Introduction
Biological reconstruction of the knee extensor
mechanism following a wide resection for a juxta-articular
musculoskeletal malignancy is a challenging procedure (1). Although some surgical options including
latissimus dorsi (LD) free flap (2),
allografting (3), free grafting of
the fascia lata with the iliac bone (4) and a pedicle medial gastrocnemius flap
(5), have been reported to date, to
the best of our knowledge, only one case report in which the knee
extensor mechanism was biologically reconstructed with a free
frozen autograft has been published (6).
The present study reports a new surgical procedure
for the functional reconstruction of the knee extensor mechanism
with a pedicle frozen autograft, following the wide resection of a
prepatellar clear cell sarcoma. This case is discussed with
reference to the previously reported procedure. Written informed
consent was obtained from the patient.
Case report
Case presentation
A previously healthy 45-year-old male presented to
the Department of Orthopaedic Surgery, Fukushima Medical University
Hospital (Fukushima, Japan) with a two-year history of pain in the
right knee and a three-month history of painless soft tissue mass
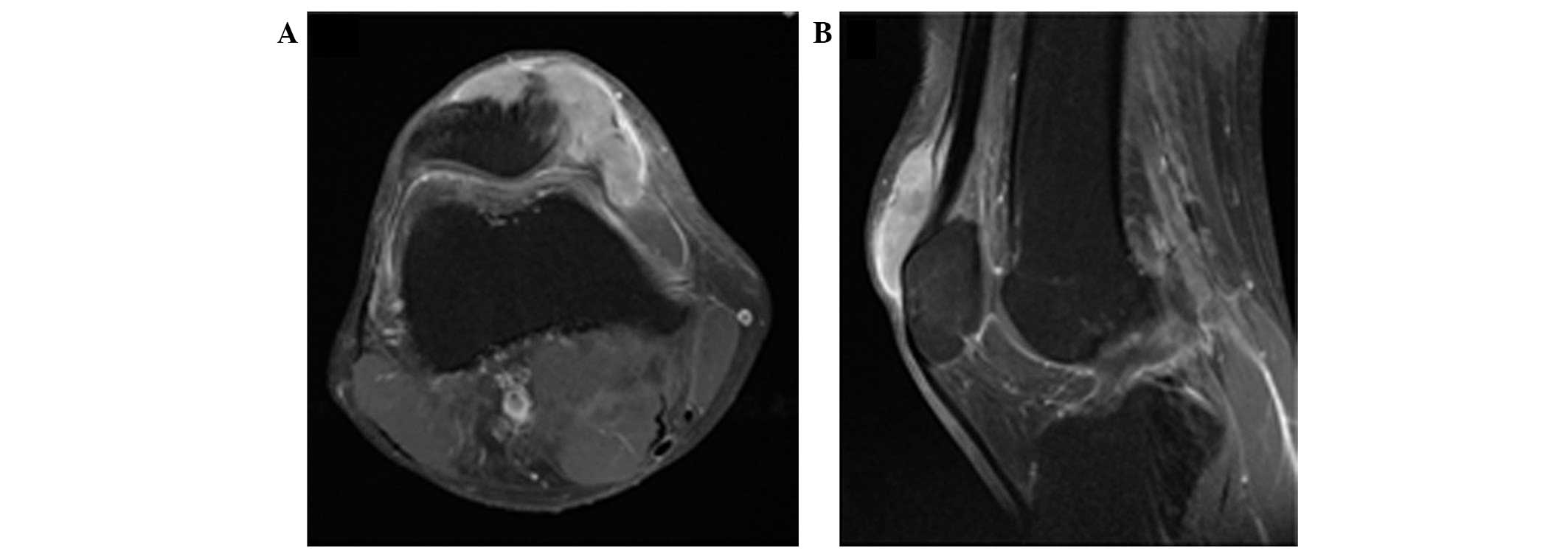
on the surface of the right patella. Magnetic resonance imaging
revealed a soft-tissue tumor growing on the surface of the
quadriceps femoris tendon and patella, measuring 57×50×29 mm
(Fig. 1). The tumor was diagnosed as
clear cell sarcoma following an incisional biopsy. An additional
radiological examination (chest computed tomography and whole-body
thallium scintigraphy) revealed no other tumorous regions
throughout the body.
Surgical technique
One month later, the patient underwent surgical
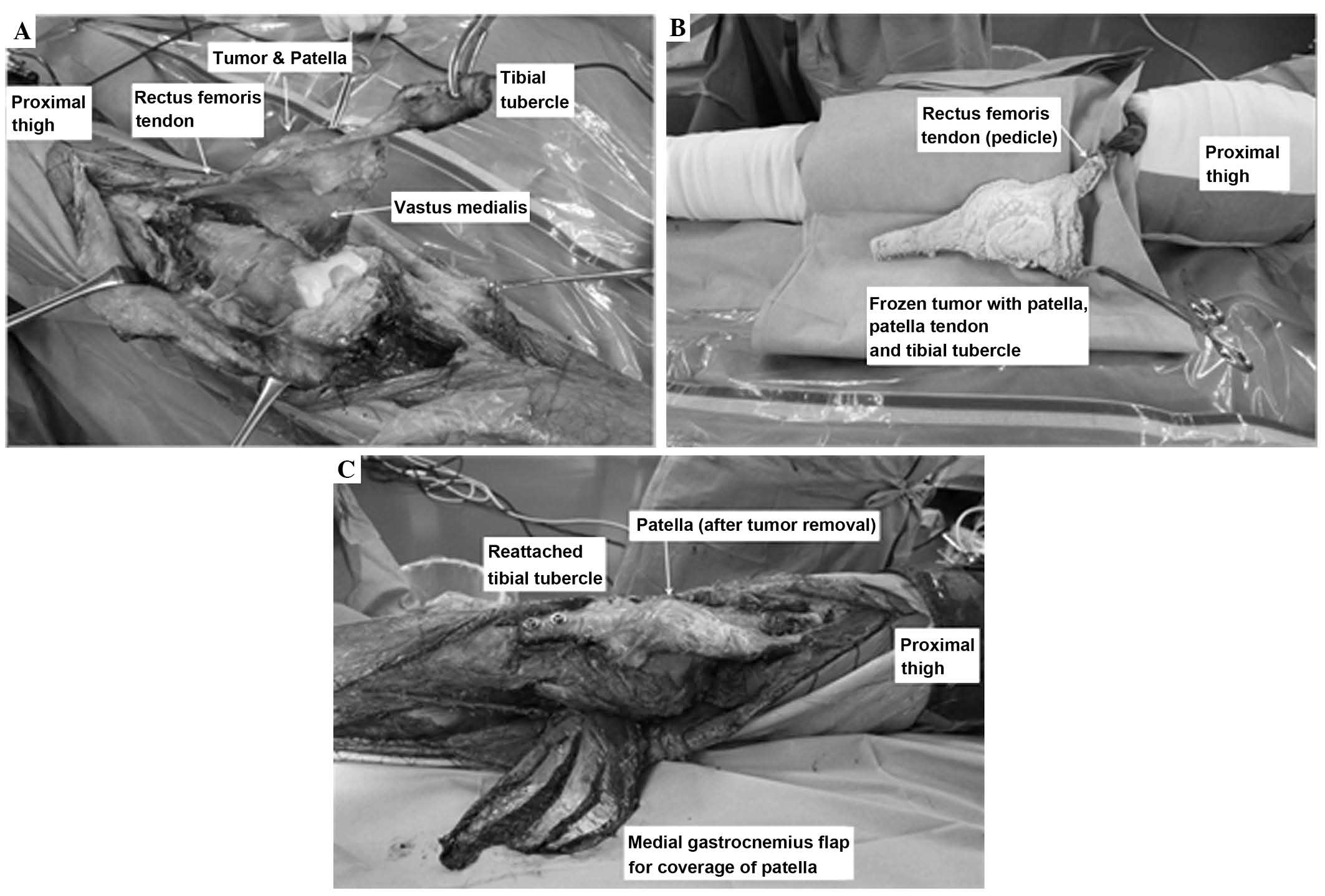
treatment for the removal of the tumor. An en-bloc wide resection
of the tumor and circumferential tissues, including the quadriceps
femoris (vastus medialis, intermedius and lateralis) tendon,
patella, patellar tendon and tibial tubercle, was performed. The
rectus femoris as a pedicle of the knee extensor mechanism was
spared (Fig. 2A). The quadriceps
tendon, patella, patellar tendon and tibial tubercle were soaked in
liquid nitrogen and frozen, maintaining the continuity of rectus
femoris muscle (Fig. 2B). Following
thawing, the tumor was resected and the tibial tubercle was
reattached to the tibia using two screws and spike washers
(Fig. 2C). The surface of the patella
and patellar tendon was covered with a medial gastrocnemius flap
and full-thickness skin graft.
Postoperative course
The knee was immobilized with a splint and was kept
non-weight-bearing for one week, followed by full-weight bearing
with straight-knee orthosis for three weeks. Mobilization of the
knee commenced concurrently. The patient began walking without
orthosis or a cane at four months post-surgery. Two courses of
adjuvant chemotherapy with cisplatin (200 mg, day 1), doxorubicin
(60 mg/m2, days 1 and 2) and caffeine (4,500
mg/m2, days 1–3) were administered every three weeks,
however, the patient declined continuation of chemotherapy due to
the adverse events experienced (nausea, G1; malaise, G2; white
blood cell reduction, G2) (7). Plain
radiographs taken six months following the surgery revealed
complete bone union of the site of the osteotomy (tibial tubercle),
and vertical fracture of the patella without trauma. The patellar
fracture was diagnosed as an insufficiency fracture and was treated
conservatively with the use of a straight-knee orthosis for four
weeks; the patient's knee function recovered without problem.
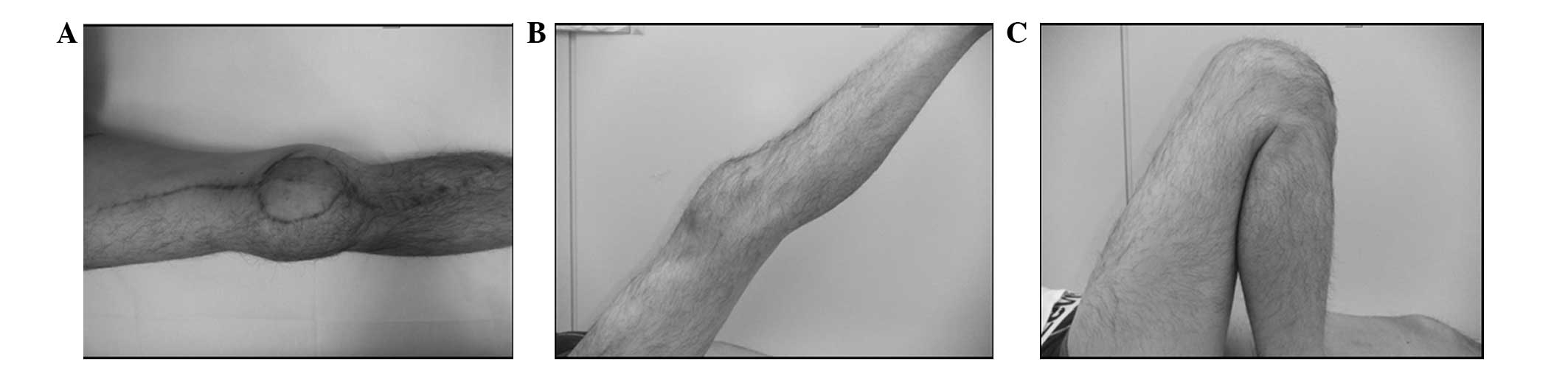
The physical examination at 14 months following
surgery showed that the active range of motion (ROM) of the knee
was from 0–135°, and the extension muscular strength of the knee
was evaluated as 5/5 by a manual muscle test (MMT) (Fig. 3). The patient was able to walk without
the assistance of a cane or a brace. Limb function was determined
to be 73% according to the International Society of Limb Salvage
(ISOLS) (8). Although there was no
indication of local recurrence, a small nodule was detected in the
left lung lobe (S10) 18 months postoperatively, and right inguinal
lymph node metastasis was discovered 24 months postoperatively. The
patient underwent a partial left lobectomy and a right inguinal
lymph node dissection at seven months following the diagnosis of
lung metastasis. The final follow-up was at 26 months after the
initial surgery for the knee and one month following the left
lobectomy and right inguinal lymphoidectomy. At that time, the
patient planned to receive additional chemotherapy.
Discussion
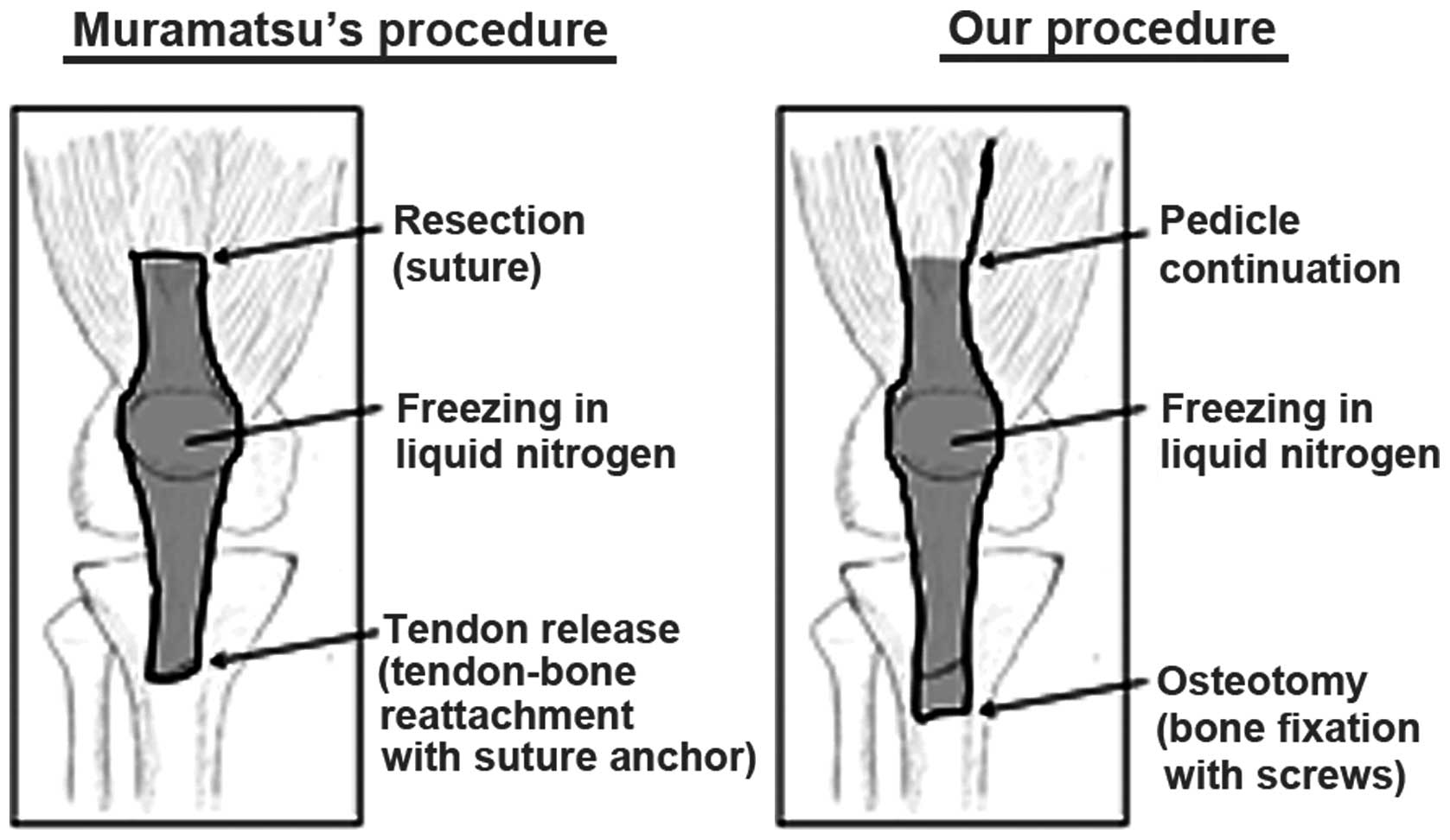
A similar surgical procedure was previously
described by Muramatsu et al (6). The quadriceps tendon, patella, and
patella tendon were resected with a prepatellar soft tissue sarcoma
(myxofibrosarcoma). Following the removal of the tumor, these
tissues were frozen in liquid nitrogen and subsequently reattached
to the remaining quadriceps muscle and tibial tubercle. The soft
tissue defect was covered by a LD free flap. The differences in the
reconstruction of the knee extensor mechanism in the current study,
compared with Muramatsu's procedure (6) are as follows: (i) The continuity of the
rectus femoris muscle is maintained in the current procedure,
conversely the muscle of the quadriceps is resected and sutured
after freezing in Muramatsu's procedure; (ii) an osteotomy of the
tibial tubercle was followed by bone-to-bone reattachment in the
current procedure, a patellar tendon release was followed by
tendon-bone reattachment with a suture anchor in Muramatsu's
procedure; and (iii) the frozen autograft was covered with a medial
gastrocnemius flap in the present study whereas an LD free flap is
used in Muramatsu's study. The characteristics of these procedures
are summarized in Fig. 4 and Table I.
 | Table I.The characteristics of the Muramatsu's
procedure (6) and the current
procedure. |
Table I.
The characteristics of the Muramatsu's
procedure (6) and the current
procedure.
|
| Muramatsu's procedure
(6) | Current
procedure |
|---|
| Blood supply | Discontinued | Preserved via rectus
femoris muscle |
| Reconstruction of
extensor mechanism | Tendon to bone
(patella tendon to tibial tubercle) | Bone to bone (tibial
tubercle to tibial shaft) |
| Procedure of
freezing | Simple (outside of
the body) | Complex (continuous
with the body) |
| Risk of
frostbite | No | Yes (protection of
the skin and soft tissue is required) |
| Coverage | Latissimus dorsi free
flap and split-thickness skin graft | Medial gastrocnemius
flap and full-thickness skin graft |
| Final functional
outcome [active ROM (extension/flexion) and MMT] | Active ROM: −10°/110°
MMT: 4+/5 | Active ROM: 0°/135°
MMT: 5/5 |
An advantage of the current procedure when compared
with Muramatsu's procedure (6), is
the continued blood supply to the frozen tissue through the
preserved rectus femoris muscle, which may lead to a shorter period
of bone union and fewer postoperative complications (9). Another advantage is the firm fixation of
the patellar tendon by bone-to-bone fixation with screws. However,
Muramatsu's procedure (6) used a
simple method for tissue freezing (outside of the body without
continuity), which has the advantage of preventing frostbite.
Although Muramatsu et al (6)
did not report their patient's ISOLS score, the final limb function
of the patient in the present study is thought to be superior,
based on the wider active ROM and stronger MMT scores.
For the coverage of the liquid nitrogen-treated
patella in the present case, a medial gastrocnemius flap was used,
whereas Muramatsu et al (6)
utilized the LD free flap. Although the use of an LD free flap
requires a more complicated method than a gastrocnemius flap, it's
use may be considered depending on the location of the tumor and
the size of soft tissue defect.
In the present study, a patellar vertical fracture
caused by insufficiency occurred in the patient six months
following the surgery. As bone revival following freezing with
liquid nitrogen typically takes a longer period than bone union
(10), it is possible, given the
timing of the fracture, that the patient's patella had not revived
yet.
In conclusion, functional reconstruction of the knee
extensor mechanism following a wide resection for a prepatellar
soft tissue sarcoma may be achieved using a pedicle frozen
auto-bone and -tendon graft. This technique allows for the
preservation of good limb function following surgery, even in
patients with juxta-articular malignant musculoskeletal tumors.
However, further study with a large number of patients treated
using this procedure is required in order to evaluate the whether
this is a feasible technique.
References
|
1
|
Ek EW, Rozen WM, Ek ET and Rudiger HA:
Surgical options for reconstruction of the extensor mechanism of
the knee after limb-sparing sarcoma surgery: an evidence-based
review. Arch Orthop Trauma Surg. 131:487–495. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Machens HG, Siemers F, Kaun M, et al:
Patellar tendon reconstruction using a free latissimus dorsi flap
following resection of a prepatellar myxofibrosarcoma: case report.
J Reconstr Microsurg. 21:235–238. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cho Y, Kim JD and Chung SH: Osteosarcoma
of the patella: biologic reconstruction with allograft.
Orthopedics. View Article : Google Scholar : 2009. View Article : Google Scholar
|
|
4
|
Nakashima H, Yoshida M and Miyamoto K:
Anatomical reconstruction of the patellar tendon using the fascia
lata attached to the iliac bone following resection for soft tissue
sarcoma: a case report. Ups J Med Sci. 117:460–464. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jentzsch T, Erschbamer M, Seeli F and
Fuchs B: Extensor function after medial gastrocnemius flap
reconstruction of the proximal tibia. Clin Orthop Relat Res.
471:2333–2339. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Muramatsu K, Yoshida K, Fujii K, Okazaki
T, Moriya A and Taguchi T: Anatomical reconstruction of the knee
extensor apparatus for prepatellar myxofibrosarcoma. Orthopedics.
33:7732010.PubMed/NCBI
|
|
7
|
National Cancer Institute, . CTCAE v4.03.
http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdfAccessed.
February 1–2015
|
|
8
|
Enneking WF, Dunham W, Gebhardt MC,
Malawar M and Pritchard DJ: A system for the functional evaluation
of reconstructive procedures after surgical treatment of tumors of
the musculoskeletal system. Clin Orthop Relat Res. 286:241–246.
1993.PubMed/NCBI
|
|
9
|
Shimozaki S, Yamamoto N, Shirai T, et al:
Pedicle versus free frozen autograft for reconstruction in
malignant bone and soft tissue tumors of the lower extremities. J
Orthop Sci. 19:156–163. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tanzawa Y, Tsuchiya H, Shirai T, Hayashi
K, Yo Z and Tomita K: Histological examination of frozen autograft
treated by liquid nitrogen removed after implantation. J Orthop
Sci. 14:761–768. 2009. View Article : Google Scholar : PubMed/NCBI
|