Introduction
Myofibroblasts, initially identified in granulation
tissue in 1971 (1), have been
revealed as the principal cell type in certain neoplastic
soft-tissue lesions, and occasionally in the stroma of normal
tissues (2,3). Myofibroblasts have also been revealed
to be associated with inflammatory or fibrosing non-neoplastic
conditions (2,3). In adults, myofibroblasts are known to
exist in the periodontal ligaments and around the testicular
seminiferous tubules (4). The cells
are believed to originate from proximal resident mesenchymal cells,
in particular fibroblasts, and less frequently from smooth muscle
cells, pericytes and endothelial cells (5–7). In a
previous study, Gabbiani (8)
concluded that the transition from fibroblast to myofibroblast
resulted from the combined effect of mechanical tension,
transforming growth factor-β and extra domain-A of cellular
fibronectin (8). However,
alternative mechanisms to explain the cellular origin of
myofibroblasts have also been proposed; these include the
recruitment from bone marrow-derived circulating fibrocytes and the
occurrence of epithelial-mesenchymal transformation (9). Evidence to suggest that myofibroblasts
can differentiate into smooth muscle cells is yet to be published,
and those cells present during wound healing are believed to
apoptose following the completion of epithelialization (8,10).
Myofibroblasts are spindle-shaped, bipolar or
stellate cells with elongated, tapered, indented or wavy nuclei.
The cells may also appear as short, oval and pale-staining cells
with distinct and punctate, small, central nucleoli (11). The cytoplasm is usually light
eosinophilic or occasionally amphophilic, moderate to minimal in
amount and with indistinct cellular margins. Ultrastructurally, the
cytoplasm is comprised of abundant rough endoplasmic reticulum, and
subplasmalemmal or peripheral bundles of thin cytoplasmic filaments
with dense foci. These bundles pass through the cell membrane to
form the cell-to-matrix junction with extracellular fibronectin
fibrils, a structure known as the fibronexus (12). The fibronexus is observed in cells
of reactive, and other forms, of myofibroblastic lesions, but is
usually absent in smooth-muscle cells and fibroblasts (13). In contrast to myofibroblasts,
myofilaments are distributed throughout the cytoplasm in smooth
muscle cells, are accompanied by cell membrane vesicles and
plaques, and are surrounded by the external lamina (12).
Low-grade myofibroblastic sarcomas (LGMSs) have been
reported in the literature under various terms, including
myofibrosarcomas, sarcomas of myofibroblasts, myofibroblast-rich
fibrosarcomas, leiomyosarcoma myofibroblastic variant and
spindle-cell sarcomas showing myofibroblastic differentiation
(14). Following the establishment
of a diagnostic criteria by Mentzel et al (15) in 1998, LGMS was reclassified as a
distinct entity by the World Health Organization classification of
soft-tissue tumors (16). LGMSs are
primarily composed of spindle-shaped or stellate cells arranged in
fascicles of varying length, with or without focal herringbone or
storiform whorls (11,12). Tumor cells consist of small to
moderate amounts of ill-defined, palely eosinophilic cytoplasm and
fusiform nuclei, which may be tapering and wavy, or round and
vesicular with indentations and small, indistinct nucleoli. Focal
nuclear atypia is observed in the majority of cases, but is usually
mild with dispersed, enlarged hyperchromatic nuclei. However,
larger atypical cells are occasionally detected (11,12).
The mitotic activity of the tumor cells varies, but abnormal
mitotic figures are typically absent. Necrosis is rare, and is
usually a feature associated with high-grade malignancies. The
stroma may be variably collagenous or focally myxoid, and contain
small numbers of lymphocytes, or on rare occasions, osteoclast-like
giant cells. In addition, polygonal cells are occasionally observed
in cellular areas (11,12).
LGMS has been reported at a variety of sites,
including the extremities (17,18),
trunk (19,20) and abdominal and pelvic cavities
(21,22). However, the malignancy is usually
associated with the head and neck, particularly the tongue
(15). The present study
investigated two rare cases of maxillary LGMS, one of which was
misdiagnosed as an inflammatory myofibroblastic tumor (IMT) during
a pre-operative excision biopsy, and presented with a different
immunophenotype upon recurrence. In addition, the
immunohistochemical analysis, differential diagnoses and literature
of LGMS are described. This study was approved by the ethics
commitee of (Jilin University Facilitated Oral Hospital, Changchun,
China) and written informed consent was obtained from all
patients.
Materials and methods
Tissues and reagents
The LGMS cases were retrieved from the routine
surgical files at the Department of Pathology, Jilin University
Facilitated Oral Hospital. Immunohistochemical analyses, using the
primary antibodies listed in Table
I, were performed upon 3-μm thick sections of
paraffin-embedded, formalin-fixed tissue selected from each case.
The monoclonal mouse anti-human primary antibodies against α-smooth
muscle actin (SMA; 1:50), muscle-specific actin (MSA; 1:50), desmin
(1:100), vimentin (1:100), h-caldesmon (1:50), cytokeratin (CK;
1:100), cluster of differentiation 34 (CD34; 1:100), anaplastic
lymphoma kinase (ALK; 1:50), epithelial membrane antigen (EMA;
1:100) and Ki-67 (1:100), polyclonal rabbit anti-human antibody
against fibronectin (1:100) and monoclonal rabbit anti-human
against calponin (1:50) and S-100 protein (1:100) were purchased
from Beijing ZhongShan Golden Bridge Biotechnology Co., Ltd.
(Beijing, China). The immunohistochemical analysis was performed
using the streptavidin-biotin-peroxidase complex method. Staining
was scored according to the following criteria: −, <5% cells
positive; +, 5–25% cells positive; ++, 25–75% cells positive; or
+++, >75% cells positive.
 | Table IImmunohistochemical antibodies and
results. |
Table I
Immunohistochemical antibodies and
results.
| | |
Immunoreactivity |
|---|
| | |
|
|---|
| Antibody | Clone | Pretreatment | Case 1 | Case 2 (primary
lesion) | Case 2 (recurrent
lesion) |
|---|
| Vimentin | V9 | None | + | + | + |
| Desmin | ZC18 | None | − | + | − |
| SMA | 1A4 | None | + | + | + |
| MSA | HHF35 | None | − | − | − |
| EMA | E29 | Pressure
cooker | − | − | − |
| CK | AE1/AE3 | Pressure
cooker | − | − | + |
| ALK | ALK-1 | Pressure
cooker | − | − | − |
| Ki-67, % | K-2 | Pressure
cooker | 24 (20–27) | 24.7 (20–27) | 41.9 (34–49) |
| S-100 | 4C4.9 | Pressure
cooker | − | − | − |
| CD34 | QBEnd/10 | Pressure
cooker | − | − | − |
| Calponin | EP63 | Pressure
cooker | − | − | − |
| h-caldesmon | h-CD | Pressure
cooker | − | − | − |
| Fibronectin | polyclone | Pressure
cooker | + | + | + |
Case report
Case 1
In March 2010, a 45-year-old male, who presented
with a painless, progressively enlarging swelling of the left
maxilla that had been apparent for six months, was admitted to the
Jilin University Facilitated Oral Hospital. The patient complained
of discomfort whilst chewing, and had a history of malignant
gingival fibroma on the left maxilla, which had been diagnosed and
treated with a subsequent local wide resection of the tumor three
years previously. The patient reported smoking a packet of
cigarettes every day for the last 20 years, and consuming 50 ml of
alcohol per day for the last 10 years. The results of all
laboratory tests upon admission were within normal limits, and no
clinical evidence of lymphadenopathy was apparent.
An oral examination revealed swelling of the left
maxilla, involving the buccal and palatal alveolar bones and the
palate, and spreading from the incisor (buccal side) and incisive
foramen (palatal side) to the distal aspect of the third molar. The
overlying mucosa exhibited no ulceration or hyperemia. All
adjacent, associated teeth demonstrated grade II mobility. A
computed tomography (CT) scan revealed a tumor mass measuring
5.2×4.5 cm within the left maxilla, which had invaded the left
maxillary sinus, the nasal cavity, the left hard palate and the
alveolar bone, with a relatively clear margin. A left maxillectomy
was performed without any subsequent therapy. Evidence of
recurrence or metastasis was not observed during the 30-month
follow-up period.
Case 2
In October 2012, a 29-year-old female was admitted
to the Jilin University Facilitated Oral Hospital following an
excision biopsy that had been performed and which had been
diagnosed as IMT. The patient presented with a progressively
enlarging swelling of the anterior portion of the maxilla,
accompanied with increased mobility of the upper incisors and pain
during occlusion. The patient reported smoking four cigarettes per
day for the last six years prior to admittance to the hospital. In
2000, the patient underwent an appendectomy, followed by a cesarean
section nine years later. The results of all laboratory tests upon
admission were within normal limits, and no clinical evidence of
lymphadenopathy was apparent.
An oral examination revealed a stable, painful
swelling in the anterior portion of the maxilla, involving the
buccal and palatal alveolar bones, and extending from the distal
aspect of the left maxillary incisor to the distal aspect of the
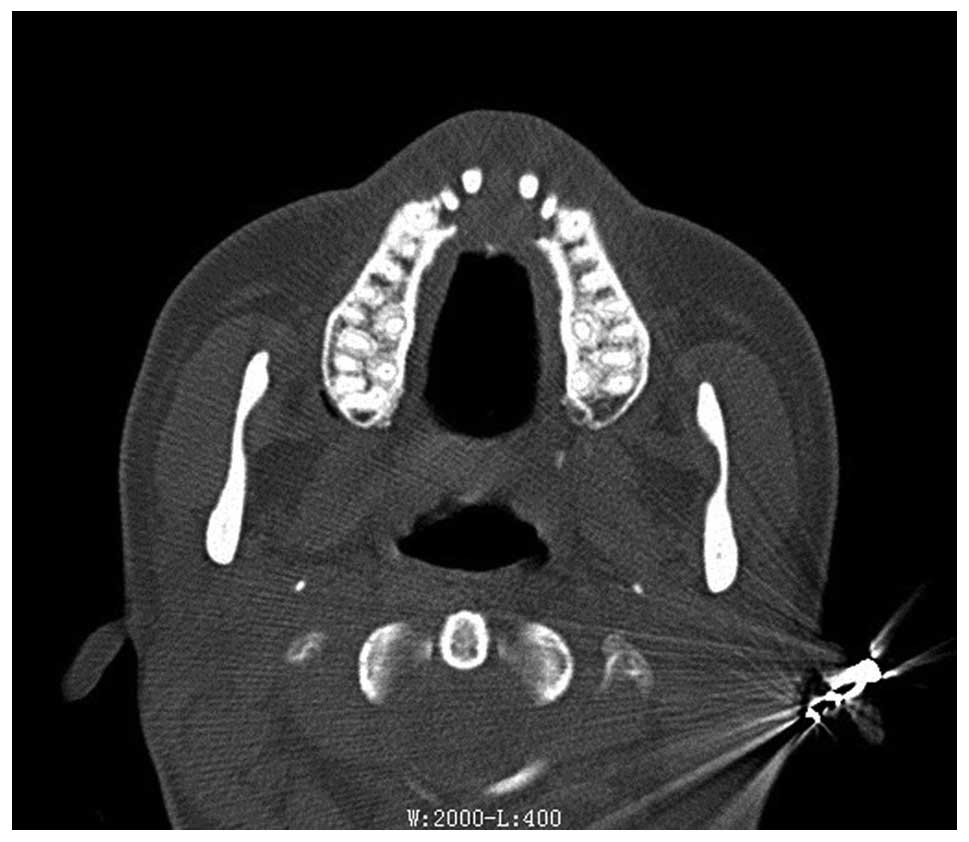
right maxillary incisor. The overlying mucosa was hyperemic. A CT
scan revealed a swelling ~2.5×2.0 cm in size, involving all
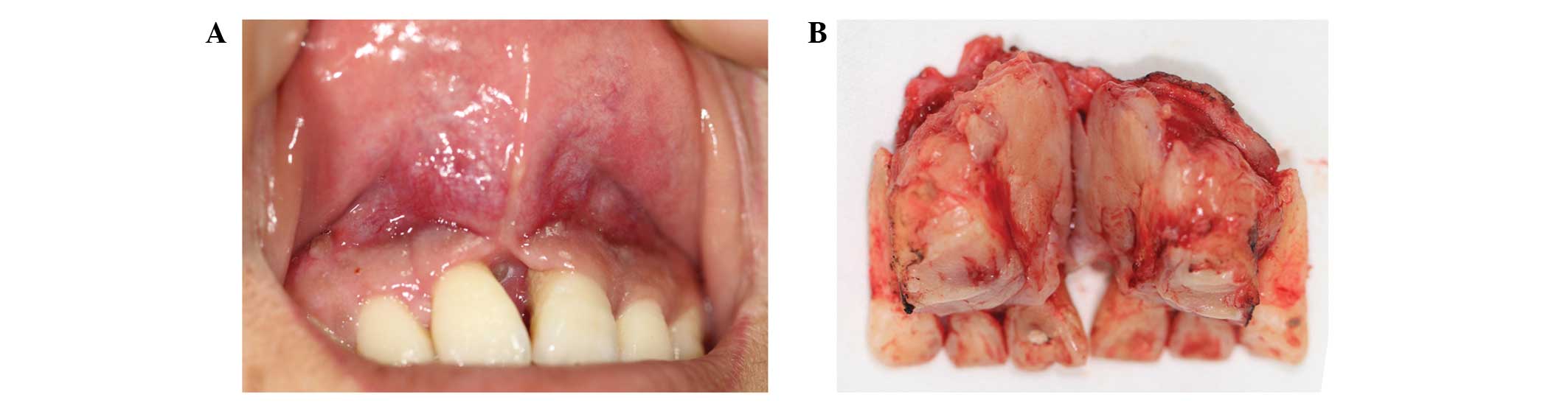
maxillary incisors (Fig. 1). A wide
local resection was performed from the distal aspect of one
maxillary canine to that of the other (Fig. 2), and the tumor-free margins were
histologically observed in the frozen sections obtained from the
biopsies. Ancillary therapy was not used, and a diagnosis of LGMS
was reached following surgery. However, six months later, the
neoplasm recurred, this time measuring 1.0×1.5 cm in size. A CT
scan revealed bone erosion on the buccal side of the first premolar
in the right maxilla. A local wide resection was therefore
performed, which included the removal of certain tumor-free
margins. Further evidence of recurrence or metastasis was not
observed at the 6-month follow-up.
Results
Case 1
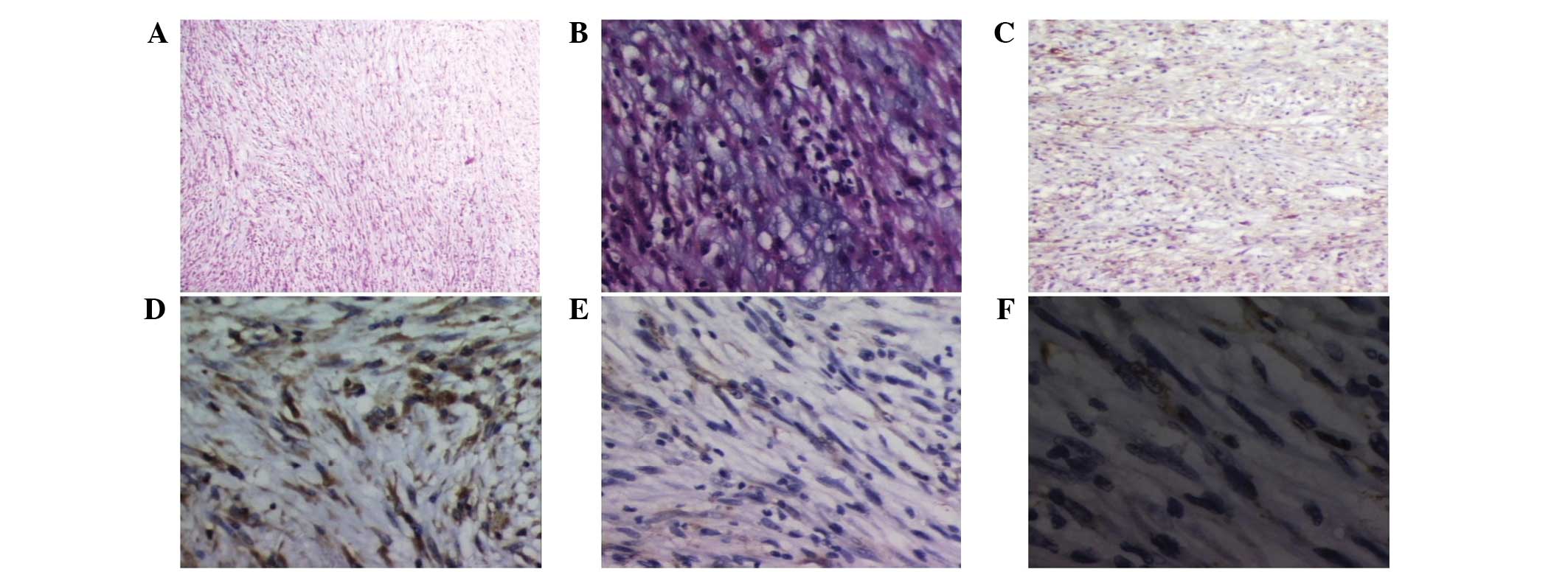
Microscopic examination revealed a tumor primarily
composed of spindle-shaped cells, with diffuse infiltrative growth
into the surrounding tissues (Fig.
3A). The neoplastic spindle cells were predominately arranged
in long fascicles, while herringbone and vague storiform patterns
were observed focally. The cytoplasm demonstrated a pale
eosinophilic appearance with ill-defined cellular margins. The
nuclei appeared to be either tapered and wavy, or slightly round
with myxoid degeneration of the stroma (Fig. 3B). Nuclear atypia was mild with
occasional nuclear hyperchromatism. Necrosis was not observed, and
the mitotic rate was relatively low at 1–2/high-power field (HPF),
with the absence of any abnormal patterns of mitosis. Inflammatory
components were unremarkable in amount. The immunohistochemical
analysis revealed that the spindle cells were positive for
fibronectin (FN) (+) (Fig. 3C),
vimentin (++) (Fig. 3D) and SMA (+)
(Fig. 3E and F), but negative for
S-100 (−).
Case 2
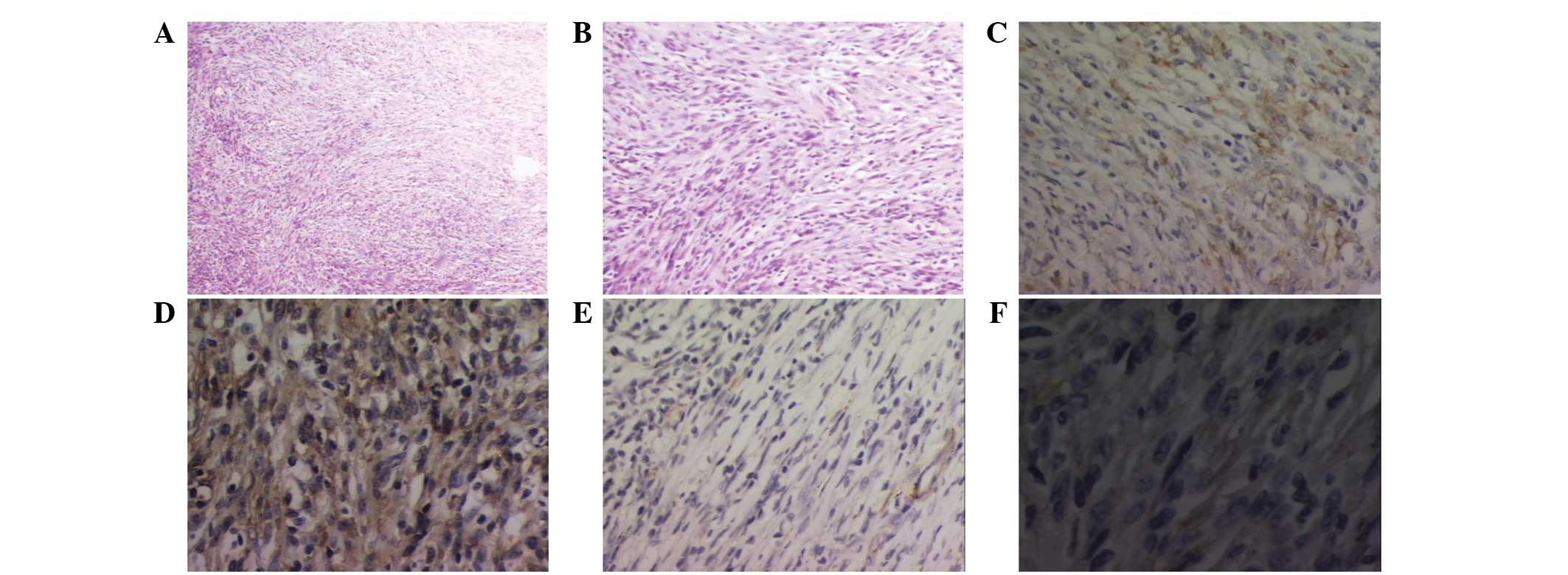
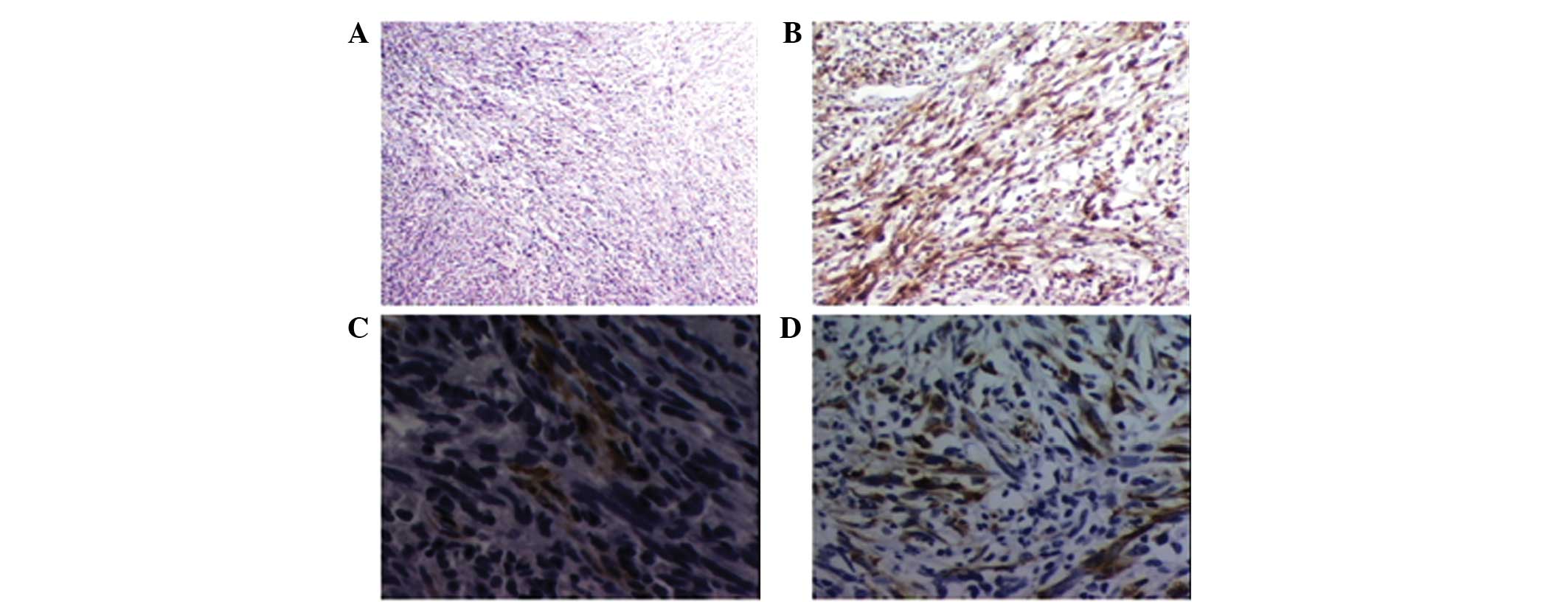
Histological examination revealed a tumor primarily
composed of spindle-shaped cells arranged in fascicles of varying
length, with intersecting and storiform patterns apparent focally
(Fig. 4A). The spindle cells had
ill-defined, palely eosinophilic cytoplasm, and the nuclei were
either thin and wavy or slightly round and vesicular. Nuclear
atypia was mild, while nuclear hyperchromatism was occasionally
observed. The mitotic rate was 1–2/HPF and abnormal mitotic
patterns were not observed. A diffuse inflammatory infiltration
(Fig. 4B), comprised of a large
number of lymphocytes and occasional plasma cells, was also
identified. The hypocellular portion of the stroma presented with
hyaline degeneration.
The immunochemical analysis revealed that the
spindle cells were positive for desmin (+) (Fig. 4C), vimentin (+++) (Fig. 4D), α-SMA (+) (Fig. 4E) and FN (Fig. 4F), and negative for S-100 protein
(−). The recurrent tumor demonstrated no further malignancy
(Fig. 5A), but presented with a
different immunophenotype, which was positive for FN (++) (Fig. 5B), SMA (+) (Fig. 5C) and CK (+) (Fig. 5D) and negative for desmin (−). The
diagnosis was consistent with the primary lesion. The primary
antibodies used in the present study, and the results of the
immunohistochemical analysis, are summarized in Table I.
Discussion
The term myofibrosarcoma, which defines a malignant
tumor of the myofibroblasts, was suggested by Ghadially (23) in 1980 as an analogy of the term
fibrosarcoma. According to current grading systems, myofibroblastic
sarcomas (myofibrosarcomas) can be classified into low-,
intermediate- and high-grade entities. Pleomorphic myofibroblastic
sarcoma is a high-grade subset of the malignant fibrous
histocytoma, and can be distinguished from the morphologically
similar low- and intermediate-grade myofibroblastic sarcomas. The
majority of LGMSs are deep soft-tissue lesions, but others may be
intraosseous or have originated from subcutaneous tissue or the
submucosa. The age range of patients with LGMS is 4–85 years (mean,
40 years), with a slightly higher proportion of males affected. The
tumors range in size between 1.5 and 17 cm (24). By contrast, myofibroblastic sarcomas
of the mammary gland differ clinically and biologically from those
affecting extra-mammary regions. The aggressive mammary
myofibroblastic sarcomas predominantly affect middle- to old-aged
patients (46 to 81 years), and are more frequently observed in
females (25). A study by Yamada
et al (26), reported a
38.2% recurrence rate among 38 cases of LGMS, which is one of the
highest values cited from nasal cavity/paranasal sinus LGMSs, the
second highest after cases of the jawbone, followed by the deep
tissue space. The recurrence rate for tumors of <3 cm in size is
21.4%, but for tumors >3 cm, the recurrence rate increases to
46.2% (26). In the aforementioned
study, the common sites affected by LGMS, after the tongue, are the
maxilla and palate, the mandible, the nasal/paranasal cavity and
the deep tissue spaces, including the parapharyngeal space.
Common factors associated with tumor recurrence are
believed to be tumor size, growth pattern and location, and the
surgical methods used during treatment. However, it is yet to be
demonstrated whether the immunophenotype of LGMS is a contributing
factor to recurrence. Myofibroblastic sarcomas, except for
pleomorphic types, are slow-growing, infiltrative tumors that are
susceptible to local recurrence, but rarely metastasize, even after
a number of years. A painless, enlarging mass is the most common
clinical finding, but tumor-related symptoms, such as hoarseness
(27) and dysphonia (28) in cases of the larynx, and
paresthesia (29,30), ulceration and non-allergic to
topical steroids (31), are also
reported. In addition, lung metastasis was observed in one case in
each of the large series reported by Mentzel et al (15) and Montgomery et al (32), and has also been identified in other
published studies (25,33,34).
Although LGMSs can be focally contained, the
majority infiltrate into the adjacent fibrous tissue, fat, skeletal
muscle or bone. Recurrent tumors tend to exhibit increased
pleomorphism, or display areas of higher grade malignancy (32,33),
but a pulmonary metastasis from an intermediate-grade
myofibrosarcoma that was unremarkable and fasciitis-like has also
been reported (32,33).
LGMSs display variable immunophenotypes, despite the
morphological homogeneity. In addition to being positive for
vimentin, these sarcomas may be positive for either SMA and/or
desmin (15,32,33),
resulting in desmin(+)/SMA(−), desmin(−)/SMA(+) and
desmin(+)/SMA(+) immunophenotypes. Reflecting the microanatomy of
myofibroblasts, SMA staining can be present as a peripheral rim
beneath the cell membrane. Calponin is diffusely positive in the
majority of cases, while h-caldemon is usually negative.
Myofibroblastic sarcomas can also display fibronectin (35), but not collagen IV or laminin. EMA
and S-100 protein staining is almost always negative, whereas
keratin(+) and CD34(+) cells have occasionally been reported
(15). Electron microscopy has
revealed that the tumor cells exhibit features of myofibroblasts,
but with variable numbers of fibronexuses that tend to be modestly
developed in comparison with those observed in granulation tissue
and tumor stroma (36,37). Cytogenetic analyses presented by
Mentzel et al (15) and Meng
et al (38) demonstrated
non-specific findings, such as those of infantile fibrosarcama and
inflammatory myofibroblastic sarcoma.
The tumor cells from the two cases in the present
study did not express calponin or MSA, a finding which is not in
accordance with the reported literature. Despite this, the other
results obtained from the present study are supportive of a
diagnosis of LGMS. The lesion from case 2, which was misdiagnosed
as an IMT following a pre-operative excision biopsy, presented with
a different immunophenotype upon recurrence. In contrast to the
primary lesion, tumor cells of the recurrent lesion were negative
for desmin and positive for CK. This is a rare finding that has not
been previously reported. On the basis of this transformation, the
present study concluded that cases of LGMS with immunoprofile
alterations are predictive of relatively poor prognoses,
particularly in terms of recurrence rate. As previously stated,
recurrent LGMS tends to exhibit increased pleomorphism and areas of
higher grade malignancy. Although the recurrent tumor in case 2 did
not exhibit such alterations, it is hypothesized that further
recurrent lesions would potentially present with increased
pleomorphism and aggressiveness. However, the evaluation and
follow-up of additional cases is required in order to understand
this phenomenon.
A wide local resection, including the removal of
tumor-free margins, is the primary treatment for LGMS. However,
ancillary treatments, such as chemotherapy and radiotherapy, are of
uncertain clinical value as there have been reported cases whereby
LGMS, excised along with free margins, demonstrated no recurrence
or metastasis either with or without ancillary treatment (39–42).
Furthermore, certain tumors have recurred or metastasized
subsequent to the administration of ancillary treatment (25). A previous study also reported that
unresectable LGMS demonstrated no response to the combination of
chemotherapy and radiotherapy, and resulted in mortality (28). In the present study, the patients
underwent wide local tumor excision, which included the removal of
tumor-free margins, and did not receive further ancillary therapy.
The lesion in case 2 recurred six months later, and a wide local
excision was performed again. Even though no further recurrence or
metastasis was identified six months post-operatively, further
follow-up is imperative.
Myofibroblastic sarcoma must be distinguished from
other neoplasms, as the lesion can resemble varying types of benign
myofibroblastic tumors, including nodular fasciitis, proliferative
myositis and fibromatosis, and also other types of low-grade
spindle-cell sarcomas, notably leiomyosarcoma and fibrosarcoma. The
differential diagnosis is usually made based upon clinical and
morphological features, combined with immunohistochemical analysis
and occasionally ultrastructural features (11,12).
As case 2 in the present study was misdiagnosed as an IMT, a
description of the differential diagnosis is subsequently
provided.
According to the 2002 World Health Organization
classification, IMT, which is synonymous with inflammatory
fibrosarcoma (43), is a locally
aggressive and rarely metastatic intermediate tumor (44). The tumor usually arises within the
lungs or the abdomen, particularly within the retroperitoneum or
mesentery, and on occasions in the visceral and soft-tissue sites
of the head, neck, trunk and extremities. IMT forms a solitary or
multicentric mass up to ~10 cm in diameter, has a peak incidence in
childhood or adolescence and exhibits a female predominance
(45,46). Furthermore, systemic features,
including anemia and hypergammaglobulinemia, which are potentially
associated with interleukin-6, are occasionally present. All the
aforementioned clinical features differ from those of LGMS.
Despite the similar infiltrating capacities of IMT
and LGMS, the histological growth patterns of the two lesions are
generally different. IMT presents with fasciitis-like, fascicular
and fibrosarcoma- or leiomyosarcoma-like hypocellular fibrous
areas, regions of hyalinization and calcification, and is
accompanied by permanent inflammation in the stroma, which is
primarily comprised of polyclonal plasma cells and lymphocytes
(24). The incidence of
pleomorphism or necrosis is low. Histologically, IMT is
multifocally- or diffusely-positive for α-SMA and MSA, and
occasionally for desmin. Certain CKs are also evident in certain
cases, particularly in intra-abdominal tumors (24). The immunoreactivity profile of ALK
reflects rearrangements in the ALK gene, which is located on
chromosome 2p23 and encodes a tyrosine kinase receptor. A variety
of fusion partners exist, of which tropomyosin 3 and 4 are the most
common (47).
When LGMS is accompanied by an inflammatory
background, it is increasingly difficult to distinguish it from
IMT. This often results in misdiagnosis, as in case 2 in the
present study. Occasionally, spindle-cell sarcoma, monophasic
synovial sarcoma, malignant peripheral nerve sheath tumors and
certain cases of angiosarcoma and spindle-cell rhabdomyosarcoma are
involved in the differential diagnosis.
Although the proportion of neoplastic myofibroblasts
required for a diagnosis of LGMS is not defined, the disease is
widely accepted as a distinct entity. Despite the fact that it
exhibits improved diagnostic specificity compared with myeloid
markers, the fibronexus has also been identified in fetal
endothelial cells, spindle-cell carcinomas (48) and more rarely in neoplastic,
compared with non-neoplastic, myofibroblasts. In recent years, the
ultrastructural features of myofibroblasts have been complemented
by histological and immunohistochemical criteria to produce a
comprehensive definition. Therefore, cases of LGMS that exhibit
actin and fibronectin positivity, but h-caldesmon and smooth muscle
myosin negativity, will for the majority of pathologists without
access to electron microscopy, be sufficient to reach a diagnosis.
However, in circumstances where it may be challenging to interpret
the results, for example, in instances of focal or equivocal
immunostaining, electron microscopy would be a useful tool to
provide maximum diagnostic confidence.
Although genetic changes have been identified that
prove that LGMS is a definite neoplasm, specific changes, such as
those evident in cases of infantile fibrosarcoma and IMT, require
identification by the application of suitable techniques to better
describe this entity.
Acknowledgements
The authors would like to thank Ms. Fengjie Miao for
supplying the materials and for assisting with the
immunohistochemical analyses.
References
|
1
|
Gabbiani G, Ryan GB and Majne G: Presence
of modified fibroblasts in granulation tissue and their possible
role in wound contraction. Experientia. 27:549–550. 1971.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Desmouliere A and Gabbiani G: The role of
the myofibroblast in wound healing and fibrocontractive diseases.
Molecular and Cellular Biology of Wound Repair. Clark RAF: 2nd
edition. Pentum Press; New York, NY: pp. 391–423. 1996
|
|
3
|
Schürch W, Seemayer TA and Gabbiani G: The
myofibroblast: a quarter century after its discovery. Am J Surg
Pathol. 22:141–147. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Eyden BP, Ponting J, Davies H, Bartley C
and Torgersen E: Defining the myofibroblast: normal tissues, with
special reference to the stromal cells of Wharton’s jelly in human
umbilical cord. J Submicrosc Cytol Pathol. 26:347–355.
1994.PubMed/NCBI
|
|
5
|
Schürch W, Seemayer TA, Hinz B and
Gabbiani G: Myofibroblast. Histology for Pathologists. Mills SE:
3rd edition. Lippincott, Williams & Wilkins; Philadelphia, PA:
pp. 123–164. 2007
|
|
6
|
Rønnov-Jessen L, Petersen OW, Koteliansky
VE and Bissell MJ: The origin of the myofibroblasts in breast
cancer. Recapitulation of tumor environment in culture unravels
diversity and implicates converted fibroblasts and recruited smooth
muscle cells. J Clin Invest. 95:859–873. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zeisberg EM, Tarnavski O, Zeisberg M, et
al: Endothelial-to-mesenchymal transition contributes to cardiac
fibrosis. Nat Med. 13:952–961. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gabbiani G: The myofibroblast in wound
healing and fibrocontractive diseases. J Pathol. 200:500–503. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Desmoulière A, Guyot C and Gabbiani G: The
stroma reaction myofibroblast: a key player in the control of tumor
cell behavior. Int J Dev Biol. 48:509–517. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gabbiani G: The cellular derivation and
the life span of the myofibroblast. Pathol Res Pract. 192:708–711.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fisher C: Myofibroblastic malignancies.
Adv Anat Pathol. 11:190–201. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fisher C: Myofibrosarcoma. Virchows Arch.
445:215–223. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Eyden B: The fibronexus in reactive and
tumoral myofibroblasts: further characterisation by electron
microscopy. Histol Histopathol. 16:57–70. 2001.PubMed/NCBI
|
|
14
|
Morgan PB, Chundru S, Hatch SS, et al:
Uncommon malignancies: case 1. Low-grade myofibroblastic sarcoma of
the breast. J Clin Oncol. 23:6249–6251. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mentzel T, Dry S, Katenkamp D and Fletcher
CD: Low-grade myofibroblastic sarcoma: analysis of 18 cases in the
spectrum of myofibroblastic tumors. Am J Surg Pathol. 22:1228–1238.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mentzel T and Fletcher JA: Low-grade
myofibroblastic sarcoma. Pathology and Genetics of Tumours of Soft
Tissue and Bone. Fletcher CDM, Unni KK and Mertens F: IARC Press;
Lyon, France: pp. 94–95. 2002
|
|
17
|
Nagata Y, Matsuno T, Hamada N, et al:
Low-grade myofibroblastic sarcoma of the palm. Scand J Plast
Reconstr Surg Hand Surg. 42:164–167. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Saito T, Mitomi H, Kurisaki A, et al:
Low-grade myofibroblastic sarcoma of the distal femur. Int J Surg
Case Rep. 4:195–199. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Morii T, Mochizuki K, Sano H, et al:
Occult myofibroblastic sarcoma detected on FDG-PET performed for
cancer screening. Ann Nucl Med. 22:811–815. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gonzalez-Palacios F, Enriquez JL, San
Miguel P, et al: Myofibroblastic tumors of the breast: A histologic
spectrum with a case of recurrent male breast myofibrosarcoma. Int
J Surg Pathol. 7:11–17. 1999. View Article : Google Scholar
|
|
21
|
Agaimy A, Wünsch PH, Schroeder J, et al:
Low-grade abdominopelvic sarcoma with myofibroblastic features
(low-grade myofibroblastic sarcoma): clinicopathological,
immunohistochemical, molecular genetic and ultrastructural study of
two cases with literature review. J Clin Pathol. 61:301–306. 2008.
View Article : Google Scholar
|
|
22
|
Miyazawa M, Naritaka Y, Miyaki A, et al: A
low-grade myofibroblastic sarcoma in the abdominal cavity.
Anticancer Res. 31:2989–2994. 2011.PubMed/NCBI
|
|
23
|
Ghadially FN: Diagnostic Electron
Microscopy of Tumours. Butterworth & Co., Ltd; London: 1980
|
|
24
|
Eyden B, Banerjee SS, Shenjere P and
Fisher C: The myofibroblast and its tumours. J Clin Pathol.
62:236–249. 2009. View Article : Google Scholar
|
|
25
|
Stark M, Hoffmann A and Xiong Z: Mammary
myofibrosarcoma: case report and literature review. Breast J.
17:300–304. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yamada T, Yoshimura T, Kitamura N, et al:
Low-grade myofibroblastic sarcoma of the palate. Int J Oral Sci.
4:170–173. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Khosla D, Yadav BS, Kumar R, et al:
Low-grade myofibroblastic sarcoma of the larynx: a rare entity with
review of literature. J Cancer Res Ther. 9:284–286. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Covello R, Licci S, Pichi B, et al:
Low-grade myofibroblastic sarcoma of the larynx. Int J Surg Pathol.
19:822–826. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Takahama A Jr, Nascimento AG, Brum MC,
Vargas PA and Lopes MA: Low-grade myofibroblastic sarcoma of the
parapharyngeal space. Int J Oral Maxillofac Surg. 35:965–968. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Demarosi F, Bay A, Moneghini L and
Carrassi A: Low-grade myofibroblastic sarcoma of the oral cavity.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 108:248–254.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Jay A, Piper K, Farthing PM, Carter J and
Diwakar A: Low-grade myofibroblastic sarcoma of the tongue. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod. 104:e52–e58. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Montgomery E, Goldblum JR and Fisher C:
Myofibrosarcoma: a clinicopathologic study. Am J Surg Pathol.
25:219–228. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kuhnen C, Homann HH and Mentzel T:
Myofibroblastic sarcoma of the thoracic wall. Change in appearance
in tumour recurrence. Pathologe. 24:128–135. 2003.(In German).
PubMed/NCBI
|
|
34
|
Watanabe K, Ogura G, Tajino T, Hoshi N and
Suzuki T: Myofibrosarcoma of the bone: a clinicopathologic study.
Am J Surg Pathol. 25:1501–1507. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Eyden BP and Christensen L: Leiomyosarcoma
versus myofibrosarcoma: observations and terminology. Ultrastruct
Pathol. 17:231–239. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Eyden B: The myofibroblast: a study of
normal, reactive and neoplastic tissues, with an emphasis on
ultrastructure. J Submicrosc Cytol Pathol. 7–166. 2007.
|
|
37
|
Watanabe K, Tanaka M, Takashi K, Yamada H
and Tajino T: Fibronexus in low-grade myofibrosarcoma: a case
report. Ultrastruct Pathol. 32:97–100. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Meng GZ, Zhang HY, Zhang Z, Wei B and Bu
H: Myofibroblastic sarcoma vs nodular fasciitis: a comparative
study of chromosomal imbalances. Am J Clin Pathol. 131:701–709.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Artopoulou II, Lemon JC, Clayman GL and
Chambers MS: Stent fabrication for graft immobilization following
wide surgical excision of myofibroblastic sarcoma of the buccal
mucosa: a clinical report. J Prosthet Dent. 95:280–285. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Murakami Y, Tsubamoto H, Hao H, Nishimoto
S and Shibahara H: Long-term disease-free survival after radical
local excision of low-grade myofibroblastic sarcoma of the vulva.
Gynecol Oncol Case Rep. 5:34–36. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Coyne JD: Low-grade myofibroblastic
sarcoma of the piriform fossa: a case report with a literature
review of a tumour with a predilection for the head and neck. Br J
Oral Maxillofac Surg. 45:335–337. 2007. View Article : Google Scholar
|
|
42
|
Niedzielska I, Janic T and Mrowiec B:
Low-grade myofibroblastic sarcoma of the mandible: a case report. J
Med Case Rep. 3:84582009. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Meis JM and Enzinger FM: Inflammatory
fibrosarcoma of the mesentery and retroperitoneum. A tumor closely
simulating inflammatory pseudotumor. Am J Surg Pathol.
15:1146–1156. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Fletcher CDM, Unni KK and Mertens F: World
Health Organization classification of tumours. Pathology and
Genetics of Tumours of Soft Tissue and Bone. IARC Press; Lyon,
France: 2002
|
|
45
|
Coffin CM, Dehner LP and Meis-Kindblom JM:
Inflammatory myofibroblastic tumor, inflammatory fibrosarcoma, and
related lesions: an historical review with differential diagnostic
considerations. Semin Diagn Pathol. 15:102–110. 1998.PubMed/NCBI
|
|
46
|
Coffin CM, Humphrey PA and Dehner LP:
Extrapulmonary inflammatory myofibroblastic tumor: a clinical and
pathological survey. Semin Diagn Pathol. 15:85–101. 1998.PubMed/NCBI
|
|
47
|
Lawrence B, Perez-Atayde A, Hibbard MK, et
al: TPM3-ALK and TPM4-ALK oncogenes in inflammatory myofibroblastic
tumors. Am J Pathol. 157:377–384. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Eyden BP: Brief review of the fibronexus
and its significance for myofibroblastic differentiation and tumor
diagnosis. Ultrastruct Pathol. 17:611–622. 1993. View Article : Google Scholar : PubMed/NCBI
|