Introduction
Hepatocellular carcinoma (HCC) is the sixth most
common type of cancer and third most common cause of cancer-related
mortality worldwide. A total of ~50,000 new cases are estimated to
occur annually (1). With an
advanced diagnosis and effective early treatment via curative
resection, ablation or transplantation, the median survival time of
patients is >5 years (2). HCC is
strongly associated with chronic hepatitis B virus (HBV) infection;
just over half of HCC patients worldwide are HBV-infected and the
proportion is much higher in Asia (1). A total of 80% of HCC patients from
Asia and South Africa present with risk factors including HBV and
aflatoxin B1 exposure (2).
Furthermore, a substantial proportion of HCC patients (range,
14–37%) develop extrahepatic HCC metastasis (3). Such metastasis most commonly occurs in
adjacent lymph nodes and the lungs, and less frequently in the
bones, adrenal glands and brain (4). Surgical resection is a safe and
effective strategy for the treatment of numerous patients with
primary or metastatic HCC, however, recurrence is common, with ≤70%
of patients exhibiting tumor recurrence within five years of
curative surgery (5). The present
study describes an unusual case of a patient with chronic HBV
infection and HCC who, five months following surgical resection,
presented with a retrobulbar and intracranial lesion. Although the
lesion mimicked meningioma, subsequent pathological analysis
identified it as HCC metastasis. Additionally, the patient did not
show any evidence of tumor recurrence in the liver. Written
informed consent for the publication of this study was obtained
from the patient.
Case report
A 43 year-old male was admitted to the Neurosurgery
Department of the First Affiliated Hospital of Guangxi Medical
University (Nanning, China) on the 8 April, 2014 with approximately
a one-month history of mild headache and mild protopsis of the left
eye. Upon physical examination, the patient exhibited mild
protopsis of the left eye and ipsilateral visual acuity of 0.3
(normal range, 1.0–2.0) and contralateral visual acuity of 1.5
(normal range, 1.0–2.0). A frontal mass under the scalp adjacent to
the left orbit was visible, however, no pulsation or other positive
clinical manifestations were observed on palpation. Furthermore,
the patient reported no abnormal sensations around the left
eyeball, vomiting or vertigo.
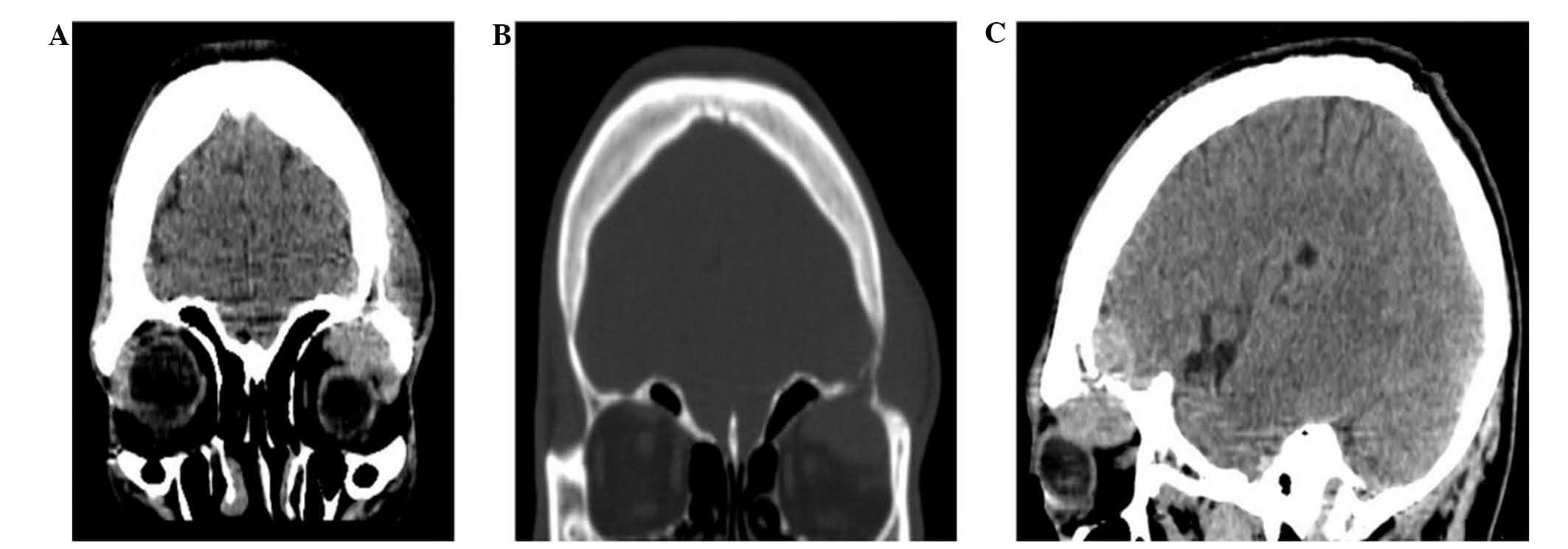
Computed tomography (CT) and cerebral magnetic
resonance imaging (MRI) scans identified retrobulbar metastasis and
intracranial invasion with lytic changes in the left orbital and
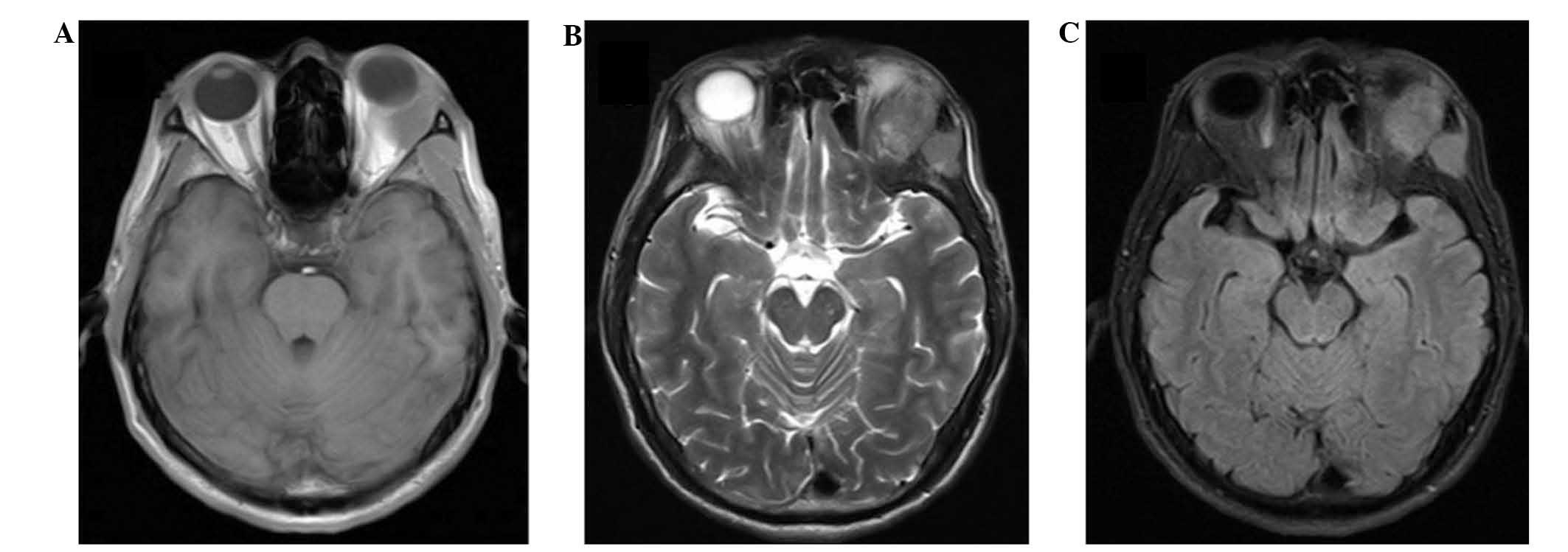
temporal bones (Fig. 1). Almost
homogeneous isointensity was visible on T1- and T2-weighted images,
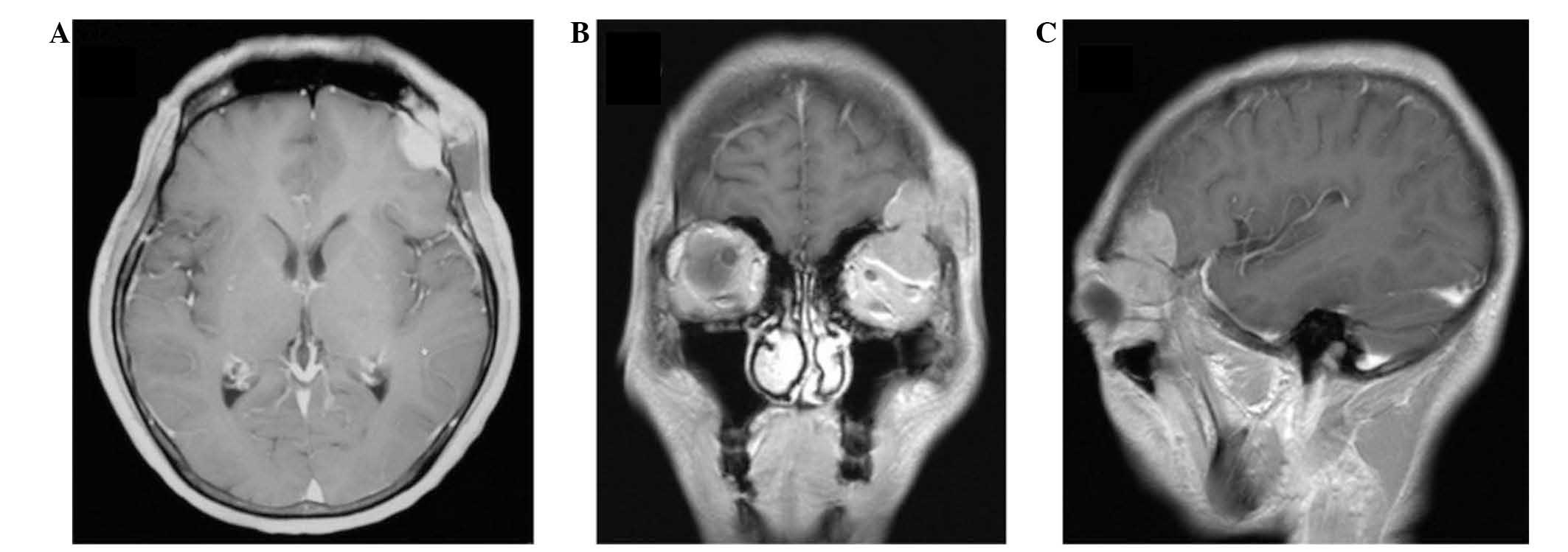
as well as on fluid-attenuated inversion recovery images (Fig. 2). Additionally, a dural tail sign
with lytic changes in the adjacent skull bones was present on
T1-enhanced MRI images (Fig. 3).
Therefore, a diagnosis of meningioma with retrobulbar and
under-scalp invasion was determined.
An enhanced CT scan of the upper abdomen revealed no
recurrent hepatic lesions (Fig. 4),
however, serological analysis demonstrated that the patient was
positive for hepatitis B (HB) surface antibody (Ab), HB e Ab and HB
core Ab. Additionally, the patient exhibited an α-fetoprotein level
of 29.07 ng/ml (normal range, 0–11 ng/ml), however, no
abnormalities were detected in the liver biochemistry or in other
routine tests.
Due to these findings, the intracranial mass was
surgically resected. Following scalp incision, a round mass with
the appearance of fish meat and a diameter of 5 cm was identified
to have invaded the local skull area. It was tightly adhered to the
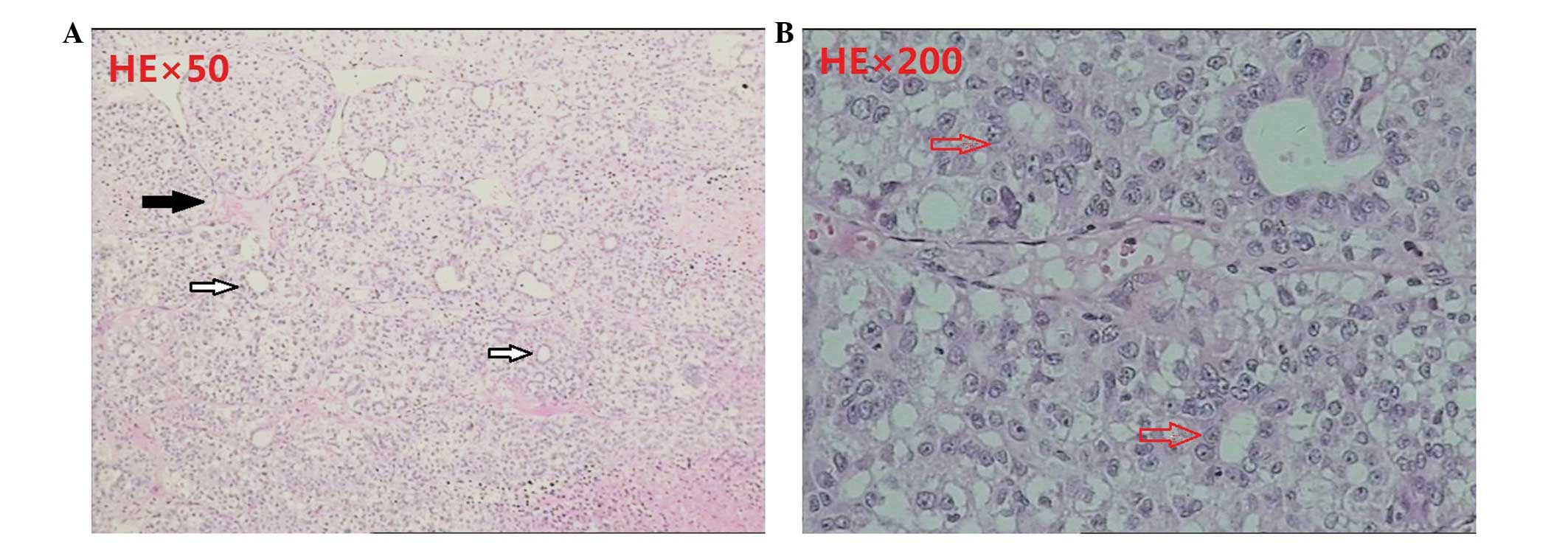
dura mater and protruded into the left orbit. Pathological
examination of the lesion following hematoxylin and eosin staining
was used to identify the mass as HCC (Fig. 5). Therefore, the patient was
definitively diagnosed with retrobulbar metastasis and intracranial
invasion from postoperative hepatocellular carcinoma (HCC).
Discussion
The combination of MRI imaging results and the
absence of detectable HCC lesions on the liver by enhanced CT of
the upper abdomen resulted in an initial misdiagnosis of meningioma
with retrobulbar invasion. Meningiomas are the second most common
type of primary brain tumor, accounting for 15–20% of primary brain
tumors; the intracranial mass protrudes extracranially via the
bones and mimics thickened bone (6). Ultimately, surgical findings and
postoperative pathology revealed the mass in the present patient to
be a HCC metastatic lesion.
The current study conducted a review of the relevant
Chinese- and English-language medical literature, and identified 39
cases of HCC metastasis to the head reported since 2009 (Table I) (4,7–35). Of
these 39 patients, 11 exhibited peri-orbital metastasis similar to
that of the present patient (Table
II) (4,17–19,25,30).
Of the 11 cases with HCC metastasis to the orbit published since
2009, all were male (with the exception of no gender being reported
in one case)e, five exhibited invasion from the right side, only
two patients demonstrated peri-orbital invasion combined with
cerebral invasion, yet cerebral invasion also occurred in the
present case. Painful proptosis was commo; seven patients suffered
from this, as well as the patient in the present case. Two patients
had not been diagnosed with HCC with metastasis when they were
hospitalized. The metastatic mass invaded the cerebrum in only two
cases and two patients experienced metastasis to the head five
years following liver transplantation to treat HCC (28,33).
The first case was a 70-year-old male, who had HCC and underwent
liver transplantation in August 2006, and was without HCC
recurrence in the following 4 years. However, the patient was
identified to have a 3-cm painless, subcutaneous mass; CT scans
showed an osteolytic lesion in the frontal bone without dural
matter invasion, which was pathologically diagnosed as HCC
metastasis. The second case was a 38-year-old male, who underwent
surgery to remove a liver mass and received a liver transplantation
4 months previously; however, a well-defined localized painless
mass was identified on the right temporal side of the patient’s
scalp. MRI showed that the mass involved the outer and inner skull
tables, and was attached to the dura matter. Pathological analysis
led to a diagnosis of HCC metastasis.
 | Table ILocation of hepatocellular carcinoma
metastases to the head reported in the Chinese- and
English-language literature since 2009. |
Table I
Location of hepatocellular carcinoma
metastases to the head reported in the Chinese- and
English-language literature since 2009.
| Lesion location | n (%) |
|---|
| Orbit | 11 (28.2) |
| Face | 8 (20.5) |
| Skull base | 5 (12.8) |
| Scalp | 4 (10.3) |
| Meninges | 4 (10.3) |
| Calvaria | 3 (7.7) |
| Cerebrum | 2 (5.1) |
| Dura and scalp | 2 (5.1) |
| Total | 39 (100) |
 | Table IIClinical characteristics of patients
with HCC metastasis to the orbit published since 2009. |
Table II
Clinical characteristics of patients
with HCC metastasis to the orbit published since 2009.
| Study Author,
year | Gender/Age,
years | Side | Cerebrum
invasion | Other metastasis | Clinical
presentation | Risk factor for
metastasis |
|---|
| Quick et al,
2009 | M/52.0 | R | No | No | Proptosis and
diplopia | No |
| Kolarevic et
al, 2011 | M/70.0 | R | No | Spleen, maxillary,
retroperitoneal lymph node | Bleeding difficult to
control after dental surgery | No |
| Mustapha et
al, 2011 | M/25.0 | R | No | No | Progressive pain,
swelling and blurred vision for 1 month | NR |
| Guerriero et
al, 2011 | M/45.0 | L | Yes | Lung | Proptosis for 1
month | HCC liver transplant
5 years previously |
| Piccirillo et
al, 2013 | NA | L | No | Lung | NR | HCC liver transplant
3 years previously |
| Eldesouky et
al, 2013 | M/62.0 | L | No | No | Painful proptosis for
8 weeks | HCC for 1.5
years |
| M/70.0 | L | No | No | Painful proptosis for
6 weeks | HCV for 10 years |
| M/55.0 | R | No | No | Proptosis for 4
weeks | HCC for 1 year |
| M/65.0 | L | No | No | Painful proptosis for
2 weeks | HCV for 12 years |
| M/47.0 | L | No | No | Painful proptosis for
6 weeks | HCV for 15 years |
| M/62.0 | R | Yes | No | Eyelid ptosis for 8
weeks | HCC for 14
months |
| Present study | M/43.5 | L | Yes | No | Mild headache and
mild protopsis for 4 weeks | HCC for 5 months |
The present study illustrates that extrahepatic
metastasis can occur with or without concurrent intrahepatic
lesions following curative resection for HCC. Surgery is widely
considered to be an effective treatment strategy for extrahepatic
metastatic lesions from HCC; however, systemic sorafenib therapy
may be another possible treatment modality, as it has demonstrated
improved survival in HCC metastatic patients (36).
In conclusion, the present study highlights the
importance of considering metastasis in the differential diagnosis
of patients with a history of HCC who present with an intracranial
mass. The possibility of HCC metastasis must be acknowledged
despite the results of imaging procedures and other clinical
indicators, as brain metastases may closely mimic meningioma.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant no. 81160168).
References
|
1
|
Montalto G, Cervello M, Giannitrapani L,
Dantona F, Terranova A and Castagnetta LA: Epidemiology, risk
factors, and natural history of hepatocellular carcinoma. Ann N Y
Acad Sci. 963:13–20. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Forner A, Llovet JM and Bruix J:
Hepatocellular carcinoma. Lancet. 379:1245–1255. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Katyal S, Oliver JH III, Peterson MS,
Ferris JV, Carr BS and Baron RL: Extrahepatic metastases of
hepatocellular carcinoma. Radiology. 216:698–703. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Quick AM, Bloomston M, Kim EY, Hall NC and
Mayr NA: Complete response to radiation therapy of orbital
metastasis from hepatocellular carcinoma. World J Gastroenterol.
15:6000–6003. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
European Association for the Study of the
Liver; European Organization for Research and Treatment of Cancer.
EASL-EORTC clinical practice guidelines: management of
hepatocellular carcinoma. J Hepatol. 56:908–943. 2012.PubMed/NCBI
|
|
6
|
Jang SY, Kim CH, Cheong JH and Kim JM:
Extracranial extension of intracranial atypical meningioma en
plaque with osteoblastic change of the skull. J Korean Neurosurg
Soc. 55:205–207. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tateno H, Hoshino T, Takahashi K,
Matsumura M, Sakaida N and Ohe C: A rapidly progressed metastatic
choroidal tumor from a hepatocellular carcinoma. Nihon Ganka Gakkai
Zasshi. 113:107–111. 2009.(In Japanese). PubMed/NCBI
|
|
8
|
Trivedi P, Gupta A, Pasricha S, Agrawal G
and Shah M: Isolated skull base metastasis as the first
manifestation of hepatocellular carcinoma - a rare case report with
review of literature. J Gastrointest Cancer. 40:10–14. 2009.
View Article : Google Scholar
|
|
9
|
Pallini R, Sabatino G, Doglietto F,
Lauretti L, Fernandez E and Maira G: Clivus metastases: report of
seven patients and literature review. Acta Neurochir (Wien).
151:291–296. 2009. View Article : Google Scholar
|
|
10
|
Somerset H, Witt JP and
Kleinschmidt-Demasters BK: Hepatocellular carcinoma metastases to
the epidural space. Arch Pathol Lab Med. 133:1975–1980.
2009.PubMed/NCBI
|
|
11
|
Ma XH: Hepatocellular carcinoma metastasis
to brain: A case report. Chinese Hepatology. 14:3362009.
|
|
12
|
Vitale AR, Compilato D, Coletti G, et al:
Metastatic hepatocellular carcinoma of the parotid region without
lung metastasis: a case report. Int J Oral Maxillofac Surg.
38:696–698. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim BG, Yoon SM, Bae HG and Yun IG:
Spontaneous intracranial epidural hematoma originating from dural
metastasis of hepatocellular carcinoma. J Korean Neurosurg Soc.
48:166–169. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Woo KM, Kim BC, Cho KT and Kim EJ:
Spontaneous epidural hematoma from skull base metastasis of
hepatocellular carcinoma. J Korean Neurosurg Soc. 47:461–463. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bair MJ, Lei WY and Chen CL: Electronic
images of the month. An unusual presentation of hematemesis: a
presentation of maxillary metastasis from hepatocellular carcinoma.
Clin Gastroenterol Hepatol. 8:e61–e62. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Saneluxsana S and Urathamakul S: Recurrent
skull metastasis of hepatocellular carcinoma at 2 month post
operation. J Med Assoc Thai. 93(Suppl 6): S212–S214. 2010.
|
|
17
|
Kolarević D, Tomasević Z, Boricić I, et
al: Metastasis of hepatocellular carcinoma presented as a tumor of
the maxillary sinus and retrobulbar tumor. Vojnosanit Pregl.
68:359–362. 2011. View Article : Google Scholar
|
|
18
|
Mustapha SK and Madachi DA: Orbital
metastasis of hepatocellular carcinoma: a case report. West Afr J
Med. 30:305–307. 2011.
|
|
19
|
Guerriero S, Infante G, Giancipoli E, et
al: Hepatocellular carcinoma metastasis to the orbit in a
coinfected HIV+ HBV+ patient previously treated with orthotopic
liver transplantation: A case report. Case Rep Ophthalmol Med.
2011:5492702011.PubMed/NCBI
|
|
20
|
Walter CM, Kirby EJ, Vasconez HC and
Rinker BD: Hepatocellular carcinoma metastatic to the scalp. J
Craniofac Surg. 22:720–721. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kato Y, Kikuchi N, Nishibu A, Ohtsuka M
and Yamamoto T: Letter: Two cases of metastases to the scalp bone
mimicking epidermoid cyst. Dermatol Online J. 17:132011.
|
|
22
|
Lasiter JC, Liess BD, Zitsch RP III and
Wieberg J: An expansile mandibular mass as the initial
manifestation of hepatocellular carcinoma. Ear Nose Throat J.
90:E192011.PubMed/NCBI
|
|
23
|
Yang JI, Kang JM, Byun HJ, et al:
Metastatic hepatocellular carcinoma presenting as facial nerve
palsy and facial pain. Korean J Hepatol. 17:319–322. 2011.
View Article : Google Scholar
|
|
24
|
Sanchez-Delgado J, Calzado S, de Haro C,
et al: Long survival after resection of cranial metastases from
hepatocellular carcinoma. Case report and review of the literature.
Gastroenterol Hepatol. 35:12–16. 2012.(In Spanish).
|
|
25
|
Eldesouky MA, Elbakary MA, Shalaby OE and
Shareef MM: Orbital metastasis from hepatocellular carcinoma:
report of 6 cases. Ophthal Plast Reconstr Surg. 30:e78–e82. 2014.
View Article : Google Scholar
|
|
26
|
Pirbhai A, Kahawita S, Davis G, Dodd T,
Thomas J and Selva D: Hepatocellular carcinoma metastasis to
sphenoid wing. Orbit. 32:132–133. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nemetz U, Tomazic PV, Walch C, et al:
Pyramidal apex metastasis as primary manifestation of
hepatocellular carcinoma. Otol Neurotol. 34:e30–e31. 2013.
View Article : Google Scholar
|
|
28
|
Turan I, Yapali S, Ozutemiz O and Karasu
Z: Frontal skull metastasis extending through the scalp: initial
sign of hepatocellular carcinoma recurrence 5 years after liver
transplantation. Transplantation. 95:e15–e16. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Miller ME, McCall AA, Juillard GF,
Nadelman CM, Wang MB and Nabili V: Hepatocellular carcinoma
metastatic to the mandible. Ear Nose Throat J. 92:E17–E19.
2013.PubMed/NCBI
|
|
30
|
Piccirillo M, Granata V, Albino V, et al:
Can hepatocellular carcinoma (HCC) produce unconventional
metastases? Four cases of extrahepatic HCC. Tumori. 99:e19–e23.
2013.PubMed/NCBI
|
|
31
|
Tomanovic N, Krstic A, Brasanac D,
Dimitrijevic M, Terzic T and Boricic I: Zygomatic bone metastasis
as an initial presentation of hepatocellular carcinoma. Arch Iran
Med. 16:675–678. 2013.PubMed/NCBI
|
|
32
|
Brunetti AE, Popescu O and Silvestris N:
Synchronous mandibular and giant parieto-occipital skull metastasis
from hepatocellular carcinoma. Clin Gastroenterol Hepatol.
11:xxvi2013. View Article : Google Scholar
|
|
33
|
Azarpira N, Dehghanian A, Safarian A and
Kazemi K: Case report of skull metastasis from hepatocellular
carcinoma after a liver transplant. Exp Clin Transplant.
12:265–268. 2014.
|
|
34
|
Pan Z, Yang G, Yuan T, et al:
Leptomeningeal metastasis from hepatocellular carcinoma with other
unusual metastases: a case report. BMC Cancer. 14:3992014.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Guo X, Yin J and Jiang Y: Solitary skull
metastasis as the first symptom of hepatocellular carcinoma: case
report and literature review. Neuropsychiatr Dis Treat. 10:681–686.
2014.PubMed/NCBI
|
|
36
|
Chua TC and Morris DL: Exploring the role
of resection of extrahepatic metastases from hepatocellular
carcinoma. Surg Oncol. 21:95–101. 2012. View Article : Google Scholar
|