–820. 2004.
|
|
4
|
Valerie K and Povirk LF: Regulation and
mechanisms of mammalian double-strand break repair. Oncogene.
22:5792–5812. 2003.
|
|
5
|
Lavin MF: Ataxia-telangiectasia: from a
rare disorder to a paradigm for cell signalling and cancer. Nat Rev
Mol Cell Biol. 9:759–769. 2008.
|
|
6
|
Hickson I, Zhao Y, Richardson CJ, et al:
Identification and characterization of a novel and specific
inhibitor of the ataxia-telangiectasia mutated kinase ATM. Cancer
Res. 64:9152–9159. 2004.
|
|
7
|
Ramachandran S, Tran DD, Klebba-Faerber S,
et al: An ataxia-telangiectasia-mutated (ATM) kinase mediated
response to DNA damage down-regulates the mRNA-binding potential of
THOC5. RNA. 17:1957–1966. 2011.
|
|
8
|
Helleday T, Petermann E, Lundin C, et al:
DNA repair pathways as targets for cancer therapy. Nat Rev Cancer.
8:193–204. 2008.
|
|
9
|
Golding SE, Rosenberg E, Valerie N, et al:
Improved ATM kinase inhibitor KU-60019 radiosensitizes glioma
cells, compromises insulin, AKT and ERK prosurvival signaling, and
inhibits migration and invasion. Mol Cancer Ther. 8:2894–2902.
2009.
|
|
10
|
Saito S, Goodarzi AA, Higashimoto Y, et
al: ATM mediates phosphorylation at multiple p53 sites, including
Ser(46), in response to ionizing radiation. J Biol Chem.
277:12491–12494. 2002.
|
|
11
|
Saito S, Yamaguchi H, Higashimoto Y, et
al: Phosphorylation site interdependence of human p53
post-translational modifications in response to stress. J Biol
Chem. 278:37536–37544. 2003.
|
|
12
|
Park BK, Zeng X and Glazer RI: Akt1
induces extracellular matrix invasion and matrix
metalloproteinase-2 activity in mouse mammary epithelial cells.
Cancer Res. 61:7647–7653. 2001.
|
|
13
|
Kim D, Kim S, Koh H, et al: Akt/PKB
promotes cancer cell invasion via increased motility and
metalloproteinase production. FASEB J. 15:1953–1962. 2001.
|
|
14
|
Tanno S, Tanno S, Mitsuuchi Y, et al: AKT
activation up-regulates insulin-like growth factor I receptor
expression and promotes invasiveness of human pancreatic cancer
cells. Cancer Res. 61:589–593. 2001.
|
|
15
|
Arboleda MJ, Lyons JF, Kabbinavar FF, et
al: Overexpression of AKT2/protein kinase Bbeta leads to
up-regulation of beta1 integrins, increased invasion, and
metastasis of human breast and ovarian cancer cells. Cancer Res.
63:196–206. 2003.
|
|
16
|
Grille SJ, Bellacosa A, Upson J, et al:
The protein kinase Akt induces epithelial mesenchymal transition
and promotes enhanced motility and invasiveness of squamous cell
carcinoma lines. Cancer Res. 63:2172–2178. 2003.
|
|
17
|
Andjelković M, Alessi DR, Meier R, et al:
Role of translocation in the activation and function of protein
kinase B. J Biol Chem. 272:31515–31524. 1997.
|
|
18
|
Bellacosa A, Chan TO, Ahmed NN, et al: Akt
activation by growth factors is a multiple-step process: the role
of the PH domain. Oncogene. 17:313–325. 1998.
|
|
19
|
Hazan RB, Phillips GR, Qiao RF, et al:
Exogenous expression of N-cadherin in breast cancer cells induces
cell migration, invasion, and metastasis. J Cell Biol. 148:779–790.
2000.
|
|
20
|
Ciciarello M, Mangiacasale R, Casenghi M,
et al: p53 displacement from centrosomes and p53-mediated G1 arrest
following transient inhibition of the mitotic spindle. J Biol Chem.
276:19205–19213. 2001.
|
|
21
|
Zhang T, Tan Y, Zhao R and Liu Z: DNA
damage induced by oridonin involves cell cycle arrest at G2/M phase
in human MCF-7 cells. Contemp Oncol (Pozn). 17:38–44. 2013.
|
|
22
|
Abraham RT: Cell cycle checkpoint
signaling through the ATM and ATR kinases. Genes Dev. 15:2177–2196.
2001.
|