Introduction
Cancer is the leading cause of mortality in children
between the ages of 6 months and 15 years in the USA and annually
>7,000 new cases of cancer are diagnosed in children <15
years of age (1).
Leukemia comprises ~25% of all childhood cancers,
followed by tumors of the central nervous system (17%),
neuroblastoma (7%), non-Hodgkin lymphoma (NHL) (6%), Wilm’s tumor
(6%), Hodgkin disease (5%), rhabdomyosarcoma (3%), retinoblastoma
(3%), osteosarcoma (3%) and Ewing sarcoma (2%). Numerous additional
rare tumor types account for the remainder. These values are with
regard to patients ≤15 years of age, worldwide (2).
During the past 30 years, improvements in the
survival rates for infants and children with different types of
cancer have been observed. In the 1960s, ~50% of all children with
malignant tumors succumbed to the disease, compared with a 75%
overall survival rate today (3).
The improved outcomes were associated with the establishment of
well-designed national multidisciplinary cooperative studies, which
were conducted in various pediatric cancer centers, using combined
treatment modalities, including surgery, chemotherapy and
irradiation (4). The availability
of new imaging techniques was also significant in identifying the
extent of tumors and determining staging. The most improved
relative survival rates have been achieved in patients with acute
lymphocytic leukemia, NHL and Wilm’s tumor (3).
The aim of the current study was to evaluate the
patterns, frequency and outcome of solid tumors and lymphomas in
children admitted to and followed up in the Pediatric Oncology
Department of Zagazig University Hospital (Zagazig, Egypt) over a
duration of 5 years (January 2004–December 2008).
Materials and methods
A retrospective study was conducted, which included
155 children with solid tumors and lymphomas who were admitted to
and followed up in this department between January 2004 and
December 2008.
All medical records were reviewed and a standardized
data abstraction form was designed to capture the appropriate
information with regard to the demographic, clinical,
histopathological, laboratory and imaging data, as well as the
treatment plan and outcome.
Statistical analysis
The data obtained for each patient were added to a
computerized database in SPSS, version 14 (SPSS, Inc., Chicago, IL,
USA). A descriptive analysis was performed for each variable
included and correlations between these variables, and the outcome
were analyzed using the appropriate statistical method. Data are
presented as the mean ± standard deviation for quantitative
variables, and as a value and percentage for qualitative variables.
The χ2, analysis of variance (f) tests were used where
appropriate, and P<0.05 was considered to indicate a
statistically significant difference.
Ethics
The study was performed in accordance with the
ethical standards of the 1964 Declaration of Helsinki, as revised
in 2000 (5). The study was approved
by the ethics committee of Zagazig University (Zagazig, Eygpt).
Results
The frequency of tumors, age groups and gender
distributions are shown in Table I.
The mean age of patients at diagnosis was 5.6±3.04 years. The most
commonly involved age group was <5 years (60.0%) and the least
common was >10 years (12.3%). Neuroblastoma was the most common
cancer in early childhood (38.7% of tumors in children <5 years
old), while NHL occurred most frequently in the older age groups
(39.5% of tumors in children aged between 5 and 10 years old and
36.8% of tumors in children ≥10 years old).
 | Table IDemographic characteristics of
patients stratified by tumor type. |
Table I
Demographic characteristics of
patients stratified by tumor type.
| | | Age groups, n
(%) | Gender, n (%) |
|---|
| | |
|
|
|---|
| Tumor | Frequency, n (%) | Mean age, y | <5 y | ≥5, <10 y | ≥10 y | Male | Female |
|---|
| NHL | 48 (31.0) | 6.6±4.1 | 24 (25.8) | 17 (39.5) | 7 (36.8) | 33 (35.1) | 15 (24.6) |
| Neuroblastoma | 45 (29.0) | 3.7±2.1 | 36 (38.7) | 7 (16.3) | 2 (10.5) | 22 (23.4) | 23 (37.7) |
| HL | 27 (17.4) | 6.2±3.9 | 15 (16.1) | 10 (23.3) | 2 (10.5) | 17 (18.1) | 10 (16.4) |
| Wilm’s tumor | 15 (9.7) | 4.9±2.3 | 8 (8.6) | 7 (16.3) | 0 (0.0) | 8 (8.5) | 7 (11.7) |
| Rhabdomyosarcoma | 8 (5.2) | 6.8±3.9 | 4 (4.3) | 1 (2.3) | 3 (15.8) | 5 (5.3) | 3 (4.8) |
| Bone tumors | 7 (4.5) | 10±4.5 | 2 (2.2) | 0 (0.0) | 5 (26.3) | 5 (5.3) | 2 (3.2) |
| Brain tumors | 3 (1.9) | 3.3±2.3 | 2 (2.2) | 1 (2.3) | 0 (0.0) | 2 (2.2) | 1 (1.6) |
| Hepatoblastoma | 2 (1.3) | 1.2±0.4 | 2 (2.2) | 0 (0.0) | 0 (0.0) | 2 (2.2) | 0 (0.0) |
| Total number | 155 | - | 93 | 43 | 19 | 94 | 61 |
| Test | - | F=5.24 | |
χ2=25.12 | |
χ2=6.02 | |
| P-value | - | P<0.001 | | P<0.05 | | P>0.05 | |
The patients comprised 94 males (60.6%) and 61
females, (39.4%), with a male to female ratio of 1.5:1. NHL was the
most common tumor in males (35.1%), whilst for females, it was
neuroblastoma (37.7%). For the entire cohort, NHL was the most
prevalent followed by neuroblastoma (31.0 and 29.0%, respectively).
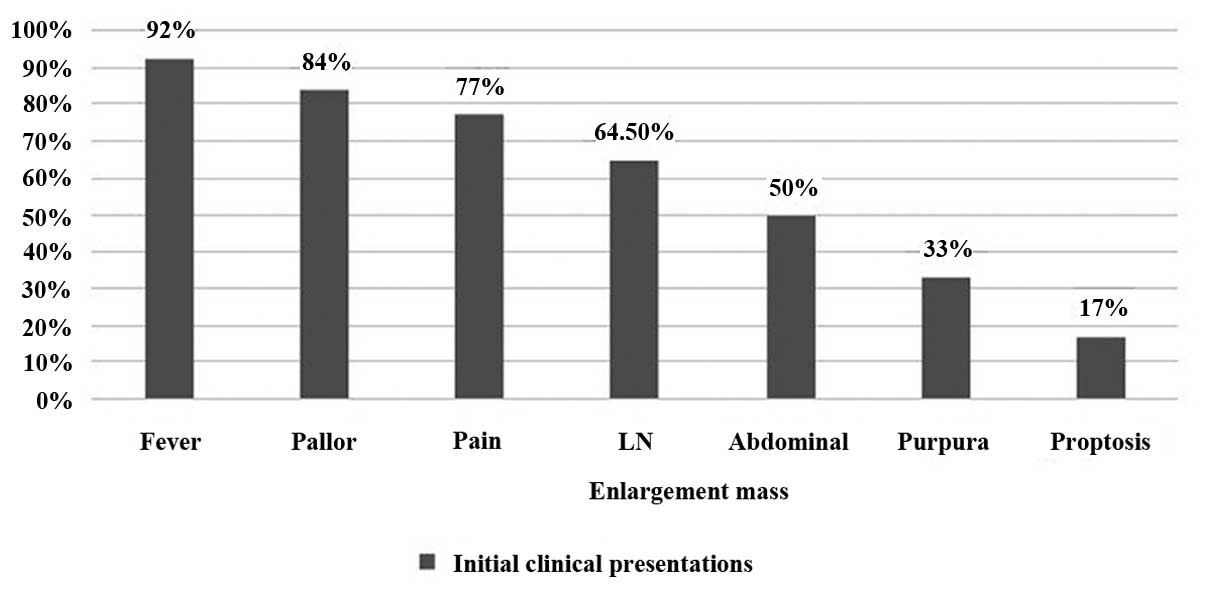
The most frequently observed primary tumor sites were the abdomen
(41.3%), head and neck (22.6%) and mediastinum (16.7%). Fever,
pallor and pain were the most common initial clinical presentations
among the patients (Fig. 1; 91.6,
83.9 and 77.4%, respectively).
Of the 155 patients, the tumor stage was only known
for 143 cases. Stage II was the most common stage (39.1%) followed
by stage IV, III and I (35.0, 20.3 and 5.6% respectively) (Table II). Complete results with regard to
the outcome were available for 129 patients. The overall 5-year
survival rate was 66.7%. No significant differences were identified
between the various age groups and between males and females with
regard to the 5-year survival rate (P>0.05). Conversely, a
significant correlation was observed between tumor stage and the
5-year survival rate, where the 5-year survival rate was
significantly higher in patients with stages I and II (100 and 84%,
respectively; P<0.001) and significantly lower in stage IV
patients (43%; P<0.001) (Table
III). The correlation between the 5-year survival rate and
tumor type is shown in Table IV.
The 5-year survival rate was significantly higher in patients with
Wilm’s tumor and Hodgkin lymphoma followed by NHL (92, 88 and 72%,
respectively; P<0.001), while the mortality rate was
significantly higher in patients with neuroblastoma
(P<0.001).
 | Table IITumor stages in the patients. |
Table II
Tumor stages in the patients.
| Tumor | Stage I, n (%) | Stage II, n (%) | Stage III, n (%) | Stage IV, n (%) |
|---|
| NHL | 1 (12.5) | 21 (37.5) | 14 (48.3) | 12 (24.0) |
| HL | 4 (50.0) | 11 (19.6) | 6 (20.7) | 6 (12.0) |
| Neuroblastoma | 0 (0.0) | 15 (26.8) | 6 (20.7) | 20 (40.0) |
| Wilm’s tumor | 1 (12.5) | 6 (10.7) | 1 (3.4) | 4 (8.0) |
| Rhabdomyosarcoma | 2 (25.0) | 0 (0.0) | 0 (0.0) | 6 (12.0) |
| Brain tumors | 0 (0.0) | 1 (1.8) | 1 (3.4) | 0 (0.0) |
| Bone tumors | 0 (0.0) | 2 (3.6) | 1 (3.4) | 1 (2.0) |
| Hepatoblastoma | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.0) |
| Total number | 8 | 56 | 29 | 50 |
 | Table IIICorrelation between the outcome and
various parameters. |
Table III
Correlation between the outcome and
various parameters.
| Age group, n (%) | Gender, n (%) | Stage, n (%) |
|---|
|
|
|
|
|---|
| Outcome | <5 y | ≥5, <10 y | ≥10 y | Male | Female | Stage I | Stage II | Stage III | Stage IV |
|---|
| Survivors | 49 (62.0) | 26 (76.0) | 11 (69.0) | 55 (70.0) | 31 (62.0) | 8 (100.0) | 43 (84.0) | 16 (61.5) | 19 (43.0) |
| STD | 30 (38.0) | 8 (24.0) | 5 (31.0) | 24 (30.0) | 19 (38.0) | 0 | 8 (16.0) | 10 (38.5) | 25 (57.0) |
| Total number | 79 | 34 | 16 | 79 | 50 | 8 | 51 | 26 | 44 |
| Test | |
χ2=2.27 | | |
χ2=0.8 | | |
χ2=22.37 | |
| P value | | P>0.05 | | | P>0.05 | | | <0.001 | |
 | Table IVCorrelation between the outcome and
various types of tumors. |
Table IV
Correlation between the outcome and
various types of tumors.
| Outcome | NHL | Neuroblastoma | HL | Wilm’s | Rhabdomyosarcoma | Brain tumor | Bone tumor | Hepatoblastoma |
|---|
| Survivors | 31 (72) | 12 (34) | 23 (88) | 11 (92) | 4 (67) | 1 (100) | 3 (75) | 1 (50) |
| STD | 12 (28) | 23 (66) | 3 (12) | 1 (8) | 2 (33) | 0 | 1 (25) | 1 (50) |
| Total number | 43 | 35 | 26 | 12 | 6 | 1 | 4 | 2 |
| Test | | | | |
χ2=26.89 | | | |
| P-value | | | | | P<0.001 | | | |
Discussion
Current statistics on the occurrence and outcome of
cancer cases are essential for the planning and evaluation of
programs for cancer control. The present study collected a database
of pediatric malignant solid tumors and lymphomas from the only
reference pediatric center in the Zagazig region of Egypt, with the
aim of analyzing the patterns, frequency and outcomes of these
tumors.
The study investigated 155 children with malignant
solid tumors and lymphomas over a duration of 5 years, yielding a
mean of 31 cases per year. An exact incidence rate cannot be
provided by a study based in a single hospital (Pediatrics
Department, Zagazig University); however, the information is useful
in revealing patterns of childhood malignancies in this region.
In the current study, NHL was the most common tumor
followed by neuroblastoma and Hodgkin lymphoma (31.0, 29.0 and
17.4%, respectively). Agboola et al (6) reported 77 children with malignant
tumors, and observed that lymphomas were the most prevalent
malignancy identified, accounting for 31 diagnoses (40%). Burkitt’s
lymphoma accounted for the majority of malignancies (28 cases;
36%), followed by retinoblastoma (16 cases; 21%) and Wilm’s tumor
(11 cases; 14%).
Following the exclusion of leukemia, a report from a
hospital-based registry by the Italian Association of Pediatric
Hematology and Oncology demonstrated that NHL was the most common
tumor (7). Memon et al
(8) investigated 113 cases of
malignant solid tumors in children; the results indicated that
retinoblastoma was the most common malignant solid tumor, followed
by Wilm’s tumor (38.9% and 13.2%, respectively). Furthermore,
Akinde et al (9) in their
retrospective review on diagnosed cases of childhood tumors
observed between January 2000 and 2007 from the records of Lagos
University Teaching Hospital in Nigeria, found that malignant
tumors constituted 30.50% of childhood tumors of which
retinoblastoma was the most common.
The low incidence of brain tumors in the current
study was due to the referral of the majority of patients with
brain tumors to the Neurosurgery Department, where surgery and
radiotherapy were the recommended treatment options. This was also
observed in patients with bone tumors.
The current study revealed male preponderance, with
an overall male to female ratio of 1.5:1. This is marginally lower
than that reported in another Egyptian study (10) where the male to female ratio was
1.6:1, and slightly higher than that reported in a Turkish study
(11), where the male to female
ratio was 1.4:1. However, the ratio observed in the current study
was significantly higher than the 1.1:1 reported in a Mexican study
(12).
The majority of the patients included in the current
study were <5 years of age at diagnosis (58.7%). Juárez-Ocaña
et al (12)found that the
highest frequency of cancer was identified in the group of 1- to
4-year-olds (36.8%). Furthermore, the results presented in the
current study, with regards to the age of patients at diagnosis,
are consistent with a number of other studies (7,13,14).
The majority of patients in the current study
initially presented with fever, pallor and pain (91.6, 83.9, and
77.4%, respectively). Lymph node enlargement was the most frequent
symptom among children with lymphoma and abdominal mass was the
most common among children with neuroblastoma and Wilm’s tumor. Gao
et al (15) reported that
the initial symptoms among 63 patients with advanced neuroblastoma
included fever, abdominal pain, abdominal mass and leg or articular
pain.
The majority of patients in the current study were
stage II (39.1%), followed by stage IV, III and I (35, 20.3 and
5.6%, respectively). The frequency of cancer stages had been
previously analyzed in a number of studies (12,16,17).
In a large Mexican study (12), a
total of 1,702 new cases of cancer in children were registered
between 1996 and 2001. The majority of cases were stage III (36.8%)
followed by stage IV, II and I (30.1, 19.6 and 13.5%,
respectively). A high percentage (66.9%) of Mexican children were
of stage III or IV at the time of diagnosis, which is marginally
higher than the 55.7% of patients with stage III or IV cancer in
the present study. The increased incidence of advanced-stage cases
in the present study and that by Juárez-Ocaña et al
(12) was explained by the
unawareness of general practitioners and parents of the early
symptoms of these types of cancer.
The overall 5-year survival rate in the current
study was 66.7%. Vasudevan et al (14) reported a 10-year overall survival
rate of 41.5%. According to the National Cancer Institute (NCI)
(16), the 5-year survival rate for
all childhood cancers (including leukemia) combined is nearing 81%.
Inclusion of leukemia in NCI results may explain the increased
5-year survival rate in NCI compared with the current study.
The 5-year survival rate was significantly higher in
patients with Wilm’s tumor and Hodgkin lymphoma, followed by NHL
(92.0, 88.0 and 72.0%, respectively), while the mortality rate was
significantly higher in patients with neuroblastoma. These results
are consistent with a number of studies (14,16,17).
Since the 1990s, the 5-year survival rates for Wilm’s tumor and
Hodgkin lymphoma have exceeded 90% (17). The 5-year survival rate for children
<15 years of age with NHL in the USA has improved significantly,
increasing from 45% between 1975 and 1978, to 88% between 1999 and
2002, which is slightly higher than that observed in the current
study (17). Furthermore, Smith
et al (17) reported that
the 5-year survival rates have improved for older children (>1
year) with neuroblastoma in the USA from ~40% prior to 1985, to 65%
between 1999 and 2002, which is relatively low compared with other
childhood cancers. The high mortality rate in neuroblastoma in the
current study may be attributed to the late stage of the disease at
diagnosis, as stages III and IV represented 63.3% of neuroblastoma
cases.
In conclusion, NHL and neuroblastoma were the most
common tumors. The survival rate was higher in patients with Wilm’s
tumor and Hodgkin lymphoma, and lower in patients with
neuroblastoma. A larger multicenter study is required to confirm
these results. The low incidence of brain and bone tumors in the
present study is due to the lack of communication with
neurosurgeons and orthopedic surgeons who are involved primarily in
the treatment of these tumors and hence establishment of tumor
boards must include neurosurgeons and orthopedic surgeons to ensure
accurate registration and team management of patients with brain
and bone tumors.
References
|
1
|
Young JL Jr, Ries LG, Silverberg E, Horm
JW and Miller RW: Cancer incidence, survival and mortality for
children younger than age 15 years. Cancer. 58(2 Suppl): 598–602.
1986.
|
|
2
|
Moore SW, Satgé D, Sasco AJ, Zimmermann A
and Plaschkes J: The epidemiology of neonatal tumours. Report of an
international working group. Pediatr Surg Int. 19:509–519.
2003.
|
|
3
|
Greenlee RT, Murray T, Bolden S and Wingo
PA: Cancer statistics 2000. CA Cancer J Clin. 50:7–33. 2000.
|
|
4
|
Grosfeld JL: Risk-based management:
current concepts of treating malignant solid tumors of childhood. J
Am Coll Surg. 189:407–425. 1999.
|
|
5
|
Christie B: Doctors revise Declaration of
Helsinki. BMJ. 321:9132000.
|
|
6
|
Agboola AO, Adekanmbi FA, Musa AA, et al:
Pattern of childhood malignant tumors in a teaching hospital in
south-western Nigeria. Med J Aust. 190:12–14. 2009.
|
|
7
|
Pession A, Dama E, Rondelli R, et al:
Italian Association of Paediatric Haematology and Oncology:
Survival of children with cancer in Italy, 1989–1998. A report from
hospital based registry of the Italian Association of Pediatric
Hematology and Oncology (AIEOP). Eur J Cancer. 44:1282–1289.
2008.
|
|
8
|
Memon F, Rathi SL and Memon MH: Pattern of
solid paediatric malignant neoplasm at Lumhs, Jamshoro, Pakistan. J
Ayub Med Coll Abbottabad. 19:55–57. 2007.
|
|
9
|
Akinde OR, Abdukareem FB, Daramola AO,
Anunobi CC and Banjo AA: Morphological pattern of childhood solid
tumors in Lagos University Teaching Hospital. Nig Q J Hosp Med.
19:169–174. 2009.
|
|
10
|
Ibrahim AS: Childhood cancer in Egypt:
National cancer Institute, Cairo University and Gharbia population
based registry, Egypt (2000–2002). Pediatr Hematol Oncol. 29:8–9.
2002.
|
|
11
|
Varan A, Büyükpamukçu M, Ersoy F, et al:
Malignant solid tumors associated with congenital immunodeficiency
disorders. Pediatr Hematol Oncol. 21:441–451. 2004.
|
|
12
|
Juárez-Ocaña S, González-Miranda G,
Mejía-Aranguré JM, et al: Frequency of cancer in children
residening in Mexico city and treated in hospital of Instituo of
Mexicano del Segruro Social (1996–2001). BMC Cancer. 13:502004.
|
|
13
|
Valsecchi MG, Tognoni G, Bonilla M, et al:
Monza’s International School of Paediatric Hematology-Oncology:
Clinical epidemiology of childhood cancer in Central America and
Caribbean countries. Ann Oncol. 15:680–685. 2004.
|
|
14
|
Vasudevan V, Cheung MC, Yang R, et al:
Pediatric solid tumors and second malignancies: characteristics and
survival outcomes. J Surg Res. 160:184–189. 2010.
|
|
15
|
Gao XN, Tang SQ and Lin J: Clinical
features and prognosis of advanced neuroblastoma in children.
Zhongguo Dang Dai Er Ke Za Zhi. 9:351–354. 2007.(In Chinese).
|
|
16
|
Ries LAG, Melbert D, Krapcho M, et al:
SEER Cancer Statistics Review, 1975–2004. National Cancer
Institute; Bethesda, MD: http://seer.cancer.gov/csr/1975_2004/.
based on November 2006 SEER data submission, posted to the SEER
website. 2007
|
|
17
|
Smith MA, Seibel NL, Altekruse SF, et al:
Outcomes for children and adolescents with cancer: challenges for
the twenty-first century. J Clin Oncol. 28:2625–2634. 2010.
|