Introduction
Minimal deviation adenocarcinoma (MDA), also known
as adenoma malignum of the uterine cervix, accounts for only ~1% of
adenocarcinomas of the uterine cervix. The main clinical
manifestations are vaginal profuse, watery or mucoid discharge and
irregular bleeding (1). In total,
~10% of MDA is accompanied by Peutz-Jeghers syndrome (2). Using magnetic resonance imaging (MRI),
MDA appears as multilocular lesions with solid components that
extend from the endocervical glands to the deep cervical stroma.
Histopathologically, MDA is composed of mucinous,
well-differentiated glands, deeply invading the cervical stroma,
often surrounded by a desmoplastic reaction. Although MDA exhibits
a benign histological appearance, it is typically characterized by
aggressive clinical behavior. Cytological evaluation and biopsies
have low detection rates, which delays the accurate diagnosis and
leads to a poor prognosis.
The current study describes a rare case of MDA that
was difficult to differentiate from endometrial adenocarcinoma of
the corpus uteri preoperatively, as the endometrial biopsy results
suggested well-differentiated endometrioid adenocarcinoma and MRI
did not show typical images. Surgery was performed under the
diagnosis of endometrial cancer, and the tumor was diagnosed as MDA
of the uterine cervix following pathological examination of the
hysterectomy specimen. Written informed consent was obtained from
the patient.
Case report
A 65-year-old female (gravida 2, para 0) visited a
local clinic due to abnormal vaginal bleeding. A previous history
of surgery for acute appendicitis was recorded at 20 years of age,
and the patient’s family history was unremarkable. Mild ascites and
swelling of an ovary were observed during transvaginal
ultrasonography; therefore, the patient was referred to the
Department of Obstetrics and Gynecology, Osaka City University
Graduate School of Medicine (Osaka, Japan).
On presentation, the patient exhibited a small
volume of bloody vaginal discharge. The uterine corpus was enlarged
to 85 mm in size and the uterine cervix was not enlarged or
abnormal. Transvaginal ultrasonography revealed a small amount of
ascites and mildly thickened endometrium. The fallopian tubes and
ovaries exhibited no abnormalities. A cervical smear was negative
for intraepithelial lesions or malignancy and an endometrial biopsy
revealed a well-differentiated suspected endometrioid
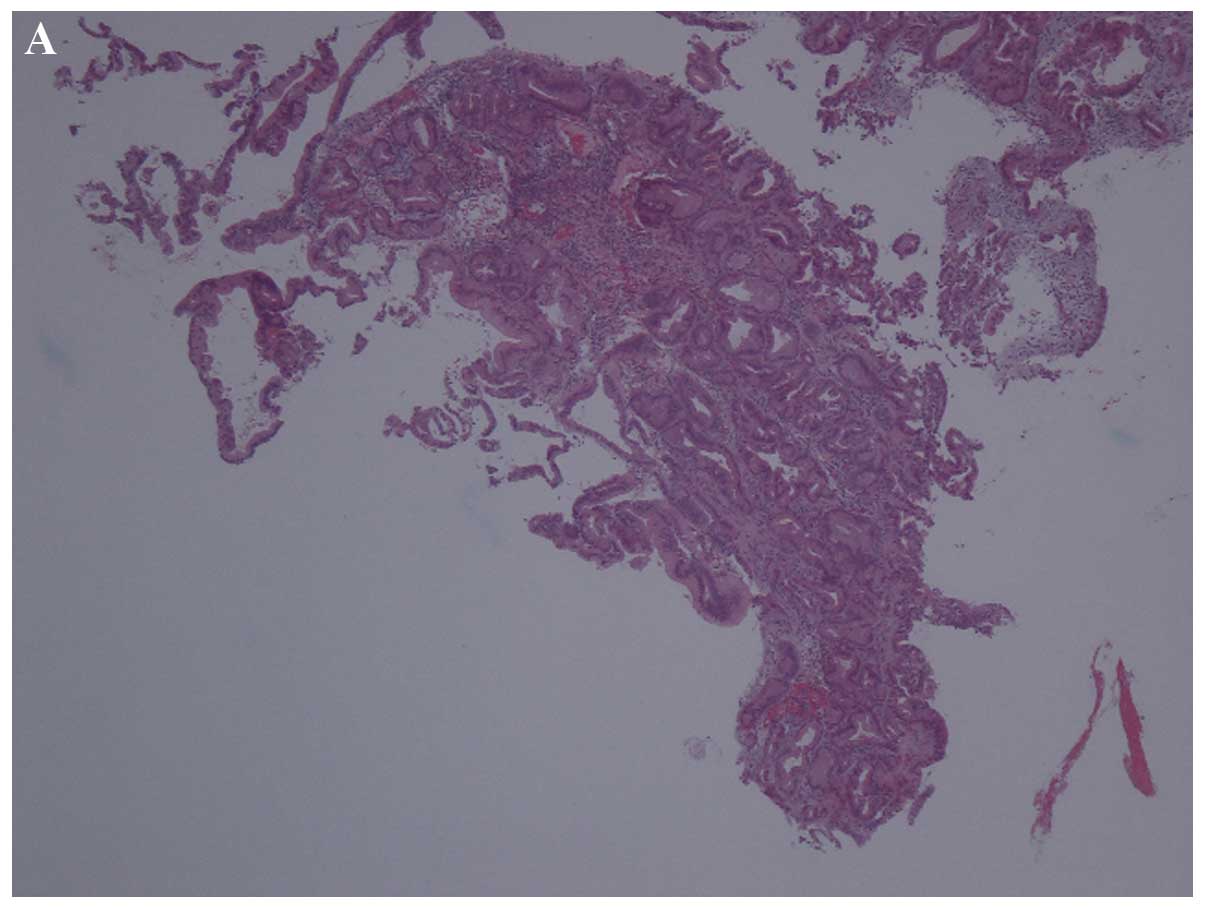
adenocarcinoma (Fig. 1). magnetic
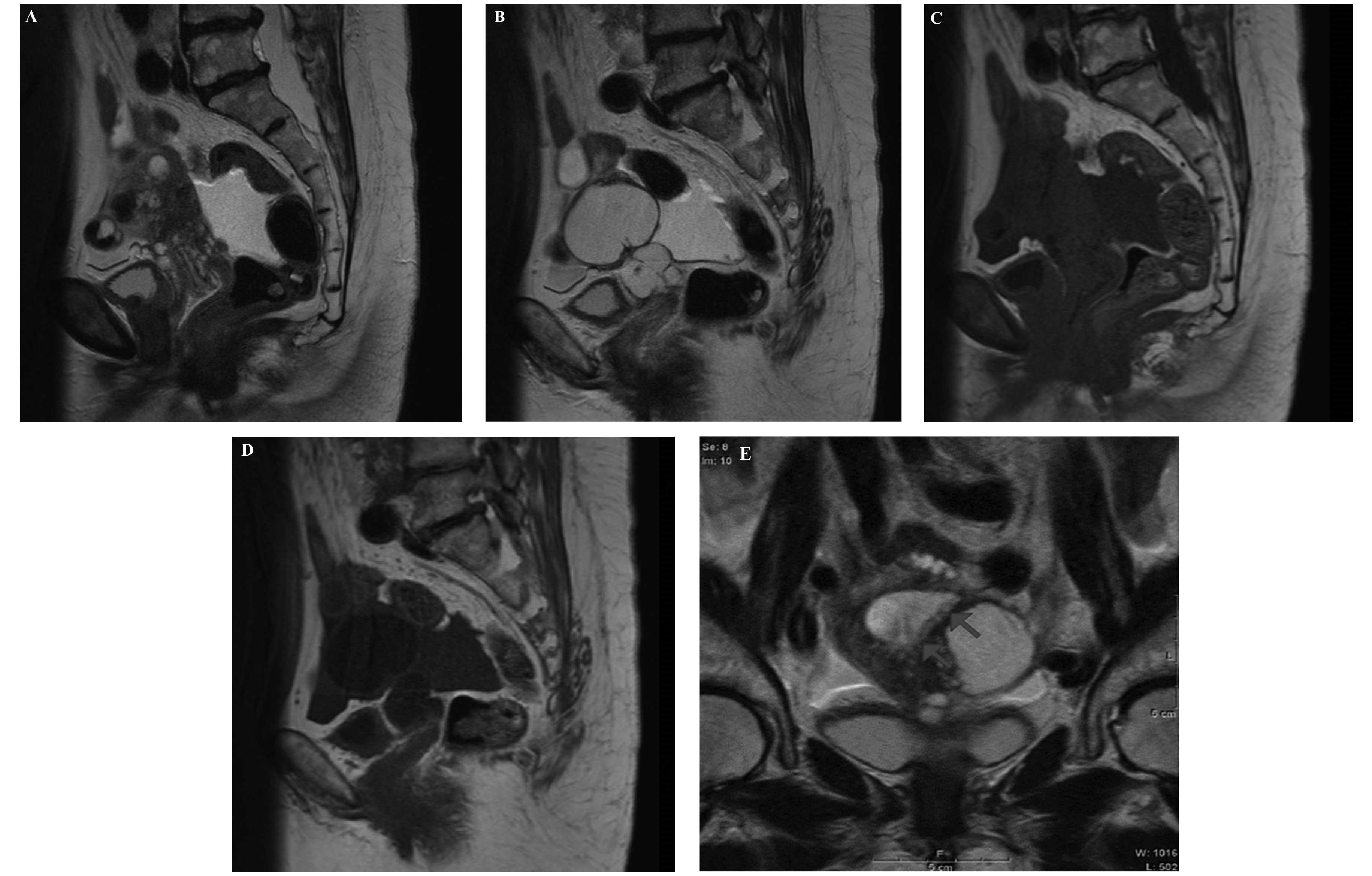
resonance imaging (MRI) revealed mucus retention in the endometrial
cavity and multiple cysts from the uterine corpus to the uterine
cervix, with low intensity on T1-weighted images and high intensity
on T2-weighted images. No enlargement of the uterine cervix was
observed. T2-weighted images revealed a high-intensity area in the
endometrium of the uterine corpus (Fig.
2). A chest CT revealed the enlargement of the supraclavicular
lymph nodes. Serum carbohydrate antigen (CA)-125 levels were 153
U/ml (normal, <35 U/ml) and CA19-9 levels were 44 U/ml (normal,
<37 U/ml), while carcinoembryonic antigen and sialyl-Tn antigen
levels were within the normal ranges.
Based on the diagnosis of advanced endometrial
adenocarcinoma of the corpus uteri, an abdominal total hysterectomy
was performed with bilateral salpingo-oophorectomy and left
supraclavicular lymph node biopsy. Intra-abdominal dissemination
was observed and intraoperative peritoneal cytology was positive.
The uterine cervix was extremely fragile and was damaged during the
hysterectomy; therefore, the affected tissue was resected as much
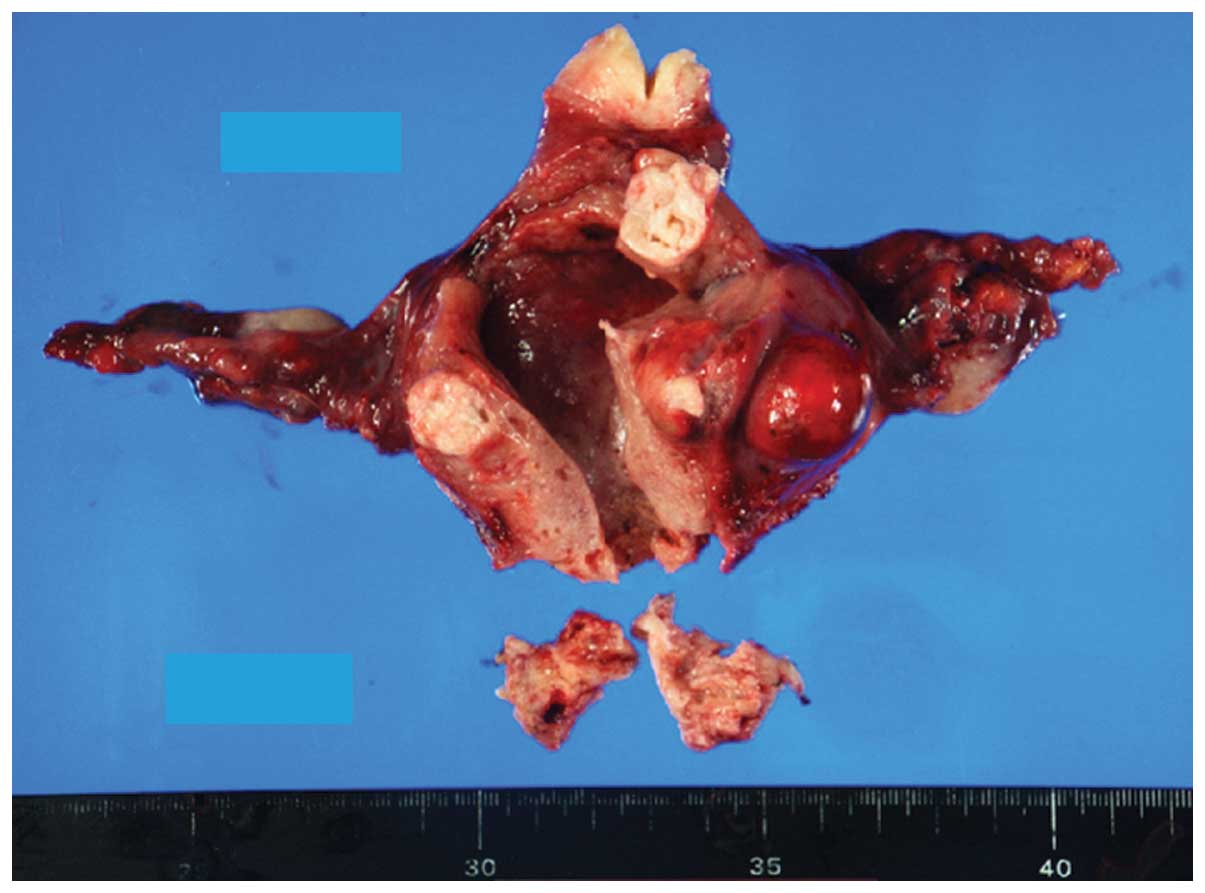
as possible. However, further tumors remained. Macroscopically, the
uterine corpus was enlarged to goose-egg size and the tumor was
located in the uterine cervix and uterine corpus. The tumor was
predominantly present in the uterine cervix. The endometrial
surface was moderately irregular (Fig.
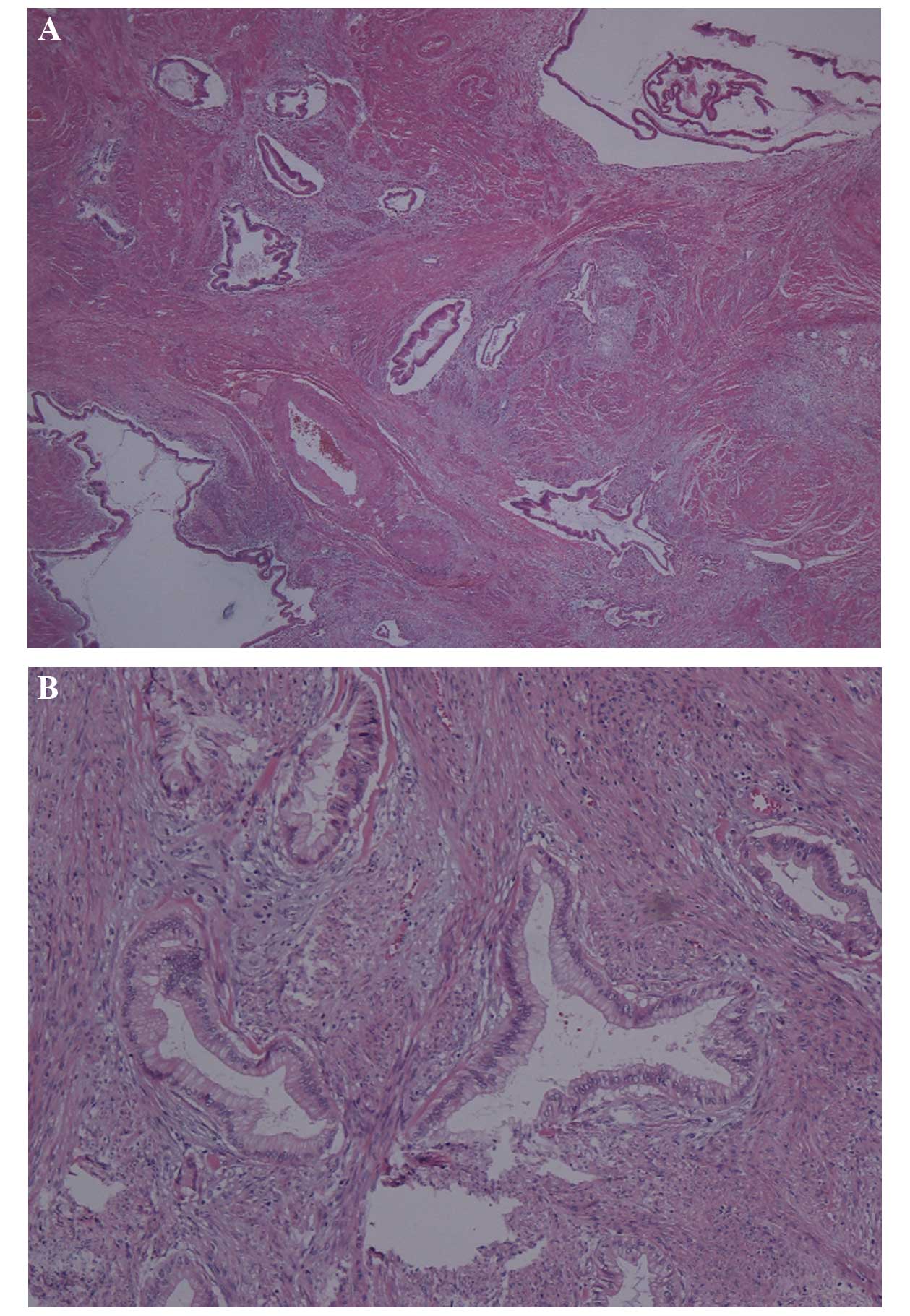
3) and microscopically, deeply infiltrating mucinous
adenocarcinoma, composed of well-formed glands arranged in an
irregular fashion, was identified. The nuclear and architectural
abnormalities were generally minimal; however, limited areas
exhibited a desmoplastic stromal reaction, indicating a malignant
nature (Fig. 4). A final diagnosis
of MDA of the uterine cervix was determined. Extension of tumors to
the uterine corpus, fallopian tubes and ovaries was identified and
the left supraclavicular lymph node was positive for metastasis.
The tumor was designated as pT4NXM1, according to the Union for
International Cancer Control TNM classification (7th edition)
(3).
In total, six courses of chemotherapy containing
irinotecan and cisplatin were administered postoperatively;
however, the growth of the remaining tumor tissue continued despite
the chemotherapy. The chemotherapy regimen was altered to
paclitaxel and carboplatin. Following one course, the remaining
tumor increased further, causing obstruction to the bilateral
ureters and leading to bilateral hydronephrosis. A double-J
catheter was inserted into the right ureter and this was followed
by supportive care. The patient is currently alive with the disease
at 10 months following the surgery.
Discussion
Adenoma malignum of the uterine cervix was initially
described by Gusserow in 1870 (4)
and, in 1963, McKelvey and Goodlin reported five cases of adenoma
malignum (5). In 1975, the name MDA
was proposed by Silverberg and Hurt (6) to more accurately reflect the
resemblance of the glands to the normal endocervical glands and the
lack of malignant cellular features. MDA is a rare subtype of
mucinous adenocarcinoma of the uterine cervix, accounting for only
1–3% of uterine cervical adenocarcinoma and 0.15–0.45% of all
cervical carcinomas of the uterus reported in the literature
(1). The major clinical
manifestations of MDA are profuse or mucoid discharge and irregular
vaginal bleeding (7).
The diagnostic methods of MDA are cytological
evaluations, biopsies, cross-sectional imaging and immunostaining.
MDA appears in MRI as a multicystic mass, demonstrating extremely
high-signal intensity on T2-weighted images and isointensity or
moderate hyperintensity on T1-weighted images, which extends from
the endocervical glands to the deep cervical stroma, with solid
portions located deep in the endocervix (8,9). MDA
is difficult to diagnose as few findings conclusively suggest
malignancy on cytological or histological examination. MDA lesions
are located deep in the endocervix and exhibit an endophytic growth
pattern, which also makes it difficult to determine an accurate
cytological and histological diagnosis (10). Li et al (7) reported that the detection rate of MDA
by cytological evaluation was only 32.7%. Granter and Lee (11) reported that enlarged glandular cells
in honeycombed sheets with abundant cytoplasm in exfoliative
cytology were crucial in the detection of MDA; however, a
preoperative histological diagnosis of MDA is also often difficult
to determine. Preoperative punch biopsy occasionally fails to
confirm the diagnosis of MDA as the tumor glands positioned in the
deep cervical stroma require a deep biopsy (i.e. cervical
conization) to confirm the presence of invasion. The monoclonal
antibody HIK-1083, which detects mucin produced and secreted by the
gastric mucous cells, has been indicated to be useful in the
correct diagnosis of MDA (12).
However, endocervical glandular hyperplasia with pyloric gland
metaplasia has also been observed to be positive for HIK-1083
(13). Li et al (7) reported that the detection rate of MDA
following a single biopsy was 28.7% and the rate of the total
number of biopsies including cervical conization was 50.7%.
Treatment and prognosis of MDA are controversial. Surgical
treatment is the most successful option; however, no standard
surgical treatment or adjuvant therapy have been established. The
treatment of MDA frequently shadows that of endocervical
adenocarcinoma and despite the presence of well-differentiated
histopathological features, the prognosis of MDA is poor. This is
due to the likelihood of the tumor to exhibit lymph node
involvement and the early presence of peritoneal carcinomatosis, in
contrast to the behavior of classical adenocarcinoma (5). However, a number of studies have
reported a favorable prognosis (7,14) and
stated that a poor prognosis of MDA is not always observed if it is
identified at an early stage. The present case exhibited peritoneal
carcinomatosis and distant metastasis to the left supraclavicular
lymph node at diagnosis; therefore, optimal surgery could not be
performed and the two types of adjuvant chemotherapy were
ineffective.
McGowan et al (2) reported that Peutz-Jeghers syndrome may
complicate MDA (2), and Gilks et
al (15) reported that
approximately half of all MDAs are complicated with ovarian
mucinous tumors. The present case, however, was not complicated
with these diseases.
The current study describes a rare case of MDA that
was difficult to differentiate from endometrial adenocarcinoma of
the corpus uteri preoperatively; following the diagnosis of
endometrial cancer, surgery was performed. The tumor was diagnosed
as MDA of the uterine cervix following pathological examination of
the hysterectomy specimen. In cases where mild thickening of the
endometrium is observed and the endometrial biopsy results indicate
a well-differentiated adenocarcinoma, with cystic lesions in the
uterine corpus and uterine cervix, the possibility of the invasion
of MDA of the uterine cervix to the uterine corpus must be
considered.
References
|
1
|
Kaminski PF and Norris HJ: Minimal
deviation carcinoma (adenoma malignum) of the cervix. Int J Gynecol
Pathol. 2:141–152. 1983.
|
|
2
|
McGowan L, Young RH and Scully RE:
Peutz-Jeghers syndrome with ‘adenoma malignum’ of the cervix. A
report of two cases. Gynecol Oncol. 10:125–133. 1980.
|
|
3
|
Sobin LH, Gospodarowicz MK and Wittekind
C: TNM Classification of Malignant Tumours. 7th edition.
Wiley-Blackwell; Hoboken, NJ: 2009
|
|
4
|
Gusserow ALS: Ueber sarcome des uterus.
Arch Gynakol. 1:240–251. 1870.
|
|
5
|
McKelvey JL and Goodlin RR: Adenoma
malignum of the cervix. A cancer of deceptively innocent
histological pattern. Cancer. 16:549–557. 1963.
|
|
6
|
Silverberg SG and Hurt WG: Minimal
deviation adenocarcinoma (‘adenoma malignum’) of the cervix: a
reappraisal. Am J Obstet Gynecol. 121:971–975. 1975.
|
|
7
|
Li G, Jiang W, Gui S and Xu C: Minimal
deviation adenocarcinoma of the uterine cervix. Int J Gynaecol
Obstet. 110:89–92. 2010.
|
|
8
|
Doi T, Yamashita Y, Yasunaga T, et al:
Adenoma malignum: MR imaging and pathologic study. Radiology.
204:39–42. 1997.
|
|
9
|
Yamashita Y, Takahashi M, Katabuchi H,
Fukumatsu Y, Miyazaki K and Okamura H: Adenoma malignum: MR
appearances mimicking nabothian cysts. Am J Roentgenol.
162:649–650. 1994.
|
|
10
|
Ishii K, Katsuyama T, Ota H, et al:
Cytologic and cytochemical features of adenoma malignum of the
uterine cervix. Cancer. 87:245–253. 1999.
|
|
11
|
Granter SR and Lee KR: Cytologic findings
in minimal deviation adenocarcinoma (adenoma malignum) of the
cervix. A report of seven cases. Am J Clin Pathol. 105:327–333.
1996.
|
|
12
|
Utsugi K, Hirai Y, Takeshima N, Akiyama F,
Sakurai S and Hasumi K: Utility of the monoclonal antibody HIK1083
in the diagnosis of adenoma malignum of the uterine cervix. Gynecol
Oncol. 75:345–348. 1999.
|
|
13
|
Yoden E, Mikami Y, Fujiwara K, Kohno I and
Imajo Y: Florid endocervical glandular hyperplasia with pyloric
gland metaplasia: a radiologic pitfall. J Comput Assist Tomogr.
25:94–97. 2001.
|
|
14
|
Hirai Y, Takeshima N, Haga A, Arai Y,
Akiyama F and Hasumi K: A clinicocytopathologic study of adenoma
malignum of the uterine cervix. Gynecol Oncol. 70:219–223.
1998.
|
|
15
|
Gilks CB, Young RH, Aguirre P, DeLellis RA
and Scully RE: Adenoma malignum (minimal deviation adenocarcinoma)
of the uterine cervix. A clinicopathological and
immunohistochemical analysis of 26 cases. Am J Surg Pathol.
13:717–729. 1989.
|