Introduction
Primary penile lymphoma presenting with priapism as
the initial symptom is extremely rare, with few cases reported
worldwide. Penile cancer accounts for only 0.4–0.6% of all
malignancies in the developed world (1), and the involvement of lymphoma is even
more rare. The first case of primary malignant lymphoma of the
penis was reported in 1962 (2), and
few cases have been reported since. The most common subtype is
diffuse large B-cell lymphoma (3).
The diagnosis of rare lymphoma is difficult and may be delayed
without specific symptoms and thus, treatment of this lesion
remains controversial. Chemotherapy is the main treatment
adminstered, however, immunotherapy, radiotherapy and penile
preservation have all been reported (3,4) and a
combined treatment modality is usually recommended (5). The current study reports a patient
diagnosed with primary malignant penile lymphoma, with metastasis
in the lungs and brain, and poor prognosis. The diagnosis was
confirmed by biopsy, and enhanced CT of chest revealed evidence of
pulmonary and brain metastasis. Written informed consent was
obtained from the patient.
Case report
A 48-year-old male presented to Yantai Yuhuanding
Hospital Affiliated to Qingdao University (Yantai, China) with a
one-month history of painless priapism associated with chest
congestion and shortness of breath. The patient had a history of
type II diabetes. Physical examination revealed a swollen penis,
enlarged inguinal lymph nodes, swelling in the thighs and varicose
veins, which were visible in the lower limbs. No fever, night
sweats or weight loss were observed in the month prior to patient
referral, and no symptoms of ulceration, difficulty in urination or
complaint of any epidermal changes were observed; therefore, no
systemic symptoms of lymphoma were presented. Norepinephrine was
administered, however, detumescence did not occur. The B-mode
ultrasound examination of the rectum and perineum and the
arteriography revealed no apparent arteriovenous fistula. An
abdominal and pelvic computed tomography (CT) scan showed multiple
node involvement, including the aortoiliac vessels, neck of the
bladder, seminal vesicle, prostate gland and bilateral inguinal
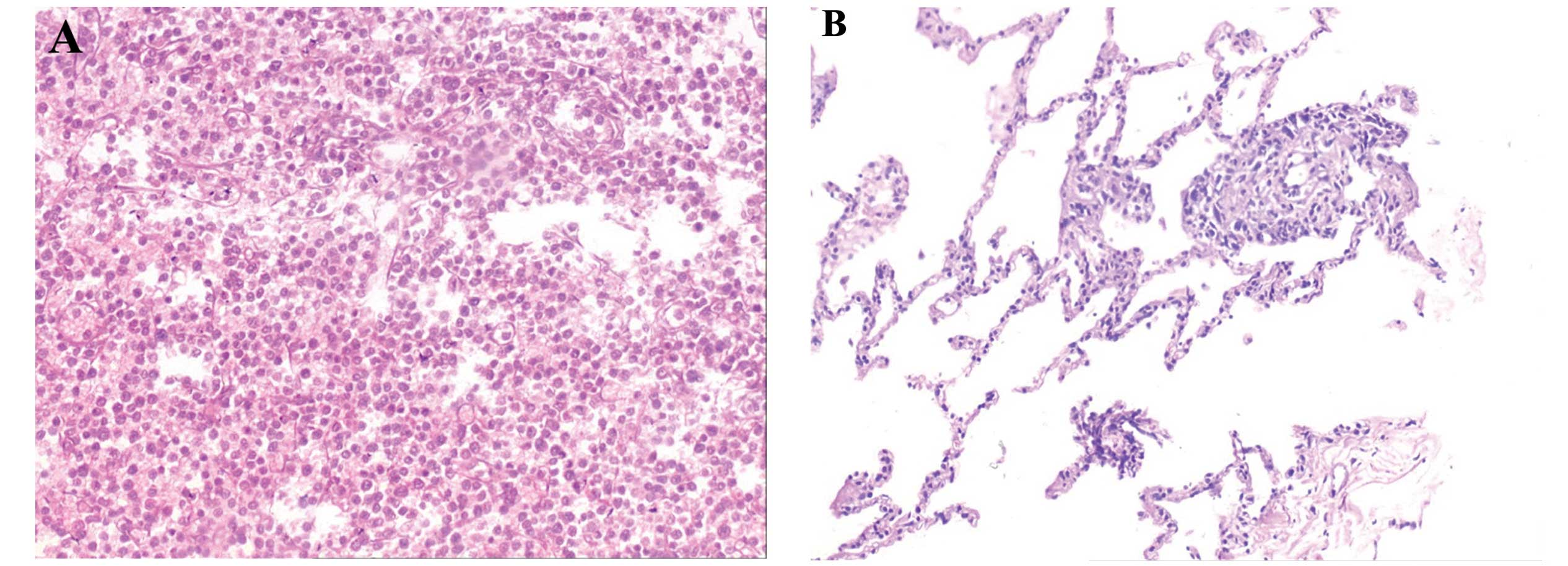
area. A biopsy was taken from the right inguinal lymph node
(1.5×1.5 cm) and immunohistochemical analysis with markers
confirmed that the lymphoma cells were CD20++,
CD3−, CD10−, MuM1− and
bcl-6−, corresponding with non-Hodgkin’s lymphoma
(Fig. 1). The degree of staining
was calculated using the following scale: −, positive staining of
cancerous cells was observed in <25% of the cells; +, positive
staining of cancerous cells was observed in >25% but <50% of
the cells; ++, positive staining of the cancerous cells was
observed in >50% but <75% of the cells (6). Based on these observations, the
diagnosis of diffuse large B-cell lymphoma (DLBCL) was
determined.
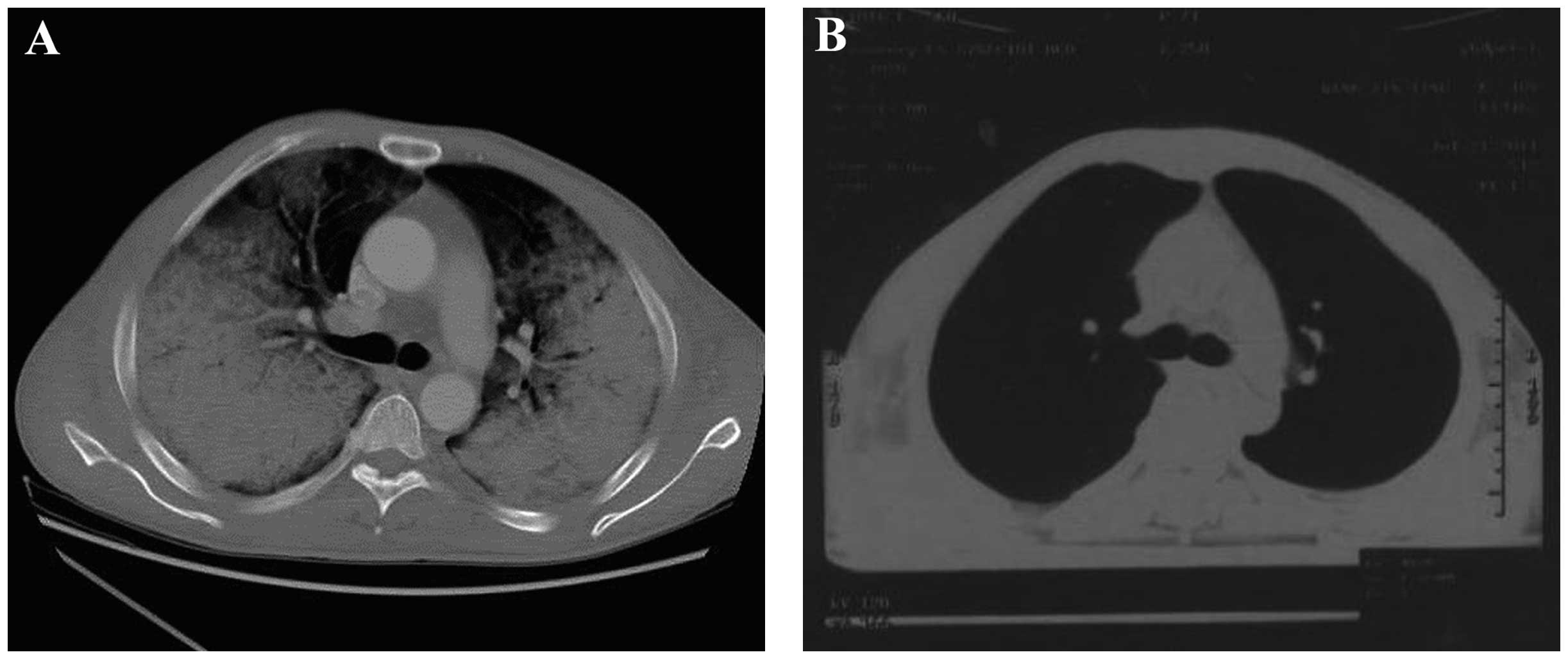
One week following admission, the patient complained
of chest congestion; an enhanced CT scan revealed the invasion of
malignant lymphoma cells to the lungs, and pericardial and
bilateral pleural effusion was also identified (Fig. 2); however, at this stage, the
possibility of fungal infection was not excluded. The E-CHOP
regimen was administered (1.2 mg cyclophosphamide, day one; 2 mg
vincristine, 60 mg epirubicin, days one to two; 100 mg
prednisolone, days one to five; and 0.1 mg etoposide, days one to
five). After four days, chest congestion, edema in the limbs and
priapism were moderately relieved. A further histology of the lung
by a needle biopsy revealed lymphoma cell infusion. Treatment for
the decreased white blood cell count (0.56×109 cells/l;
normal range, 4–10×109 cells/l) was administered during
the second course of chemotherapy. The patient was continuously
treated with systemic chemotherapy with the E-CHOP regimen.
Concomitantly, symptomatic treatment to relieve airway spasms was
administered. The patient tolerated the entire course of
chemotherapy well, and the priapism was alleviated two days
following the completion of one cycle of E-CHOP therapy. The
enlarged bilateral inguinal lymph nodes were non-palpable at the
time of completion.
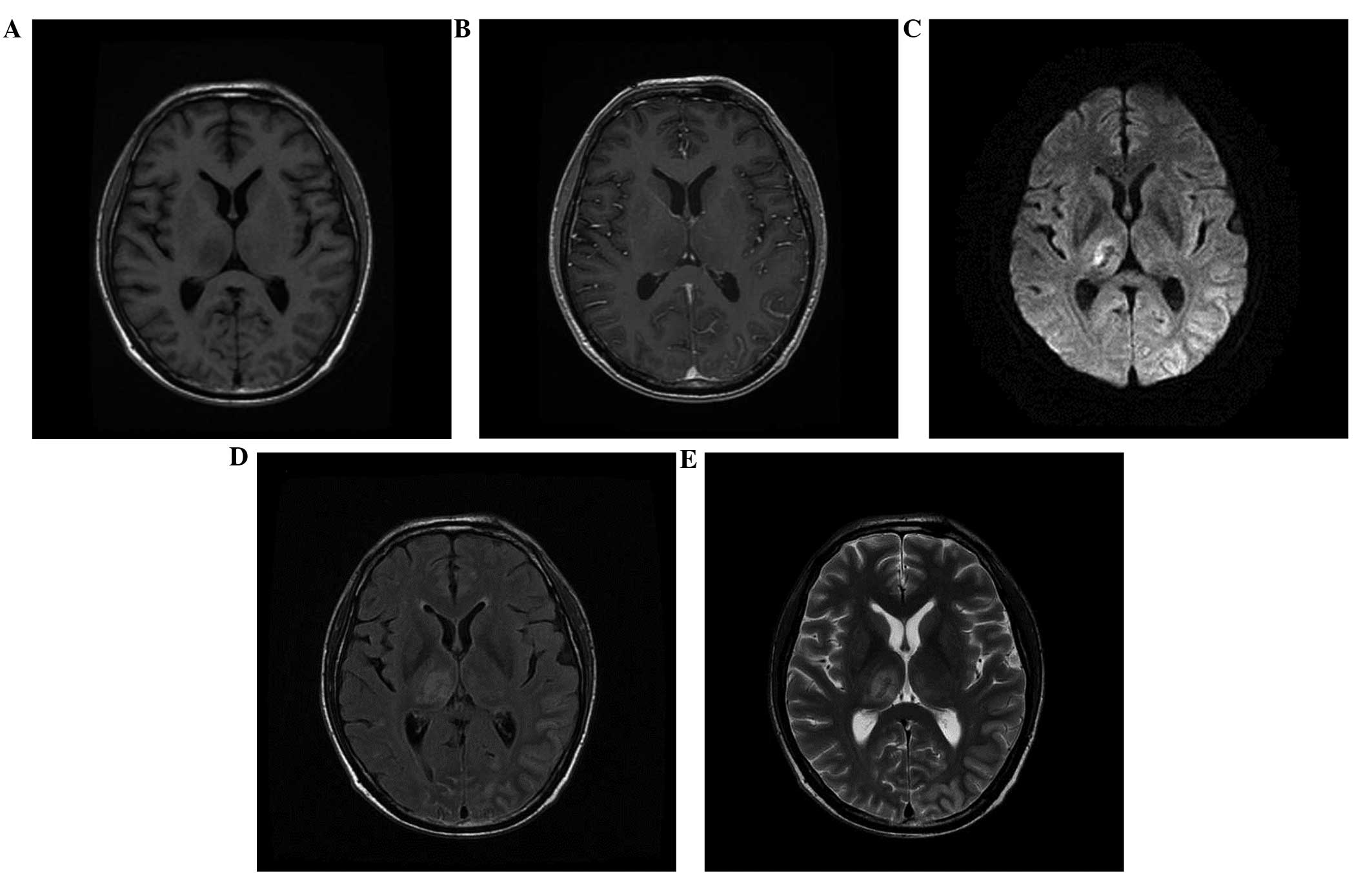
On day 14 following admission, the patient was
unresponsive to external stimuli and suffered an epileptic seizure.
The results of the laboratory evaluations were as follows: Blood
ammonia levels, 18 μmol/l (normal range, 20–60 μmol/l); blood
ketone bodies, negative; and blood sugar levels, 17.27 mmol/l
(normal range, 3.9–7.5 mmol/l); therefore, DKA and hepatic
encephalopathy were ruled out. A cranio-cerebral magnetic resonance
imaging scan revealed an anomaly in the rear of the anterior and
posterior pituitary, suggesting possible cranial nerve nuclei
involvement and infiltration (Fig.
3). The patient was subjected to radiotherapy when brain
metastasis was identified. Systemic treatment for cerebral edema
(dehydration) and nutrition following severe epileptic seizures
were also administered. The final diagnosis was stage IV diffuse
large B-cell non-Hodgkin’s lymphoma with metastasis to the brain
and lungs, according to the Ann Arbor-Cotswolds staging
classification (7). The patient
succumbed to the disease three months following the initial
diagnosis of lymphoma.
Discussion
Priapism is defined as an involuntary, usually
painful, prolonged penile erection unrelated to sexual stimulation
(8). It is most commonly caused by
hematological disorders such as sickle cell anemia; however, other
causes include neurological damage, trauma, infection, malignancy,
erectile dysfunction drugs, such as papaverine and alprostadil, and
metabolic disturbances (9). The
presentation of penile lymphoma varies, with symptoms including
indurated papules, nodules, ulcers and diffuse penile swelling
(10). Primary penile lymphoma is
extremely rare and difficult to diagnose, and patient history must
be carefully assessed. In order to determine an accurate diagnosis,
a full physical examination, radiological imaging studies, excision
biopsy and immunohistochemical analysis must be conducted. Reports
have been published describing this malignancy with common
phenotypes including nodules, ulceration or penile enlargement, all
of which are similar to other soft tissue tumors and, therefore,
lead to the condition being difficult to diagnose (3). However, priapism as the initial
symptom of lymphoma is extremely rare. To the best of our
knowledge, only four cases of primary penile lymphoma have been
reported presenting with priapism as the initial symptom (11–13).
The pathological studies demonstrated that all cases were diffuse
large DLBCL, which is the most common subtype of lymphoma at this
anatomical site (14).
In the current study, the 48-year-old male initially
presented with priapism, which was followed by enlargement of the
lymph node. The pathological studies confirmed the diagnosis of
malignant penile lymphoma and treatment with the E-CHOP regimen led
to the remission of the physiological symptoms; however, the
patient later developed metastasis in the lungs and brain. This
indicated a poor prognosis for DLBCL, the most common subtype of
non-Hodgkin’s lymphoma. DLBCL is aggressive and is associated with
a wide range of clinical manifestations at all ages; however,
patients with the condition may undergo complete remission with
appropriate treatment (11,12,15,16).
It was speculated that priapism in lymphoma is caused by tumor
cells infiltrating the penile cavernous tissue, which causes venous
obstruction and priapism (10).
Priapism caused by tumor cell infiltration is usually associated
with congestion and swelling in the body of penis. Additionally,
priapism as the initial manifestation has been reported in
leukemia, which is also a malignant hematological disease. Often,
priapism subsides after two to seven days of chemotherapy; however,
occasionally it is caused by tumor lysis syndrome in leukemia,
where the condition occurs following chemotherapy (13,17).
To achieve an improved outcome in cases where the original
diagnostic evidence is limited or current treatment failed, the
possibility of lymphoma must be investigated. Furthermore, it has
been suggested that levels of soluble interleukin-2 receptor may
serve as a potential prognostic marker for the low complete
response rates in DLCBL (16,18).
To date, the preferred treatment for DLCBL includes
excision, radiotherapy, and chemotherapy; however, no standard
treatment modality has been established (16). Although early-stage localized
lymphoma is potentially curable with localized therapy and has a
good prognosis, the anatomical resection and radiotherapy may cause
local morbidity. The E-CHOP regimen alone, or combined with
rituximab, which is a chimeric monoclonal antibody against the CD20
B-cell antigen, has become the current recommended treatment for
DLBCL. In the majority of reported cases, following chemotherapy
treatment, complete resolution of the disease was observed for
between four months and six years (10,15,19–26).
However mortalities due to this malignancy have also been reported
(21).
In conclusion, the current study reports the case of
a 48-year-old male with primary penile lymphoma, presenting with a
one-month history of priapism due to large DLBCL cell infiltration,
which also affected the lungs and cranial nervous system. The
diagnosis was prolonged as the initial manifestation of the disease
was extremely rare. The E-CHOP chemotherapy regimen was the
selected treatment modality in this case, considering the patient’s
relatively young age, due to the vigorous nature of the therapy.
However, the prognosis was poor due to the advanced stage of the
invasion and disseminated lymphoma cells. This case report may
increase understanding with regard to the specific aetiology and
pathogenesis of this disease and may prevent misdiagnosis by
clinicians. Non-Hodgkin’s lymphoma may be difficult to diagnose
based on the initial symptoms presented by patients. Thus, early
recognition and appropriate clinical management are required.
Further clinical studies are required to identify a standard
treatment for this malignancy.
Acknowledgements
This study was supported by the Shandong Doctoral
Program fund (grant no. 2008BS02012) and the Yantai Science and
Technology Program (grant no. 2009155-3).
References
|
1
|
Bleeker MC, Heideman DA, Snijders PJ, et
al: Penile cancer: epidemiology, pathogenesis and prevention. World
J Urol. 27:141–150. 2009.
|
|
2
|
Oomura J, Ookita K, Takenaka M and Yamada
S: Primary reticulosarcoma of the penis. Report of a case.
Hinyokika Kiyo. 8:53–542. 1962.(In Japenese).
|
|
3
|
Chu L, Mao W, Curran Vikramsingh K, et al:
Primary malignant lymphoma of the glans penis: a rare case report
and review of the literature. Asian J Androl. 15:571–572. 2013.
|
|
4
|
Delicato G, Baffigo G, Bianchi D, et al:
Conservative therapy in two cases of non-Hodgkin lymphoma of the
penis: Case reports with review of the literature. World J Oncol.
3:37–38. 2012.
|
|
5
|
Arena F, di Stefano C, Peracchia G, et al:
Primary lymphoma of the penis: diagnosis and treatment. Eur Urol.
39:232–235. 2001.
|
|
6
|
Vardiman JW, Thiele J, Arber DA, et al:
The 2008 revision of the World Health Organization (WHO)
classification of myeloid neoplasms and acute leukemia: rationale
and important changes. Blood. 114:937–951. 2009.
|
|
7
|
Izumi T and Ozawa K: Clinical
classification of non-Hodgkin’s lymphoma. Nihon Rinsho. 58:598–601.
2000.(In Japenese).
|
|
8
|
Salonia A, Eardley I, Giuliano F, et al:
European Association of Urology guidelines on priapism. Eur Urol.
65:480–489. 2014.
|
|
9
|
Van der Horst C, Stuebinger H, Seif C, et
al: Priapism - etiology, pathophysiology and management. Int Braz J
Urol. 29:391–400. 2003.
|
|
10
|
Kim HY, Oh SY, Lee S, et al: Primary
penile diffuse large B cell lymphoma treated by local excision
followed by rituximab-containing chemotherapy. Acta Haematol.
120:150–152. 2008.
|
|
11
|
Guo Y, Bai RJ and Gao S: FDG PET/CT
detects malignant lymphoma invading the penis. Clin Nucl Med.
36:e204–206. 2011.
|
|
12
|
Madeb R, Rub R, Erlich N, Hegarty PK and
Yachia D: Long standing priapism as presentation of lymphoma. Am J
Hematol. 82:872007.
|
|
13
|
Hamamoto S, Tozawa K, Nishio H, Kawai N
and Kohri K: Successful treatment of primary malignant lymphoma of
the penis by organ-preserving rituximab-containing chemotherapy.
Int J Clin Oncol. 17:181–184. 2012.
|
|
14
|
Sun J, Medeiros LJ, Lin P, Lu G,
Bueso-Ramos CE and You MJ: Plasmablastic lymphoma involving the
penis: a previously unreported location of a case with aberrant CD3
expression. Pathology. 43:54–57. 2011.
|
|
15
|
Wei CC, Peng CT, Chiang IP and Wu KH:
Primary B cell non-hodgkin lymphoma of the penis in a child. J
Pediatr Hematol Oncol. 28:479–480. 2006.
|
|
16
|
Marks D, Crosthwaite A, Varigos G, Ellis D
and Morstyn G: Therapy of primary diffuse large cell lymphoma of
the penis with preservation of function. J Urol. 139:1057–1058.
1988.
|
|
17
|
Asakura H, Nakazono M, Masuda T, Yamamoto
T and Tazaki H: Priapism with malignant lymphoma: a case report.
Hinyokika Kiyo. 35:1811–1814. 1989.(in Japanese).
|
|
18
|
Arena F, di Stefano C, Peracchia G,
Barbieri A and Cortellini P: Primary lymphoma of the penis:
diagnosis and treatment. Eur Urol. 39:232–235. 2001.
|
|
19
|
Delicato G, Baffigo G, Bianchi D, Farullo
G, Signore S, Tartaglia E, Corvese F and Ferdinandi V: Conservative
therapy in two cases of non-Hodgkin lymphoma of the penis:
Casereports with review of the literature. World J Oncol. 3:37–38.
2012.
|
|
20
|
Carter RD, Smith R, Alpern HD and Healey
BM: Primary lymphoma of the penis with rationale of treatment. Int
Urol Nephrol. 24:521–525. 1992.
|
|
21
|
el-Sharkawi A and Murphy J: Primary penile
lymphoma: the case for combined modality therapy. Clin Oncol (R
Coll Radiol). 8:334–335. 1996.
|
|
22
|
Gallardo F, Pujol RM, Barranco C and Salar
A: Progressive painless swelling of glans penis: uncommon clinical
manifestation of systemic non-Hodgkin’s lymphoma. Urology.
73:e3–e5. 2009.
|
|
23
|
Wang HT, Lo YS and Huang JK: Primary
lymphoma of the penis. J Chin Med Assoc. 66:379–381. 2003.
|
|
24
|
Pomara G, Cuttano MG, Tripodo C, Carlino F
and Selli C: Primary T-cell rich B-cell lymphoma of the penis: a
first case. BJU Int. 91:8892003.
|
|
25
|
Hashine K, Akiyama M and Sumiyoshi Y:
Primary diffuse large cell lymphoma of the penis. Int J Urol.
1:189–190. 1994.
|
|
26
|
Terada T, Shirakashi Y and Sugiura M:
T-cell lymphoma of the penis as the first manifestation of adult
T-cell lymphoma/leukemia. Int J Dermatol. 51:973–975. 2012.
|