Introduction
Glioblastoma multiforme is one of the most frequent
primary malignancies of the brain and accounts for ~40% of all
primary brain tumors (1,2). The median survival time for patients
with malignant glioma is poor, ranging between 15 and 22 months
(2). Surgical excision is the
primary clinical treatment option; however, due to its infiltration
into normal brain tissue and the specificity of growth locations
(3), the tumor usually cannot be
removed completely (4).
Chemotherapeutic drugs rarely reach brain tumor cells and,
similarly to radiotherapy, certain systemic side effects are
experienced (5). The majority of
chemotherapy has failed due to the difficulties associated with
blood-brain barrier (BBB) penetration and poor glioma targeting of
the chemotherapeutics (6). All of
this has contributed to the poor efficacy of treatment regimens for
glioblastoma; therefore, new approaches to treatment are urgently
required (7).
Liposomes (LPs) represent a versatile system for
drug delivery in cancer therapy, which may alter the
pharmacokinetic properties of compounds. To date, several
drug-loaded LPs have been approved by the Food and Drug
Administration for cancer therapy (8). To further enhance the antitumor
efficiency and reduce side effects, receptor-targeted LPs have been
developed. Chaudhury et al (9) demonstrated that folate
receptor-targeted liposomal carboplatin may improve the therapeutic
efficacy in the treatment of metastatic ovarian cancer. Rodriguez
et al (10) reported that
the epidermal growth factor receptor-targeted LP was more effective
in the control of tumor growth. It is known that the clinical
application of chemotherapy to brain tumors has been severely
limited by the inability of compounds to penetrate the BBB
(11). To overcome the challenge of
drug delivery across the BBB to effectively target glioma, the
current study investigates the use of receptor-targeted LP.
The cell adhesion molecule, integrin
αvβ3, is particularly known for its role in
cancer progression and is overexpressed in melanomas, glioblastoma,
and ovarian, breast and prostate cancers (12). Arginine-glycine-aspartic acid
(RGD)-containing peptides have been identified to have high
affinity for αvβ3 integrin (13) and, in particular, for the
αvβ3 integrin that is overexpressed in
glioma. Transferrin (TF) is a specific ligand for the TF receptor
(TFR), which is overexpressed in the BBB and tumor cells (14). TF targeting LPs have been reported
to increase the BBB penetration of the encapsulated drug and
thereby improve the therapeutic efficacy towards brain glioma in
vivo (15–17).
In this study, to further intensify the targeting
efficiency of LP, it was modified with RGD and TF to exert its
superior glioma targeting property in vivo. It is proposed
that the targeting of glioma can be achieved in the following two
steps: The TFR that is overexpressed in the BBB may aid the LP to
cross the BBB efficiently, while the RGD and TF enhance the
targeting migration and accumulation of LPs to the
αvβ3 integrin-expressing tumor. Subsequently,
TF improves the cellular uptake of LP by TFR-expressing tumor
cells. To characterize the potential for the dual-targeting effects
of LP modified with RGD and TF, the fluorescent dyes,
30-tetramethylindotricarbocyanine iodide (DiR) and coumarin-6 were
utilized to track the behavior of RGD/TF-LP in vivo and
in vitro, respectively. To identify the targeting
efficiency, in vitro cellular uptake analysis was performed.
The tumor spheroid penetration characteristics were evaluated for
RGD/TF-LP, which was important for solid tumor therapy. In
vivo imaging was utilized to evaluate the glioma imaging value
of RGD/TF-LP. The MTT assay and the growth inhibition of tumor
spheroids were studied to further demonstrate the chemotherapeutic
value of paclitaxel (PTX)-loaded RGD/TF-LP.
Materials and methods
Materials and animals
The C6 and b.End.3 cell lines were purchased from
American Type Culture Collection (Manassas, VA, USA). Soybean
phospholipids (SPC) and cholesterol (Cho) were purchased from
Sym-Bio Life Science Co., Ltd., (Shanghai, China). NHS-PEG2000-MAL
and mPEG2000-NHS were purchased from JenKem Technology Co. Ltd.
(Beijing, China). TF and coumarin-6 were purchased from
Sigma-Aldrich (St. Louis, MO, USA). RGD peptide was purchased from
Qiangyao Biotechnology Ltd., (Shanghai, China) and DiR was
purchased from Biotium, Inc., (Hayward, CA, USA). Other chemicals
and reagents were of analytical grade and obtained commercially
(Jinxing Biotechnology Ltd., Zhengzhou, China).
Male BALB/c mice (~20 g in weight) were purchased
from the Experimental Animal Center of Zhengzhou University
(Zhengzhou, China). All of the animal experiments adhered to the
principles of care and use of laboratory animals and were approved
by the Ethics Committee of Experimental Animals in Henan Cancer
Hospital, The Affiliated Cancer Hospital of Zhengzhou
University.
Synthesis of DSPE-PEG2000-RGD
The RGD mimetic was synthesized according to the
literature protocol with certain modifications (18). RGD was conjugated with
DSPE-PEG2000-BTC (Ruixi Biotechnology Ltd., Xi’an, China) in 0.01 M
isotonic HEPES buffer (pH 7.5) under the following reaction
conditions: Gentle stirring for 4 h at 4°C, with a 1:2 molar ratio
of the peptides to DSPE-PEG2000-BTC. The reaction was traced by
thin-layer chromotography until the peptide was completely
consumed. The mixture was subsequently dialyzed against water, and
lyophilized. The resulting conjugate DSPE-PEG2000-RGD was used for
preparing the LPs without further purification.
Preparation of LPs
RGD-conjugated LPs (RGD-LP) were prepared by thin
film hydration methods (19). The
SPC, Cho, DSPE-PEG2000 and DSPE-PEG2000-RGD were dissolved in
chloroform (the total molar ratio of phospholipid to Cho
derivatives was 3:2, while the molar ratio of DSPE-PEG2000 to
DSPE-PEG2000-RGD was 9.5:5). Chloroform was then removed by rotary
evaporation and any residual organic solvent was removed under
vacuum overnight. Subsequently, the thin film was hydrated in
phosphate-buffered saline (PBS; pH 7.4) for 1 h at 37°C, followed
by intermittent probe sonication (5 sec pulse/5 sec rest for 5
cycle durations) for 50 sec at 100 W.
Bare LPs were prepared by thin film hydration
methods initially, and TF-LPs were prepared by the post-insertion
method (20,21). This method was adopted to
incorporate the TF into the bare LP. TF was reacted with Traut’s
reagent (Pierce Biotechnology, Inc., Rockford, IL, USA) at a molar
ratio of 1:5 to yield the TF-thiol (SH). The TF-SH was reacted with
the DSPE-PEG2000-Mal micelles at a molar ratio of 1:10, and
subsequently incubated with the bare LP for 1 h at 37°C. The ratio
of TF-PEG2000-DSPE to lipid was 1:50. The final LPs were stored at
4°C for further experiments.
The RGD/TF-LP was prepared by the post-insertion
method with RGD-LP instead of bare LPs. For the LPs used in the
in vitro experiment, coumarin-6 was incorporated within the
total lipids as a fluorescent probe. The LPs used for the in
vivo experiment were the same as those used for in vitro
experiments, with the exception of the replacement of the
fluorescent probe, coumarin-6, with DiR.
Characterization of LPs
The size distribution and ζ-potential of LPs were
analyzed using a Malvern Zetasizer Nano ZS90 instrument (Malvern
Instruments Ltd., Malvern, UK). Encapsulation efficiencies of PTX
in the LPs were determined using high performance liquid
chromatography (HPLC 1200 Series; Agilent Technologies Inc., Santa
Clara, CA, USA).
Cell uptake
The C6 and bEnd.3 cell lines were seeded into
24-well plates at a density of 2×105 cells/ml. After 24
h, each well was subsequently incubated with 1 ml of a 100 mg/ml
coumarin-6-loaded LP, RGD-LP, TF-LP and RGD/TF-LP for 2 h. For
quantitative analysis, at the designated time period, the
suspension was removed and the wells were washed three times with
1,000 μl cold PBS. Following this, 50 μl of 0.5% Triton X-100 (Dow
Chemical Co., Midland, MI, USA) was introduced into each well for
cell lysis. The fluorescence intensity of each sample well was
measured using the GENios microplate reader (Tecan, Männedorf,
Switzerland), with an excitation wavelength of 465 nm and emission
wavelength of 502 nm. For the qualitative study, the cells were
washed three times with cold PBS and fixed with 4% paraformaldehyde
for 20 min. Then, the cells were washed twice with cold PBS and
observed by confocal laser scanning microscopy (Leica TCS SP5;
Leica, Mannheim, Germany).
In vitro cell cytotoxicity
For cytotoxicity measurements, C6 cells were
incubated in 96-well transparent plates (Costar, Chicago, IL, USA)
at a density of 5×103 cells/well (0.1 ml). After 12 h,
the old medium was removed and the cells were incubated in fresh
media containing PTX or PTX-loaded LPs at concentrations of 0.3, 3,
10 and 300 μg/ml, for 24 and 48 h. The LPs were sterilized with UV
irradiation for one day prior to use. MTT assay was used to measure
the cell viability. The absorbance of the wells was measured by a
microplate reader (Tecan) with the wavelength of 570 nm and the
reference wavelength of 620 nm. Cell viability was defined as the
percentage of the absorbance of the wells containing the cells
incubated with the LP suspension divided by the absorbance of the
wells containing only cells.
Evaluation of tumor spheroid
penetration
To prepare the three-dimensional (3D) tumor
spheroids, the C6 cells (200 μl) were seeded at a density of
2×103 cells per well in 96-well plates coated by 80 μl
of a 2% low melting temperature agarose. Seven days following this,
the cells were seeded and the tumor spheroids were treated with 10
μg/ml coumarin-6-loaded LPs. Following 4 h of incubation, the
spheroids were rinsed three times with ice-cold PBS and fixed using
4% paraformaldehyde for 30 min. Subsequently, the spheroids were
transferred to glass slides and covered by glycerophosphate.
Fluorescent intensity was observed using laser scanning confocal
microscopy (Leica).
Growth inhibition of tumor spheroid
Tumor spheroids were prepared as described in the
previous section. After seven days the wells containing the
spheroids were treated with 3 mg/ml of the PTX solution and
PTX-loaded LPs. The length and width of each spheroid were measured
each day for eight days and the volume was calculated. A volume
curve was calculated to allow the comparison of the effects of each
treatment with the various formulations.
In vivo imaging in tumor-bearing
mice
The DiR loaded LPs were utilized as previously
described, to investigate the distribution of LPs in male BALB/c
mice bearing a C6 orthotopic glioma (22,23).
BALB/c mice were anesthetized with 5% chloral hydrate and
individually placed in brain stereotactic apparatus (World
Precision Instruments Inc., Sarasota, FL, USA). The C6 cells
(5×105 cells/7.5 μl of PBS, pH 7.4) were injected into
the right brain of each mouse (1.8 mm lateral to bregma and 3.0 mm
deep from the dura) at a rate of 3.0 μl/min. Eight days following
the injection, the DiR-loaded LP, RGD-LP, TF-LP and RGD/TF-LP was
intravenously administered into the mice and subsequently, the
in vivo fluorescence imaging was performed at predetermined
time points using the IVIS® Spectrum system (Caliper
Life Sciences, Hopkinton, MA, USA).
Results
Characterization of LPs
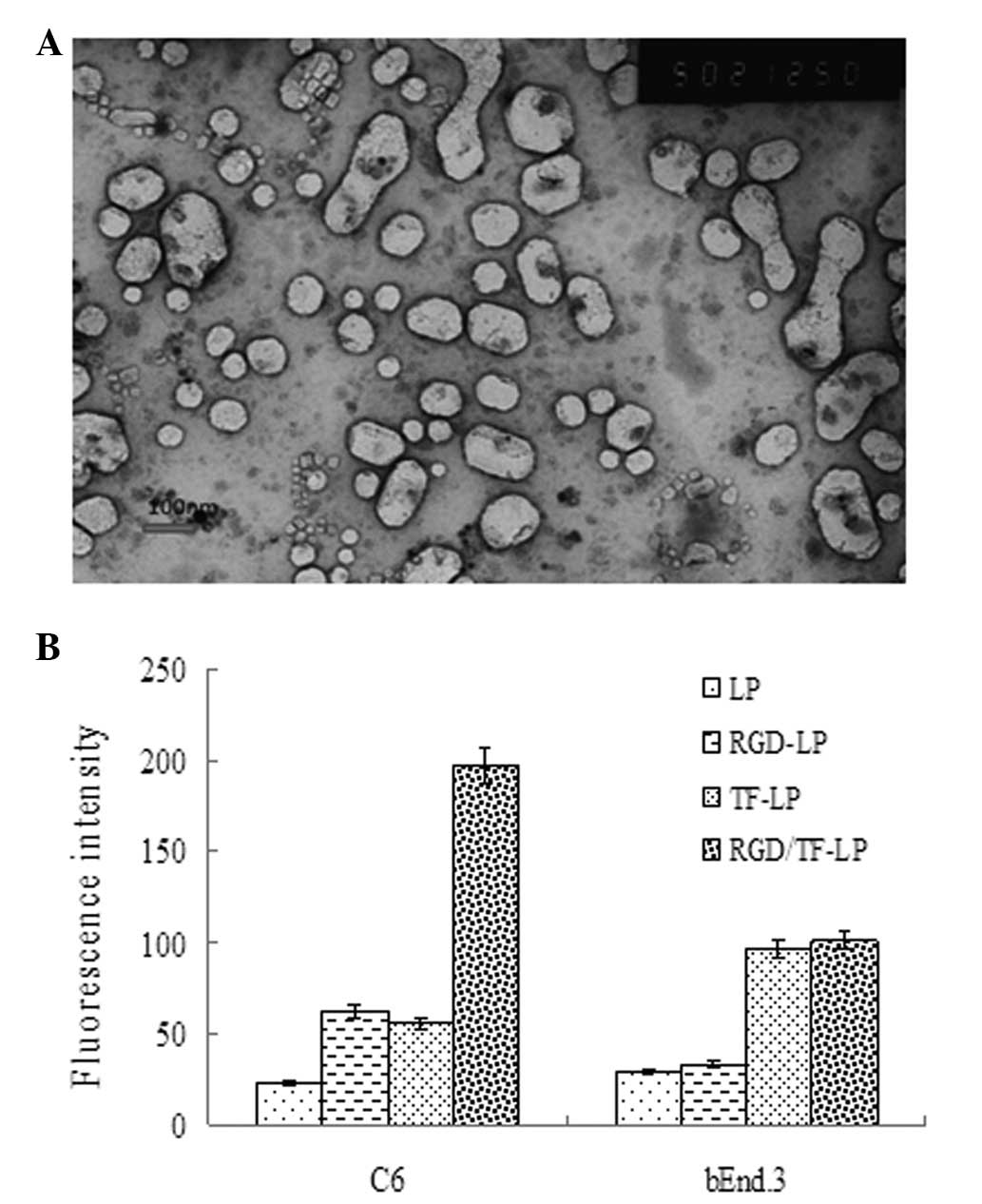
A summary of the PTX-loaded LPs is provided in
Table I. The LP sizes were ~120 nm,
with a polydispersity index of ~0.2. The conjugation with TF
marginally increased the LP sizes. However, the encapsulation of
PTX, courmarin-6 and DiR did not affect the LP size. Transmission
electronic microscopy confirmed that the LPs were generally
spheroid (Fig. 1A). The
polydispersity of all the LPs also exhibited a narrow size
distribution. With regard to drug encapsulation efficiency (EE),
the four LPs all demonstrated high loadings of >75%. The
slightly lower EEs for the TF-LP and RGD/TF-LP were likely to be
due to drug loss during the incubation and post-preparation washing
steps.
 | Table ICharacteristics of paclitaxel-loaded
liposomes, including particle size, size distribution, ζ-potential
and drug encapsulation efficiency (n=3). |
Table I
Characteristics of paclitaxel-loaded
liposomes, including particle size, size distribution, ζ-potential
and drug encapsulation efficiency (n=3).
| Group | Particle size,
nm | Polydispersity | ζ-potential, mV | Encapsulation
efficiency, % |
|---|
| LP | 112±7.8 | 0.107 | −2.55±1.47 | 85.45±1.43 |
| RGD-LP | 116±5.5 | 0.120 | 1.26±1.42 | 84.24±1.85 |
| TF-LP | 124±9.5 | 0.182 | −2.67±1.25 | 77.85±0.80 |
| RGD/TF-LP | 128±13.0 | 0.210 | −2.67±1.85 | 76.65±1.57 |
Cellular uptake characterization in
vitro
The C6 and bEnd.3 cell lines had the ability to take
up the coumarin-6-loaded LP, RGD-LP, TF-LP and RGD/TF-LP at various
capacities (Fig. 1B). In bEnd.3
cells, the level of RGD/TF-LP uptake was ~3.2 times higher than for
RGD-LP, while that of RGD-LP was almost the same as that of LP.
However, in C6 cells, RGD-LP, TF-LP and RGD/TF-LP uptake was
markedly higher than that of LP (approximately 2.7, 2.4 and
8.6-fold higher, respectively). The cell uptake efficiency of
RGD/TF-LP was also markedly higher compared with that of RGD-LP and
TF-LP, which was proposed to be the result of the targeting
capacity of αvβ3 integrin and TFRs. The
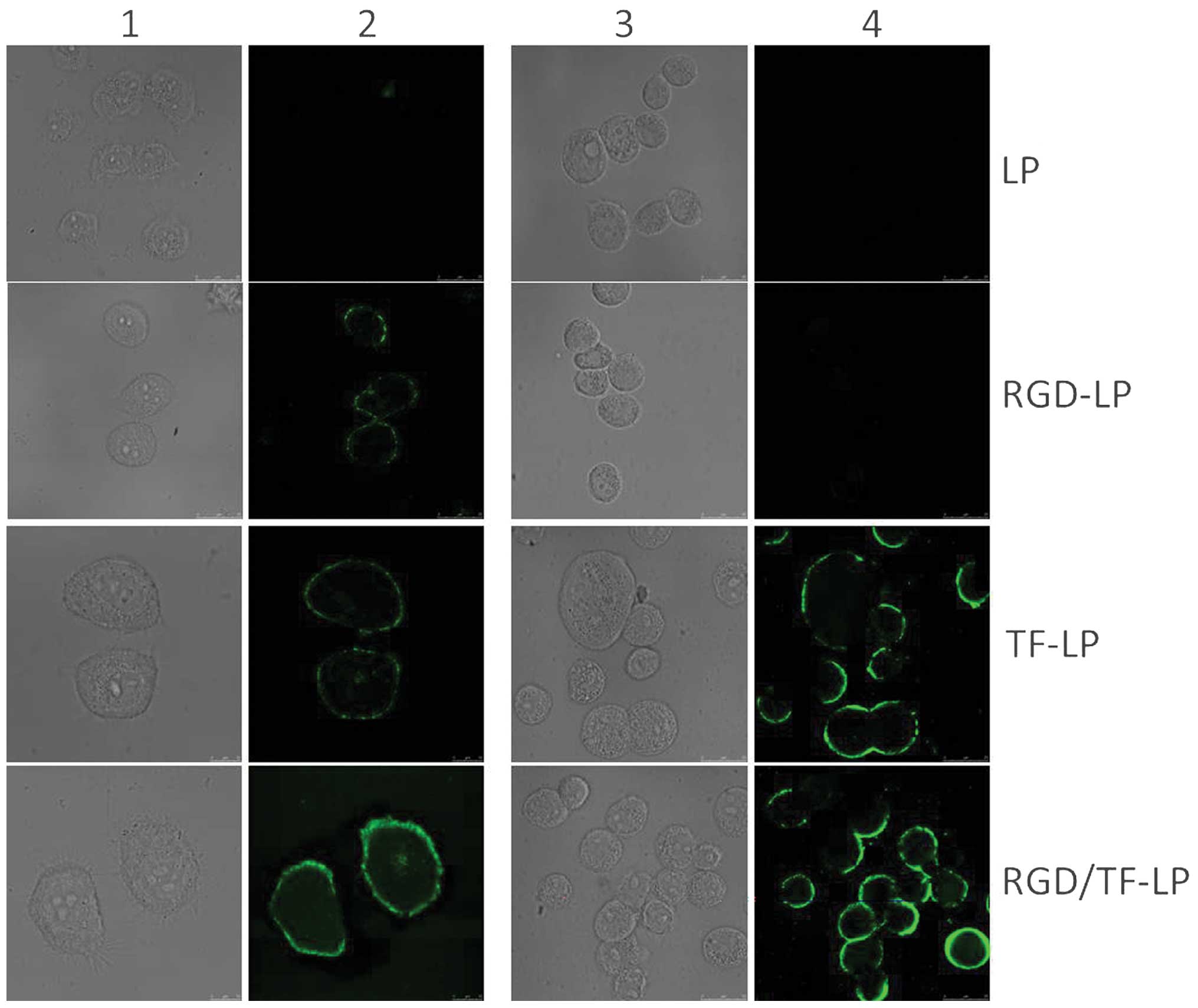
confocal images of bEnd.3 and C6 cells following incubation with
the various LPs are shown in Fig.
2. The fluorescence intensity of the LP alone was the lowest
observed between the two cell types. In bEnd.3 cells (Fig. 2; columns 3 and 4), the fluorescence
intensity of TF-LP and RGD/TF-LP was higher than that of LP and
RGD-LP, while in C6 cells, the fluorescence intensity of RGD-L-P,
TF-LP and RGD/TF-LP was markedly higher compared with that of LP.
The quantitative analysis indicated extremely similar results to
those obtained from the fluorescence imaging.
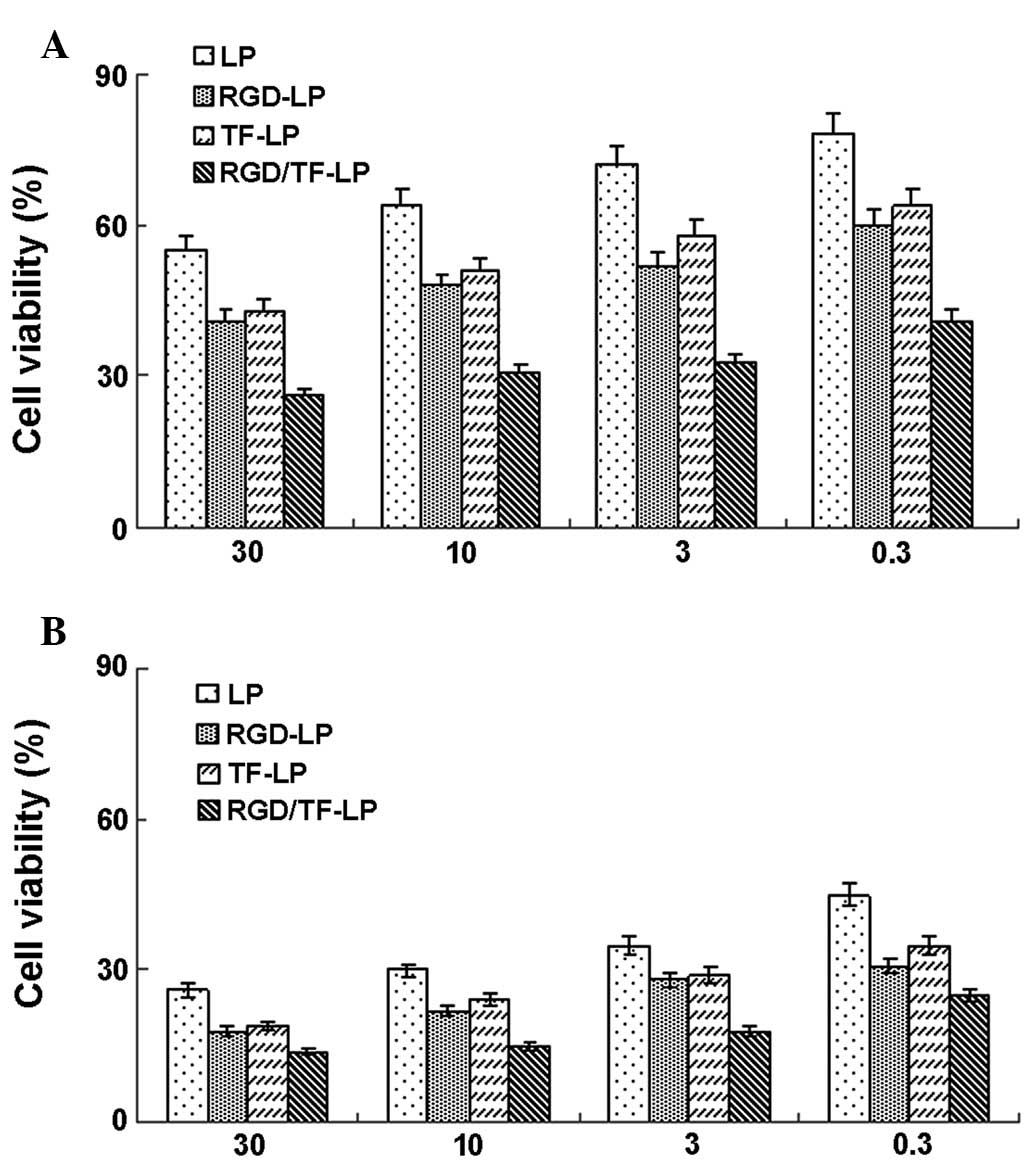
Cytotoxicity of LPs
The in vitro viability of C6 cells is shown
in Fig. 3 following 24 and 48 h of
culture with PTX-LP, PTX-RGD-LP, PTX-TF-LP and PTX-RGD/TF-LP at
various concentrations. The viability of C6 cells decreased with
the increasing incubation time as well as the PTX concentration.
LPs exhibited higher toxicity following conjugation with RGD or TF,
as the TF receptor and αvβ3 integrin are
overexpressed in glioma cells (24).
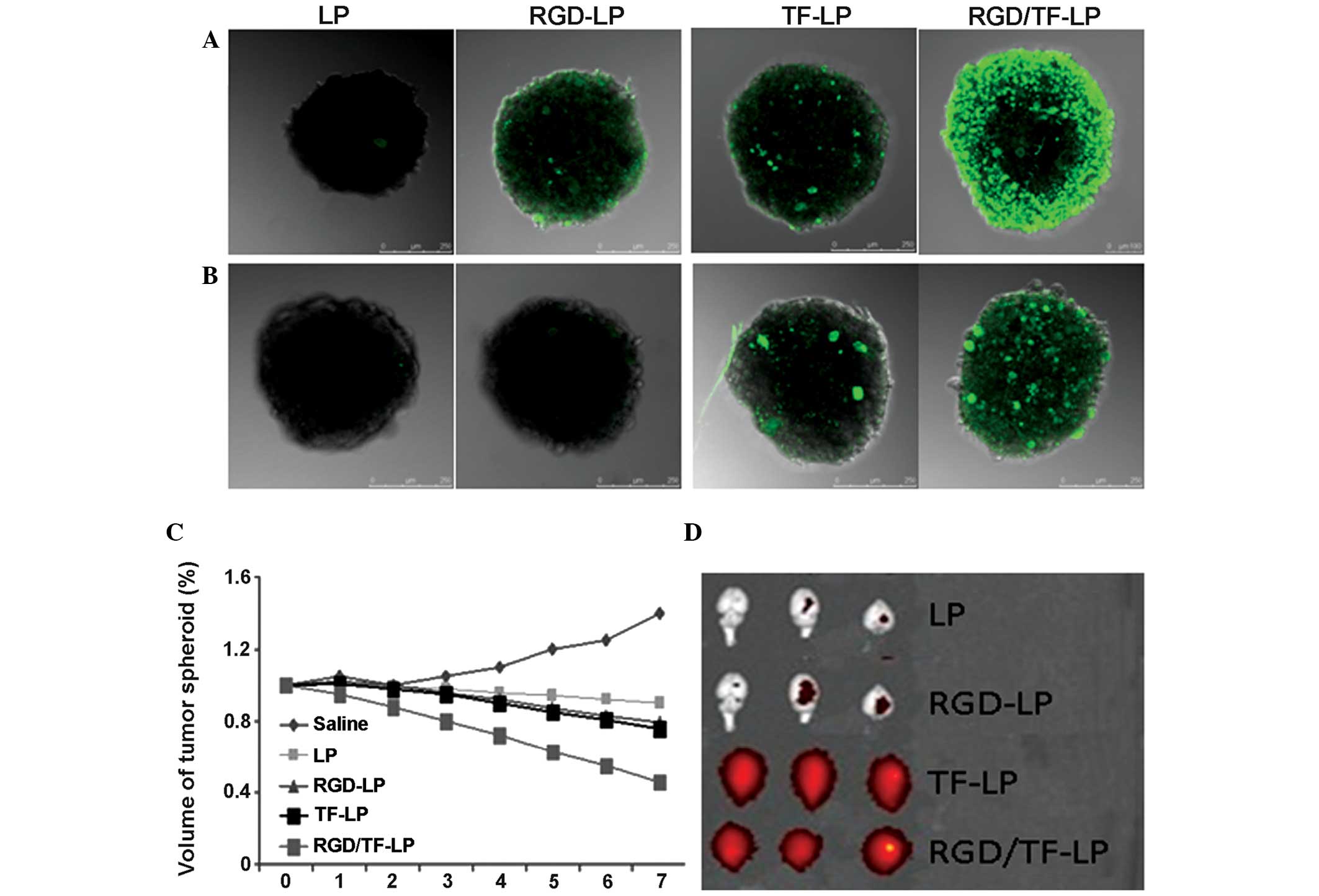
Evaluation of tumor spheroid
penetration
To evaluate the tumor spheroid penetration of the
dual targeting LP, RGD/TF-LP, the tumor spheroid transportation and
a bEnd.3 monolayer penetration model were used. The distribution of
RGD-LP, TF-LP and RGD/TF-LP was markedly higher in the whole
spheroid (Fig. 4A), indicating that
RGD and TF may effectively increase the tumor uptake and
penetration. This enhanced adsorption and transportation was
essential for inhibiting tumor growth. As shown in Fig. 4B, the uptake of RGD/TF-LP was the
highest of the four formulations, while that of LP was the lowest
for C6 spheroids cocultured with the bEnd.3 monolayers.
Growth inhibition of tumor spheroid
The influence of various treatments on the growth of
tumor spheroids was also investigated. Fig. 4C shows the in vitro tumor
spheroid volume ratios following treatment with saline, LP, RGD-LP,
TF-LP and RGD/1TF-LP at the final PTX concentration of 3 mg/ml,
respectively. Continued growth in size and volume was observed for
the tumor spheroids, in the absence of any drug (140% of the
primary volume after seven days). An evident reduction in volume of
the tumor spheroids was observed for all PTX formulations after
seven days of treatment, indicating that the tumor spheroids were
sensitive to PTX. The percentage change in the tumor spheroid
volumes (%) on day seven were ~90, ~79, ~76 and ~46% for PTX loaded
LP, TF-LP, RGD-LP and RGD/TF-LP, respectively. These results
indicated that RGD/TF-LP markedly improved the inhibitory effects
on the 3D tumor spheroids. For solid tumors, regions with high
pressure and few vessels may also be identified. The tumor
spheroids may imitate the in vivo status, as the tumor
spheroids are free of blood vessels; therefore, the tumor spheroid
penetration and inhibitory effects were likely to be caused by the
influence of the TFR and αvβ3 integrin.
In vivo imaging
The different combinations presented diverse
targeting effects. Brain ex vivo imaging demonstrated that
unmodified LP is rarely distributed in the brain, while RGD-LP is
marginally distributed in the brain (Fig. 4D). However, when conjugated with TF,
the accumulation of LPs in the brain is markedly increased. TF-LP
is distributed throughout the whole brain without selectivity,
while RGD/TF-LP is distributed in the glioma of the brain more than
TF-LP, revealing an effective and precise target for this type of
brain cancer. The brain fluorescence intensity of the RGD-LP was
extremely similar to that of the LP, indicating that RGD may not
significantly enhance the brain uptake of the LPs. The increased
uptake by the glioma may be due to the enhanced penetration of the
RGD and TF when the LPs diffused to the glioma by an enhanced
permeability and retention effect.
Discussion
The BBB is an important factor that lowers the
antitumor efficiency of chemotherapeutic drugs in the treatment of
glioma (25). Therefore, there is a
requirement to develop a drug delivery system that is able to
penetrate the BBB and, thus, improve the therapeutic efficiency of
glioma in the clinic. Receptor-modified LPs represent an effective
approach to increase the penetration of chemotherapeutic drugs
(26). In the present study, a
dual-targeting LP conjugated with transferrin and RGD was generated
for glioma-targeting therapy. In this liposomal formulation, the
receptor-targeting properties of transferrin and RGD were combined
with the enhanced cell uptake effect to improve the transport of
desired cargo to the tumor.
Particle size plays a critical role in their
clearance by the sinusoidal spleens of human and rats. Particles
must be small enough to avoid the splenic filtration process at the
interendothelial cell slits in the walls of venous sinuses
(27). Similarly, particle size is
an important factor that affects the LP endocytosis by the brain
capillary cells on the BBB, and the size distribution is generally
limited to ~200 nm in diameter for brain-targeted LPs (28). In the current study, the sizes of
the prepared LPs were all below 130 nm, which provided a favorable
size condition for brain transport. The particle sizes decreased
due to the stabilizing effect of polyethene glycols (PEGs), which
prevented the LP interactions. The polydispersity index (PDI)
increased with the introduction of PEGs, which can be explained by
the greater flexibility and folding of longer chains. A PDI of
<0.300 and particle diameters of ~200 nm were considered
adequate for further in vitro and in vivo
studies.
The bEnd.3 cells are an immortalized mouse brain
endothelial cell line exhibiting endothelial properties. These
cells are widely used as a model for the BBB due to their rapid
growth, the maintenance of the BBB characteristics over repeated
passages, the formation of functional barriers and the amenability
to numerous molecular interventions (29). Thus, this cell line was chosen as a
simple BBB model to study the brain delivery property of the LPs
in vitro. The cellular uptake of LP, RGD-LP, TF-LP and
RGD/TF-LP was characterized using bEnd.3 and C6 glioma cells. The
results (Fig. 1B) showed that the
uptake of RGD-LP by bEnd.3 cells was marginally greater than that
of the LP, which suggested RGD did not have a high binding affinity
for the bEnd.3 cells. Following conjugation with TF, the uptake of
LPs, including TF-LP and RGD/TF-LP, markedly increased,
demonstrating that TF effectively mediated LP uptake by endothelial
cells. In C6 cells, both the TF receptor and αvβ3 integrin are
overexpressed, and TF and RGD could recognize the C6 cells and
mediate endocytosis (24), which
contributed to a great increase in the uptake of RGD-LP, TF-LP and
RGD/TF-LP by C6 cells (Fig. 1B and
Fig. 2). The cellular uptake
demonstrated that TF bound well to the bEnd.3 cells and C6 cells,
for both the first stage to deliver the drug across the BBB and the
second stage to target glioma. RGD was found to be beneficial for
the second stage to target glioma. RGD and TF could effectively
increase the efficiency of LPs targeting to glioma.
In the cytotoxicity experiment, the PTX-loaded LP,
RGD-LP, TF-LP and RGD/TF-LP demonstrated time- and dose-dependent
cytotoxic activity towards C6 cells. Notably, the PTX-RGD/TF-LP
formulation achieved the lowest cell viability among the four LP
formulations in all equivalent drug concentration levels applied.
This further confirmed the advantages for cellular uptake shown in
the previous experiments, which resulted from the coactivation of
the TF receptor and αvβ3 integrin, thus contributing to an
additional pathway through which the drug could be delivered into
the cell cytoplasm to induce cell apoptosis.
In numerous solid tumors, there are regions with
high pressure and few vessels (30). Due to the poor permeation of
delivery systems, the level of drug that is able to access the
inner area of solid tumors is low. As a consequence, these
chemotherapy ‘blind areas’ eventually and ineluctably induce the
recurrence of cancer, and the overall chemotherapeutic efficacy of
anticancer agents is compromised (31). For a cancer treatment to be
curative, the delivery system must efficiently penetrate the tumor
tissue to reach all of the viable cells. Thereby, three-dimesnional
multicellular modeling, which represents the avascular regions
found in numerous solid tumor tissues, can serve as an invaluable
tool to evaluate the solid tumor penetration effect of a drug
delivery system (32). In the
present study, the results (Fig. 4A and
B) demonstrated the penetration capabilities of LP, RGD-LP,
TF-LP and RGD/TF-LP. It was found that the existence of the bEnd.3
monolayers markedly decreased the uptake of RGD-LP, which was
similar to that of LP. The TF could enhance the transport of LPs
across the bEnd.3 monolayer, and it could increase the uptake and
penetration of RGD-LP by the C6 spheroids. These findings indicated
that the combination of RGD and TF was able to effectively
transport the LPs across the two barriers to then be successfully
taken up by the spheroids.
In the growth inhibition experiments in the present
study, utilizing PTX-loaded LP, RGD-LP, TF-LP and RGD/TF-LP, the
tumor spheroid was used to imitate the in vivo status of the
solid tumor and to evaluate the antitumor efficiency of the
different LPs. The results showed that PTX-loaded RGD/TF-LP
possessed the greatest antitumor activity, which may benefit from
its increased penetration and uptake by tumors. The modified TF and
RGD also could facilitate the transportation of LPs through C6
tumor spheroids, which was markedly better than LP alone. This
finding demonstrated that RGD/TF-LP could overcome the barriers of
the endothelial and tumor cells to arrive at the center of the
tumor. In vivo imaging further demonstrated that RGD/TF-LP
could combine the brain target and the glioma target effects.
In conclusion, the present study has demonstrated a
targeted delivery system for glioma therapy, RGD/TF-LP. This system
has an enhanced and precise targeting effect when compared with the
TF-LP or RGD-LP delivery systems. LPs modified with TF aided in the
penetration and improved the glioma targeting, while RGD enhanced
the cellular uptake and accumulation in the tumor. This system
could target both endothelial and tumor cells, and penetrate the
endothelial cell monolayer and tumor spheroid to reach the center
of the tumor cell mass. The targeting and penetration effects
resulted in the highest glioma accumulation compared with single
target RGD-LP or TF-LP, leading to the best imaging results. Thus,
the dual-targeting LP conjugated with TF and RGD may have the
potential to serve as a drug delivery system in glioma therapy.
Further studies regarding this delivery system are required to
identify appropriate anti-glioma drugs, improve the encapsulation
efficiency and to investigate its potential application in glioma
targeting therapy.
Abbreviations:
|
LP
|
liposome
|
|
BBB
|
blood-brain barrier
|
|
TF
|
transferrin
|
|
TFR
|
transferrin receptor
|
|
PTX
|
paclitaxel
|
|
DiR
|
30-tetramethylindotricarbocyanine
iodide
|
References
|
1
|
Jain RK, di Tomaso E, Duda DG, Loeffler
JS, Sorensen AG and Batchelor TT: Angiogenesis in brain tumours.
Nat Rev Neurosci. 8:610–622. 2007.
|
|
2
|
Hegi ME, Diserens AC, Gorlia T, et al:
MGMT gene silencing and benefit from temozolomide in glioblastoma.
N Engl J Med. 352:997–1003. 2005.
|
|
3
|
Ong BY, Ranganath SH, Lee LY, et al:
Paclitaxel delivery from PLGA foams for controlled release in
post-surgical chemotherapy against glioblastoma multiforme.
Biomaterials. 30:3189–3196. 2009.
|
|
4
|
Genc DB, Canpolat C and Berrak SG:
Clinical features and management of carboplatin-related
hypersensitivity reactions in pediatric low-grade glioma. Support
Care Cancer. 20:385–393. 2012.
|
|
5
|
Pang Z, Feng L, Hua R, et al:
Lactoferrin-conjugated biodegradable polymersome holding
doxorubicin and tetrandrine for chemotherapy of glioma rats. Mol
Pharm. 7:1995–2005. 2010.
|
|
6
|
Pardridge WM: Brain drug development and
brain drug targeting. Pharm Res. 24:1729–1732. 2007.
|
|
7
|
Guerin C, Olivi A, Weingart JD, Lawson HC
and Brem H: Recent advances in brain tumor therapy: local
intracerebral drug delivery by polymers. Invest New Drugs.
22:27–37. 2004.
|
|
8
|
Muthu MS and Feng SS: Theranostic
liposomes for cancer diagnosis and treatment: current development
and pre-clinical success. Expert Opin Drug Deliv. 10:151–155.
2013.
|
|
9
|
Chaudhury A, Das S, Bunte RM and Chiu GN:
Potent therapeutic activity of folate receptor-targeted liposomal
carboplatin in the localized treatment of intraperitoneally grown
human ovarian tumor xenograft. Int J Nanomedicine. 7:739–751.
2012.
|
|
10
|
Rodriguez BL, Li X, Kiguchi K, DiGiovanni
J, Unger EC and Cui Z: Control of solid tumor growth in mice using
EGF receptor-targeted RNA replicase-based plasmid DNA. Nanomedicine
(Lond). 7:475–491. 2012.
|
|
11
|
Tzeng SY and Green JJ: Therapeutic
nanomedicine for brain cancer. Ther Deliv. 4:687–704. 2013.
|
|
12
|
Marelli UK, Rechenmacher F, Sobahi TR,
Mas-Moruno C and Kessler H: Tumor targeting via integrin ligands.
Front Oncol. 3:2222013.
|
|
13
|
Li Q and Xu W: Novel anticancer targets
and drug discovery in post genomic age. Curr Med Chem Anticancer
Agents. 5:53–63. 2005.
|
|
14
|
Bidros DS and Vogelbaum MA: Novel drug
delivery strategies in neuro-oncology. Neurotherapeutics.
6:539–546. 2009.
|
|
15
|
Gao JQ, Lv Q, Li LM, et al: Glioma
targeting and blood-brain barrier penetration by dual-targeting
doxorubincin liposomes. Biomaterials. 34:5628–5639. 2013.
|
|
16
|
Miyata S, Kawabata S, Hiramatsu R, et al:
Computed tomography imaging of transferrin targeting liposomes
encapsulating both boron and iodine contrast agents by
convection-enhanced delivery to F98 rat glioma for boron neutron
capture therapy. Neurosurgery. 68:1380–1387. 2011.
|
|
17
|
Ying X, Wen H, Lu WL, et al:
Dual-targeting daunorubicin liposomes improve the therapeutic
efficacy of brain glioma in animals. J Control Release.
141:183–192. 2010.
|
|
18
|
Kurohane K, Namba Y and Oku N: Liposomes
modified with a synthetic Arg-Gly-Asp mimetic inhibit lung
metastasis of B16BL6 melanoma cells. Life Sci. 68:273–281.
2000.
|
|
19
|
Maeda T and Fujimoto K: A
reduction-triggered delivery by a liposomal carrier possessing
membrane-permeable ligands and a detachable coating. Colloids Surf
B Biointerfaces. 49:15–21. 2006.
|
|
20
|
Yang XJ, Koh CG, Liu SJ, et al:
Transferrin receptor-targeted lipid nanoparticles for delivery of
an antisense oligodeoxyribonucleotide against Bcl-2. Mol Pharm.
6:221–230. 2009.
|
|
21
|
Chiu SJ, Liu S, Perrotti D, Marcucci G and
Lee RJ: Efficient delivery of a Bcl-2-specific antisense
oligodeoxyribonucleotide (G3139) via transferrin receptor-targeted
liposomes. J Control Release. 112:199–207. 2006.
|
|
22
|
Adam JF, Joubert A, Biston MC, et al:
Prolonged survival of Fischer rats bearing F98 glioma after
iodine-enhanced synchrotron stereotactic radiotherapy. Int J Radiat
Oncol Biol Phys. 64:603–611. 2006.
|
|
23
|
Gu YT, Zhang H and Xue YX: Dexamethasone
enhances adenosine 5′-triphosphate-sensitive potassium channel
expression in the blood-brain tumor barrier in a rat brain tumor
model. Brain Res. 1162:1–8. 2007.
|
|
24
|
Zhang P, Hu L, Yin Q, Feng L and Li Y:
Transferrin-modified c[RGDfK]-paclitaxel loaded hybrid micelle for
sequential blood-brain barrier penetration and glioma targeting
therapy. Mol Pharm. 9:1590–1598. 2012.
|
|
25
|
Gidwani M and Singh AV: Nanoparticle
enabled drug delivery across the blood brain barrier: in vivo and
in vitro models, opportunities and challenges. Curr Pharm
Biotechnol. 14:1201–1212. 2014.
|
|
26
|
Torchilin V: Antibody-modified liposomes
for cancer chemotherapy. Expert Opin Drug Deliv. 5:1003–1025.
2008.
|
|
27
|
Gastaldi L, Battaglia L, Peira E, et al:
Solid lipid nanoparticles as vehicles of drugs to the brain:
Current state of the art. Eur J Pharm Biopharm. 87:433–444.
2014.
|
|
28
|
Wohlfart S, Gelperina S and Kreuter J:
Transport of drugs across the blood-brain barrier by nanoparticles.
J Control Release. 161:264–273. 2012.
|
|
29
|
Hu K, Li J, Shen Y, et al:
Lactoferrin-conjugated PEG-PLA nanoparticles with improved brain
delivery: in vitro and in vivo evaluations. J Control Release.
134:55–61. 2009.
|
|
30
|
Farnsworth RH, Lackmann M, Achen MG and
Stacker SA: Vascular remodeling in cancer. Oncogene. 33:3496–3505.
2014.
|
|
31
|
Jiang X, Xin H, Gu J, et al: Solid tumor
penetration by integrin-mediated pegylated poly(trimethylene
carbonate) nanoparticles loaded with paclitaxel. Biomaterials.
34:1739–1746. 2013.
|
|
32
|
Thoma CR, Zimmermann M, Agarkova I, Kelm
JM and Krek W: 3D cell culture systems modeling tumor growth
determinants in cancer target discovery. Adv Drug Deliv Rev.
69–70:29–41. 2014.
|