Introduction
Renal cell carcinoma (RCC) accounts for ~3.8% of all
adult malignancies in the USA (1).
Recently, the number of patients diagnosed with RCC has increased
due to the development of diagnostic modalities, including
ultrasonography and CT (computed tomography). Approximately 20–30%
of RCC patients develop bone metastases (2), which represents the third most common
site of distant metastases in advanced RCC, following the lungs and
liver (3).
Radiographically, bone metastases from RCC are
predominantly osteolytic in nature and decrease bone integrity,
leading to significant patient morbidity due to the associated
skeletal-related events (SREs). SREs are defined as pathological
fractures, radiotherapy for bone pain, surgery for impending
fracture, spinal cord and nerve root compressions and
hypercalcemia. SREs may significantly decrease patient quality of
life. Radiotherapy is the most common SRE in RCC patients, as ~81%
of patients with RCC receive radiotherapy treatment and 29% require
orthopedic surgery (2).
Sorafenib is an epidermal growth factor receptor
(EGFR) tyrosine kinase inhibitor that has been used in molecularly
targeted therapy for advanced-stage renal cell cancer (RCC). In a
study by Escudier et al (4),
sorafenib treatment prolonged the median progression-free survival
of RCC patients (5.5 months), when compared with a placebo group
(2.8 months). However, there is little available information on the
radiological effects of sorafenib on the bone metastases of RCC.
The current study presents the case of a 59-year-old male with
metastatic RCC and multiple metastases of the femur and ilium, who
demonstrated marked recovery of the bone metastasis and reduction
of the lung metastases, following treatment with sorafenib. Written
informed consent was obtained from the patient.
Case report
A 59-year-old male was referred to the Department of
Orthopedic Surgery, Osaka City University Hospital (Osaka, Japan)in
February 2008. The patient presented with a seven-month history of
gradually increasing pain in the right leg. The patient had
previously visited Fuchu Hospital (Izumi, Japan) due to an abnormal
shadow on the right proximal femur and was subsequently referred to
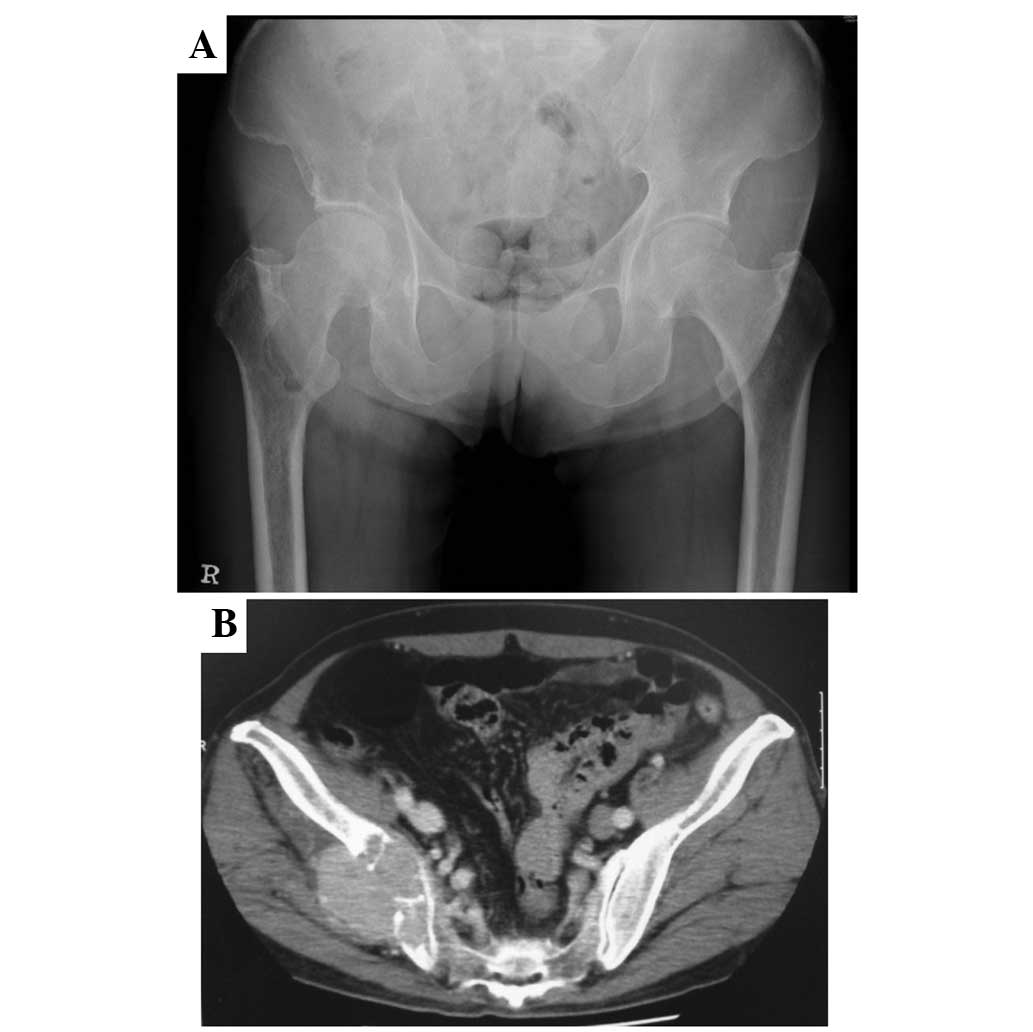
our hospital. A plain film revealed an osteolytic lesion with an
ill-defined margin in the right proximal femur (Fig. 1A), suggesting a malignant bone
tumor. Pelvic CT also revealed a mass in the right ilium, extending
into the gluteal muscle (Fig. 1B).
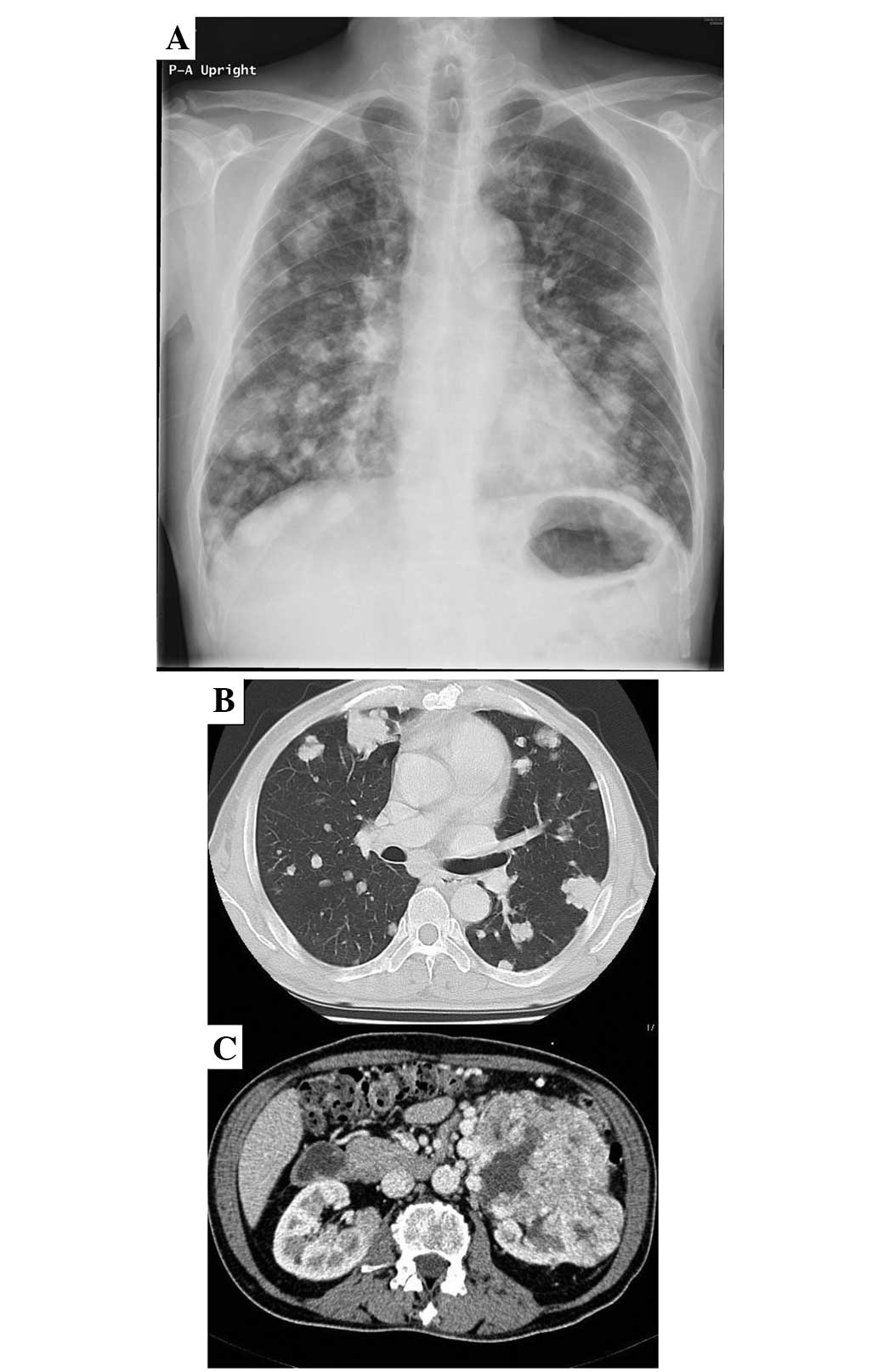
Lung plain film (Fig. 2A) and CT
(Fig. 2B) confirmed multiple masses
in bilateral lung fields. Screening of the abdominal CT to detect
the primary cancer revealed an occupying mass in the left kidney
(Fig. 2C). Other metastases
involving the pancreas and abdominal lymph nodes were also
revealed. Subsequent to consultation with the Department of Urology
and clinical staging, the patient was diagnosed with advanced-stage
RCC (cT3aN3M1; stage IV). Resection of the primary RCC and
palliative surgery with a γ-nail for an impending fracture of the
right proximal femur were performed simultaneously, which revealed
hemorrhagic brown tissue. The histology of a surgical specimen
revealed that the tumor was composed of cells with clear cytoplasm
and alveolar structural patterns. The pathological diagnosis of the
surgical specimen of the curettage material was consistent with
renal clear cell carcinoma.
At two weeks post-surgery, radiotherapy (36 Gy/12
fractions) was administered to the tumor in the right proximal
femur for three weeks and subcutaneous injection of interferon-α
(5×106IU) was started (5 times per week, for 9 months).
The patient then received 200 mg oral sorafenib combined with
interferon-α every day for two weeks, subsequently the dosage of
sorafenib was increased to 400 mg. No major adverse effects were
experienced, but a dry skin rash developed on the face and trunk,
and the patient experienced mild diarrhea. Subsequently, the dose
of sorafenib was reduced to 200 mg for two weeks. Four weeks later,
the dose was increased to 400 mg. Treatment with sorafenib was
continued for eight months and the dose (400–600 mg) was determined
according to the adverse effects experienced by the patient.
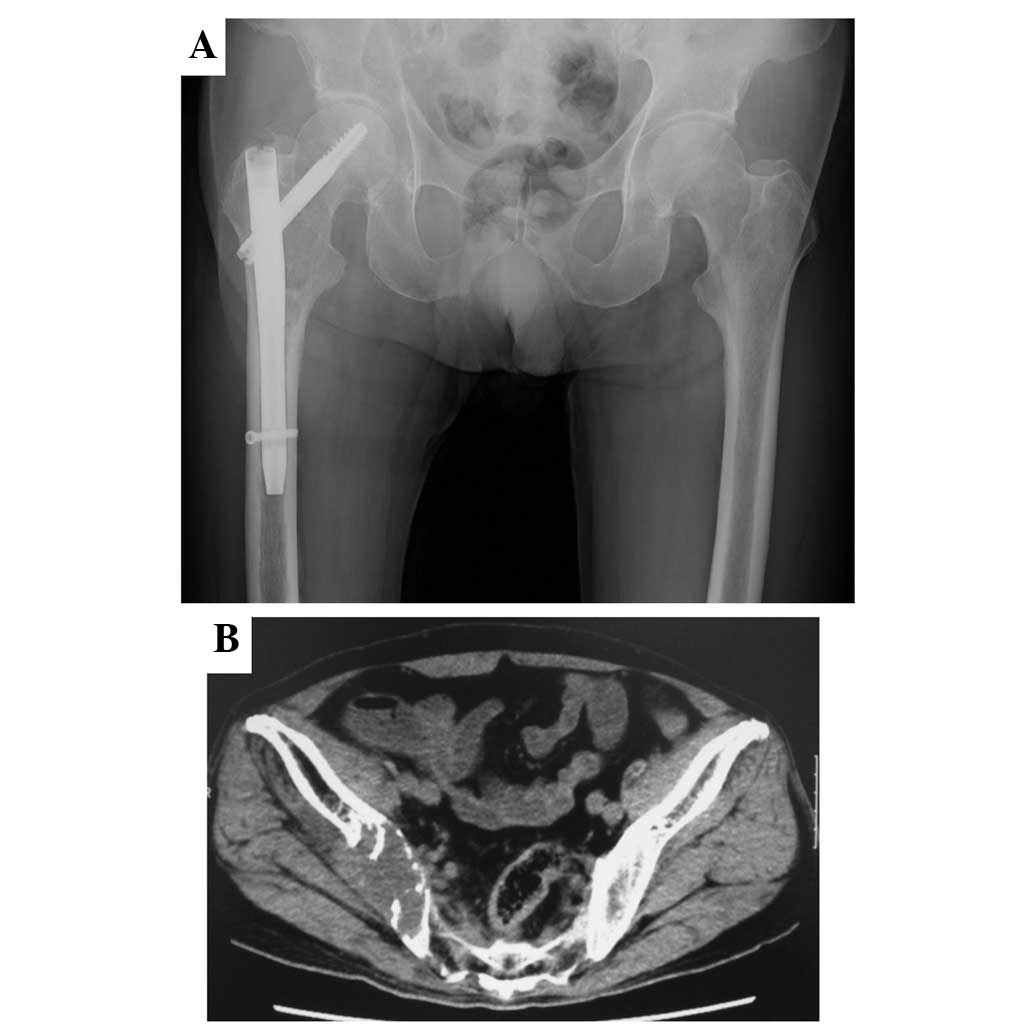
At eight months post-surgery, a plain film (Fig. 3A) showed no apparent progression in
the right femur, and pelvic CT demonstrated regression of the mass
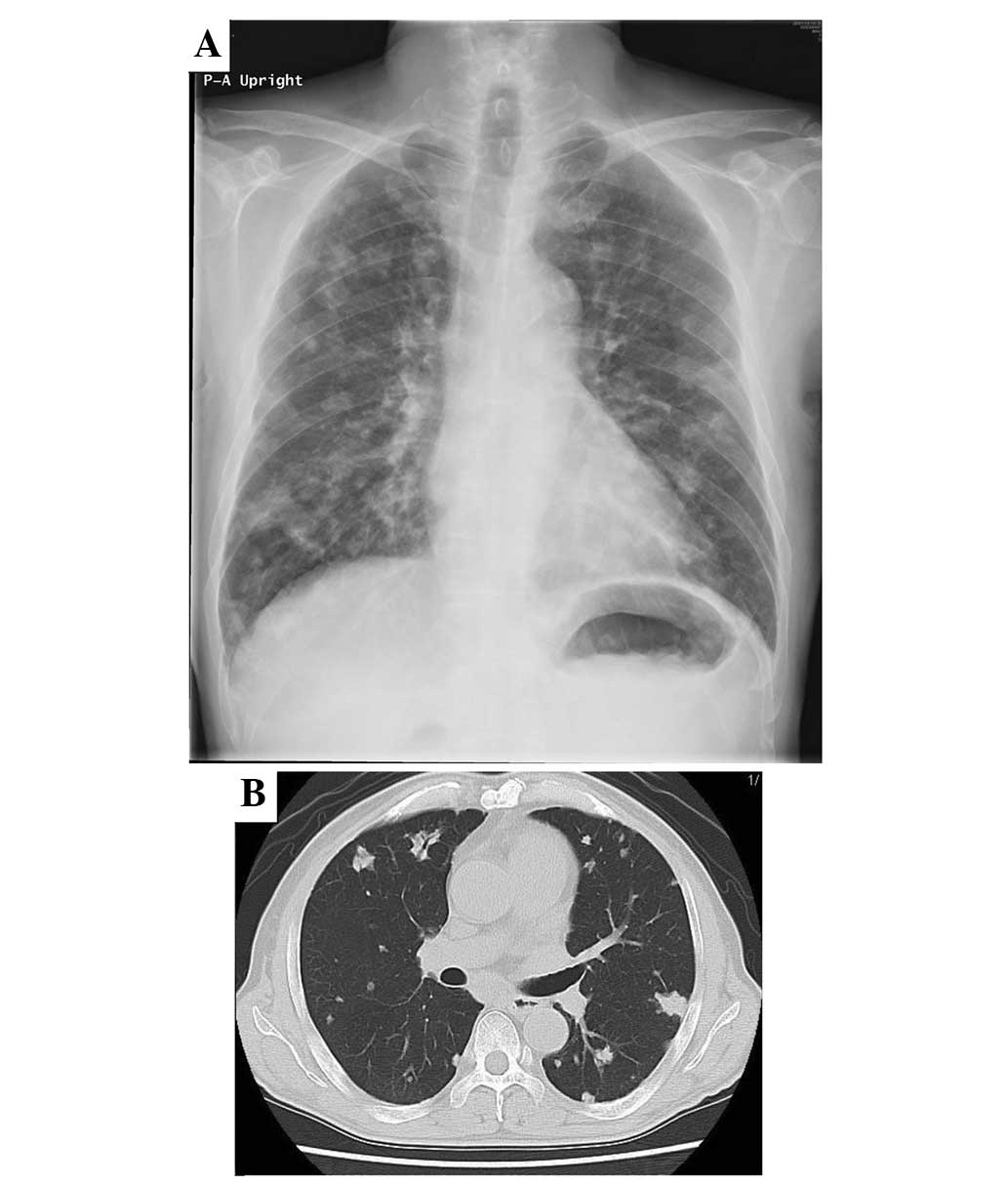
in the right ilium (Fig. 3B). Plain
film and CT of the lungs also revealed favorable responses
(Fig. 4). The abdominal lymph node
swelling was also reduced. The patient remained alive with the
disease at the time of follow-up at 36 months post-surgery.
Discussion
RCC is estimated to account for ~3.8% of all cancers
(1). RCC has a high mortality rate,
with a five-year survival rate of <10% (5), despite recent progress in various
therapeutic strategies. The bone remains one of the most common
distant metastatic sites of RCC. Patient quality of life is
negatively impacted by bone damage caused by developing bone
metastases (6), however, due to
severe pain and a poor performance status, the administration of
systemic chemotherapy is difficult. The prognosis is further
worsened by the unfavorable conditions (7).
Interferon-α and interleukin-2 are generally
accepted as the standard treatments for advanced-stage RCC
(8,9). However, sorafenib, a multi-kinase
inhibitor that blocks the raf and tyrosine kinases of vascular
endothelial and platelet-derived growth factor receptors, has been
recently introduced for the treatment of unresectable and/or
multiple metastatic RCC (4). In a
phase III randomized, placebo-controlled trial, sorafenib produced
a response in 10% of patients who were resistant to standard
therapy, and progression-free survival was significantly prolonged
from 2.8 to 5.5 months (10). In a
phase II study, progression-free survival in the sorafenib-treated
group was not significantly different from that in the
interferon-α-2a-treated group (10). In the current study, the patient
developed minor adverse effects, including a skin rash on the face
and trunk, and mild diarrhea, necessitating a temporary dose
reduction. Major adverse effects (grade, >3) of hand-foot skin
reactions (11.3%), diarrhea (6.2%) and rashes/desquamation (6.2%)
have previously been reported (10).
There is little information available concerning the
chemotherapeutic response of bone metastasis to sorafenib. Iliac
bone metastases in the current patient were significantly reduced
without the use of radiotherapy. The association between EGFR
kinase inhibitors and bone metastases has rarely been investigated.
Using prostate cancer cells, Angelucci et al (11) and Normanno and Gullick (12) suggested three possible pathways to
explain the beneficial effects of EGFR inhibitors on bone
metastases. Firstly, using cell invasion-related molecules,
including matrix metalloproteinase-9 and urokinase-type
plasminogen, EGFR tyrosine kinase inhibitors may act directly on
tumor cells. Secondly, EGFR inhibitors may exert anti-angiogenic
activity via the blockage of vascular endothelial growth factor
production. Thirdly, EGFR tyrosine kinase inhibitors may cause the
inhibition of osteoclast development by affecting the induction of
osteoclast differentiation and activation by bone marrow stromal
cells. These mechanisms could all act to prevent the expansion of
bone metastases.
The one-year survival rate of patients after
treatment for bone metastases from RCC was found to be 47%, when
compared with 31.6% for lung cancer patients (13,14).
However, the prognosis of the current patient at the initial
presentation was considered to be poor due to the presence of
multiple organ metastases, including lung, liver, pancreas and
lymph node metastases. Orthopedic surgery was performed using
γ-nail fixation as palliative therapy for preventing a pathological
fracture of the right femur. However, molecularly targeted therapy
with sorafenib led not only to bone recovery, but also improved the
survival time.
In conclusion, the current study reports the case of
a male patient with RCC who presented with bone metastases of the
right proximal femur and ilium. Marked tumor reduction was observed
subsequent to treatment with a combination of sorafenib and
interferon-α for 9 months. The patient remained alive at the time
of follow-up at 36 months post-surgery. Sorafenib administration is
a promising agent for improving the prognosis of patients with bone
metastases of RCC.
References
|
1
|
Jemal A, Siegel R, Ward E, et al: Cancer
statistics, 2008. CA Cancer J Clin. 58:71–96. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zekri J, Ahmed N, Coleman RE and Hancock
BW: The skeletal metastatic complications of renal cell carcinoma.
Int J Oncol. 19:379–382. 2001.PubMed/NCBI
|
|
3
|
Kyoda Y, Kobayashi K, Hirobe M, et al:
Evaluation of long-term outcome for patients with renal cell
carcinoma after surgery: analysis of cancer deaths occurring more
than 10 years after initial treatment. Int J Clin Oncol.
19:146–151. 2014. View Article : Google Scholar
|
|
4
|
Escudier B, Eisen T, Stadler WM, et al;
TARGET Study Group. Sorafenib in advanced clear-cell renal-cell
carcinoma. N Engl J Med. 356:125–134. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Motzer RJ, Bander NH and Nanus DM: Renal
cell carcinoma. N Engl J Med. 335:865–875. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Woodward E, Jagdev S, McParland L, et al:
Skeletal complications and survival in renal cancer patients with
bone metastases. Bone. 48:160–166. 2011. View Article : Google Scholar
|
|
7
|
Weiss RJ, Ekström W, Hansen BH, et al:
Pathological subtrochanteric fractures in 194 patients: a
comparison of outcome after surgical treatment of pathological and
non-pathological fractures. J Surg Oncol. 107:498–504. 2013.
View Article : Google Scholar
|
|
8
|
Negrier S, Perol D, Ravaud A, et al:
Medroxyprogesterone, interferon alfa-2a, interleukin 2, or
combination of both cytokines in patients with metastatic renal
carcinoma of intermediate prognosis: results of a randomized
controlled trial. Cancer. 110:2468–2477. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
McDermott DF, Regan MM, Clark JI, et al:
Randomized phase III trial of high-dose interleukin-2 versus
subcutaneous interleukin-2 and interferon in patients with
metastatic renal cell carcinoma. J Clin Oncol. 23:133–141. 2005.
View Article : Google Scholar
|
|
10
|
Escudier B, Szczylik C, Hutson TE, et al:
Randomized phase II trial of first-line treatment with sorafenib
versus interferon alfa-2a in patients with metastatic renal cell
carcinoma. J Clin Oncol. 27:1280–1289. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Angelucci A, Gravina GL, Rucci N, et al:
Suppression of EGF-R signaling reduces the incidence of prostate
cancer metastasis in nude mice. Endocr Relat Cancer. 13:197–210.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Normanno N and Gullick WJ: Epidermal
growth factor receptor tyrosine kinase inhibitors and bone
metastases: different mechanisms of action for a novel therapeutic
application? Endocr Relat Cancer. 13:3–6. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lin PP, Mirza AN, Lewis VO, et al: Patient
survival after surgery for osseous metastases from renal cell
carcinoma. J Bone Joint Surg Am. 89:1794–1801. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sugiura H, Yamada K, Sugiura T, Hida T and
Mitsudomi T: Predictors of survival in patients with bone
metastasis of lung cancer. Clin Orthop Relat Res. 466:729–736.
2008. View Article : Google Scholar : PubMed/NCBI
|