Introduction
Malignant melanoma exhibits a clear demographic and
ethnic disparity, being more common in Caucasians. Malignant
melanoma has the highest incidence in Queensland, Australia
(1), and is the fifth most commonly
diagnosed cancer in the United States (2). Compared with the high incidence of
malignant melanoma found in this population, the incidence in
non-Caucasians is low, therefore, the majority of research on
melanoma has focused on Caucasian populations. However, primary
gastrointestinal melanoma is relatively rare in the Asian
population and the literature surrounding this is limited. Primary
malignant melanoma of the esophagus (PMME) is a rare malignant
disease, accounting for only 0.1–0.2% of all esophageal neoplasms.
The mean survival time from diagnosis is only 13.4 months, and the
five-year survival rate is 4.2% worldwide (3,4).
Definitive diagnoses may be confirmed by pathological analysis and
positivity for S-100, human melanoma black (HMB)-45 and
melanoma-specific antigen (Melan-A) proteins on immunohistochemical
examination. Surgical extirpation is the standard treatment for
PMME. The current study presents a case of PMME in a Chinese
female. Written informed consent was obtained from the patient's
family.
Case report
In February 2013, a 65 year-old female was admitted
to the Drum Tower Hospital (Nanjing, China) with a two-month
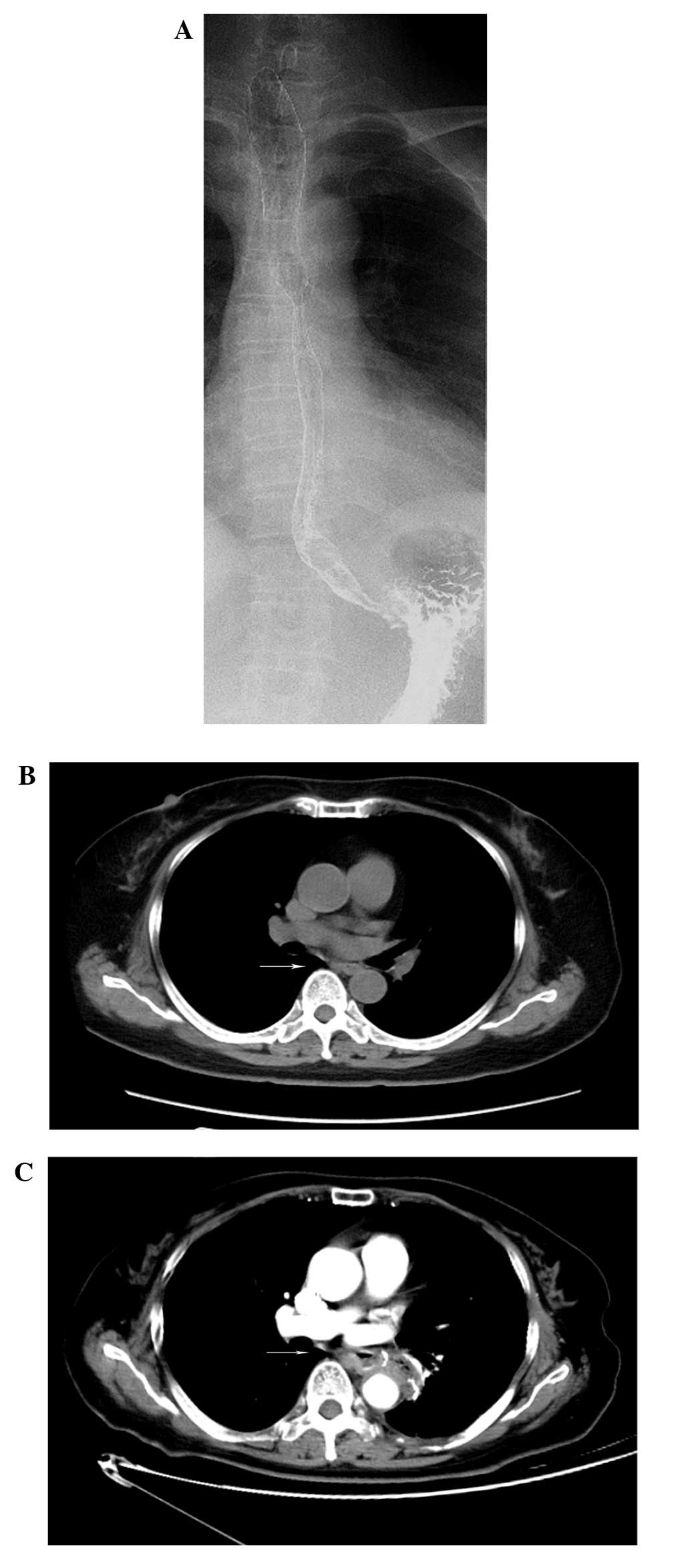
history of dysphagia. An upper gastrointestinal barium esophagogram
was conducted and revealed an intraluminal peduncular mass
extending into the esophagus (Fig.
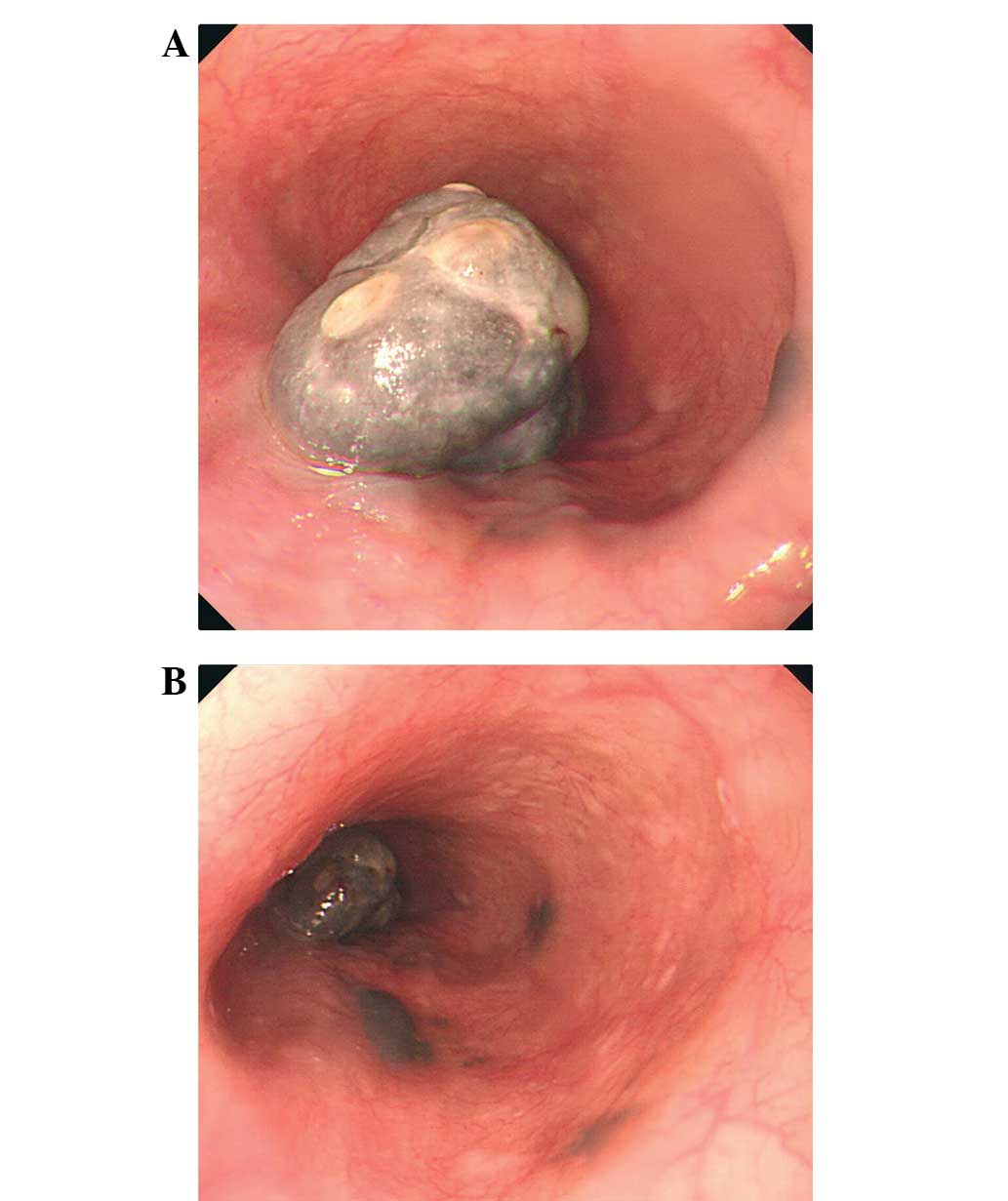
1A). Endoscopic examinations showed a 2.0×4.0-cm neoplasm with
black pigmentation; the neoplasm protruded into the esophageal
lumen and was located 30–33 cm from the incisors, with three flat,
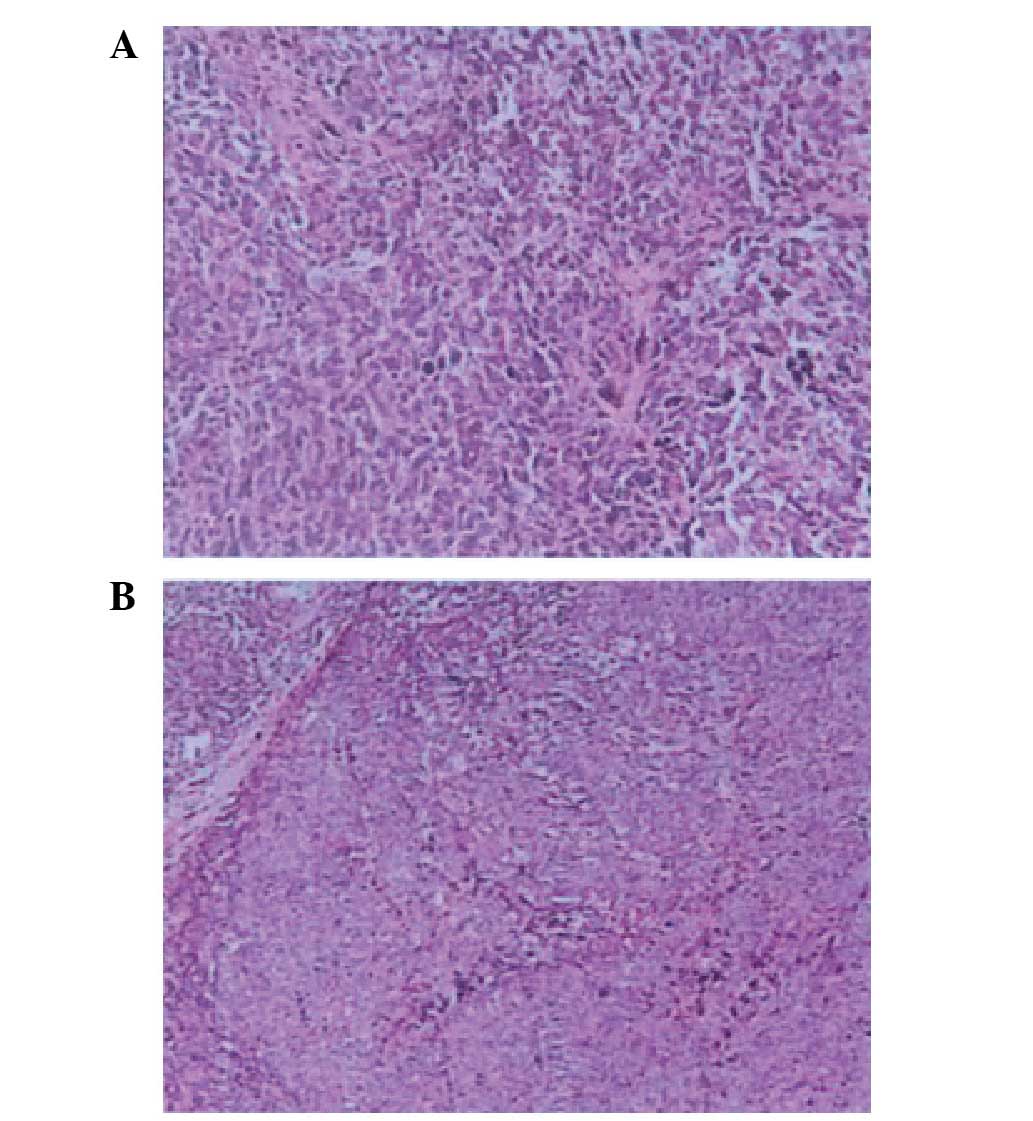
black-pigmented, 0.5×1.0-cm mucosal lesions (Fig. 2). Biopsy specimens identified foci
cells containing melanin (Fig. 3). No
primary cutaneous or ocular lesions were detected. Subsequent to
excluding other primary sites by computed tomography (CT; Fig. 1B), a PMME was suspected.
As a result, an esophagectomy with extensive lymph
node dissection was performed on February 19, 2013. Histologically,
the invasion of the tumors was limited to the submucosal layer and
no lymph node metastasis was detected. Evaluation of the resected
specimen demonstrated malignant melanoma in situ, and
subsequent immunohistology revealed that the tumor cells were
positive for the Melan-A, HMB-45, and the S-100 protein (Fig. 4), resulting in a diagnosis of
melanoma.
Next, two cycles of combined dendritic cell
(DC)-based immunotherapy were administered. The first cycle
consisted of adjuvant intravenous fotemustine (100
mg/m2, day 1) and intravenous oxaliplatin (100
mg/m2, day 1) chemotherapy, however, due to the severe
gastrointestinal reaction experienced by the patient, chemotherapy
was terminated. Instead, the patient was treated with traditional
Chinese medicine (20 mg ginsenoside Rg3, twice daily).
To date, the results of the most recent physical
examinations and blood tests, i.e., an esophagogastroduodenoscopy
conducted in April 2013 and a CT scan performed in August 2013
(Fig. 1C), have been unremarkable.
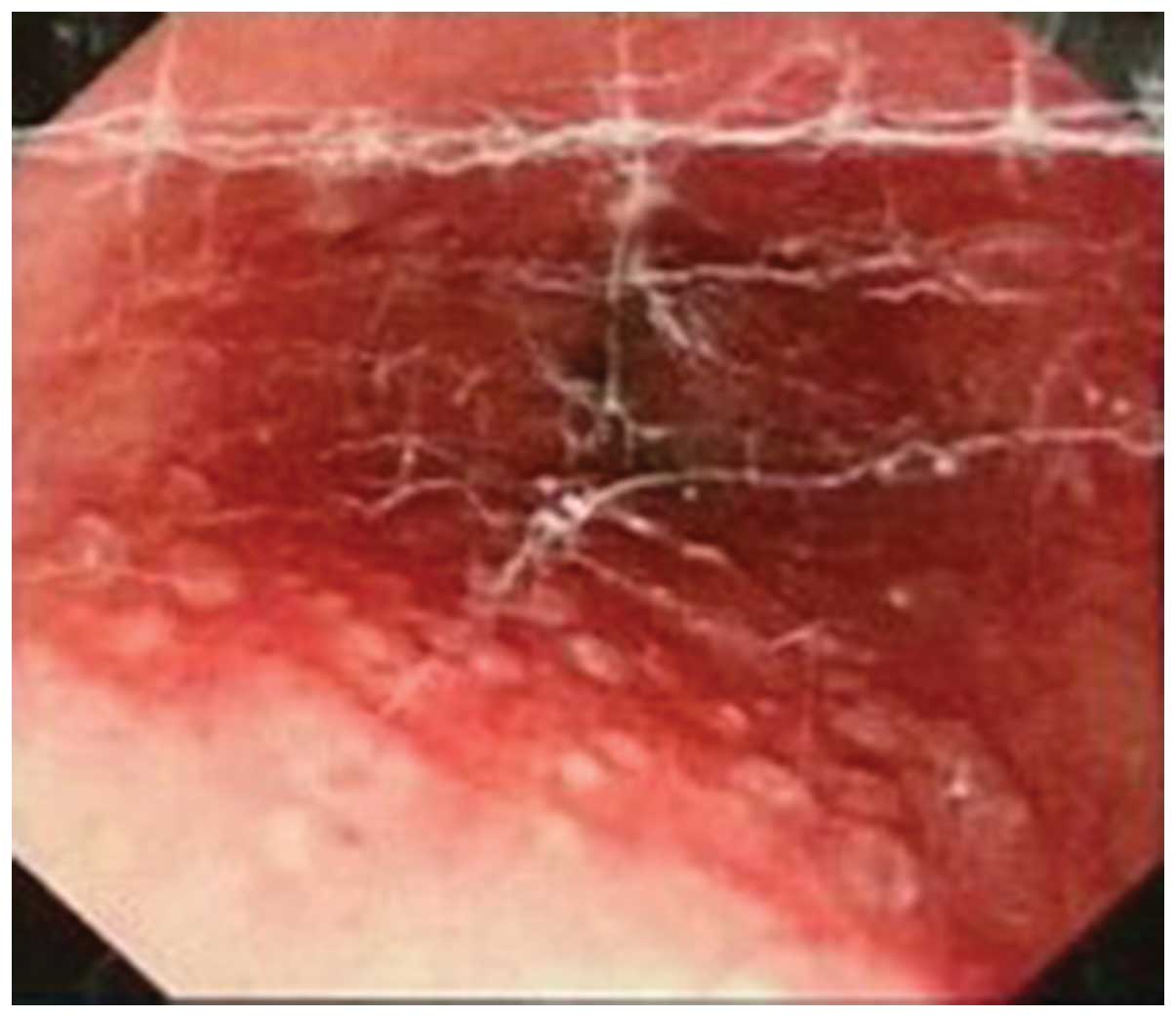
The patient was in a good general condition for 12 months
post-surgery. An endoscopic evaluation in May 2012 revealed a few
granule-like spots scattered in the lower esophagus, with no
melanin pigment (Fig. 5), indicating
squamous epithelial hyperplasia. The patient exhibited no clinical
symptoms therefore no further treatment was administered.
Discussion
PMME is characterized by aggressive behavior and a
poor prognosis, even following surgical resection. The average age
of onset is 60.5 years, which is younger than that of esophageal
carcinoma patients. The incidence of PMME in males is higher than
in females, with a ratio of 2:1 (3,4). The
majority of PMME patients present with the complaints of dysphagia,
non-specific retrosternal pain and weight loss. Occasionally,
hematemesis and melena are observed. The most common form of
recurrence for PMME is distant hematogenous metastasis, as opposed
to lymph node or regional recurrence. In the majority of patients
exhibiting tumors later than stage Ib, this recurrence has been
found to occur within ~1 year of surgery (5). In addition, ~90% of PMME lesions are
located in the distal two-thirds of the esophagus (6). Mehra et al (7) confirmed the role of tumor thickness as a
prognostic marker of mucosal melanoma; the survival time of
patients with mucosal melanoma depends on the primary's T-stage at
the time of diagnosis. While, no similar studies particularly
regarding PMME were found in the literature.
Even though the first case of malignant melanoma of
the esophagus was reported by Baur (8) in 1906, the condition was considered to
metastatic, originating from other sites of malignant melanoma.
This did not change until 1963 when De La Pava (9) reported the presence of typical
melanocytes in the esophageal epithelium. Volpin et al
(10) identified that 238 cases of
PMME had been reported up to early 2001 and that, by 2011, 337
cases had been reported (11). A
study by Ohashi et al (12)
revealed that the rate of esophageal melanocytosis was 7.7% among
healthy populations at autopsy and 29.9% among surgical esophageal
carcinoma cases in Japanese patients. Furthermore, the results
indicated that the increase in melanocytes observed in areas of
hyperplastic epithelium and chronic esophagitis may act as
precursor lesions for malignant melanoma in the esophagus.
The PMME diagnostic criteria defined in the study by
Allen and Spitz (13) include: i) A
typical histological pattern of melanoma and the presence of
melanin granules within the tumor cells; ii) an origin in an area
of junctional change within the squamous epithelium; and iii)
junctional activity with melanotic cells in the adjacent
epithelium. These criteria, the presence of in situ melanoma
and/or satellite tumors with no previous history of cutaneous
melanoma, and a systematic investigation with pathological
examination are required for a definitive diagnosis of PMME.
According to endoscopy, PMME is characterized by a
well-circumscribed, elevated and pigmented tumor, partially covered
by healthy mucosa, and rarely accompanied by ulcers. Although the
unique black pigmentation is an established characteristic of PMME,
10–25% of melanomas may exhibit a variety of other colors,
including tan, dark brown, black, blue, red and occasionally light
gray. Conversely, melanomas that lack pigment also exist; these are
termed amelanotic melanomas (14,15).
Bisceglia et al (11)
presented a case of primary malignant melanoma of the esophagus of
the amelanotic variant in a 69-year-old male, however, cases of
amelanotic melanomas are not common; Terada (16) reviewed 910 consecutive esophageal
biopsies obtained by the Department of Pathology, Shizuoka City
Shimizu Hospital (Shimizu, China), in the previous 15 years, and
identified only two cases of primary amelanotic malignant melanoma
(0.2%).
Biopsies may provide definitive diagnoses, however,
a number of patients have been previously misdiagnosed due to the
absence of melanin granules. Thus, immunohistochemical
investigations are required for a definitive diagnosis; this
includes positive immunohistochemical staining for S100 protein,
HMB-45 and Melan-A (15).
No gold standard has been established for the
treatment of PMME. Kimura et al (17) reported the use of endoscopic mucosal
resection for the treatment of early PMME, and recorded no
recurrence after 18 months. Consistent with this finding, Cheung
et al (18) evaluated the
Surveillance, Epidemiology and End Results database of primary
gastrointestinal melanomas (1973–2004) and identified complete
surgical resection as the only identifiable treatment strategy that
significantly improved survival in PMME patients. Therefore, the
present study proposes that the timely surgery received by the
current patient was significantly associated with the outcome, as
the patient remained in good condition 12 months after
esophagectomy.
Alternative non-surgical or surgical-adjuvant
therapies for PMME patients include chemotherapy,
chemoradiotherapy, endocrine therapy and immunotherapy, however,
these treatment strategies have yet to be fully evaluated.
Nevertheless, even in those patients who were successfully
administered these treatments, the majority also underwent surgery
(19–23).
Uetsuka et al (20) reported a long-term eight-year survival
period in an advanced PMME patient who underwent a radical
esophagectomy and lymphadenectomy, pre-operative and post-operative
chemoendocrine therapy, and immunohormone therapy. The treatment
course consisted of 200 mg/day dacarbazine for five days, 100 mg
nimustine for one day, 35 mg/day cisplatin for three days and 20
mg/day oral tamoxifen for seven days.
As extremely efficient antigen-presenting cells, DCs
are essential for the initiation of the T-lymphocyte-dependent
specific immune response. The study by Asakage et al
(21) was the first to report a case
of PMME treated with adjuvant dendritic cell therapy following
esophagectomy, which exhibited no recurrence 30 months after
surgery. Additionally, Ueda et al (20) was the first to report on the effect of
active specific immunotherapy using monocyte-derived DCs pulsed
with the epitope peptides of melanoma-associated antigens (MAGE)-1
and −3. This novel technique was administered to two
HLA-A24-positive PMME patients. Prior to specific immunotherapy,
the patients each underwent a radical esophagectomy with regional
lymphadenectomy, followed by treatment with dacarbazine, nimustine,
vincristine and interferon-α as adjuvant chemotherapy. One of the
patients was treated with active specific immunotherapy focusing on
a large abdominal lymph node metastasis. The patient survived for
12 months subsequent to the initiation of immunotherapy, with a
stable disease state for the first five months. In the second
patient, immunotherapy was administered post-operatively following
adjuvant chemotherapy. No tumor recurrence was observed for 16
months after the immunotherapy and the patient remains alive 49
months after esophagectomy (22).
Successful therapeutic cases of PMME using
completely non-surgical treatment strategies have been reported,
albeit only sporadically. For example, in one previous study, two
patients who were considered unsuitable for surgery due to their
age and general poor health were treated with a combination of
external radiotherapy and hyperthermia (HT) (23). A total dose of 35 Gy external
radiotherapy was administered as seven fractions of 5 Gy twice a
week, and combined with external and intraluminal HT once a week
(optimal temperature, 43°C). The results varied, with one patient
succumbing to a fast-growing distant metastasis 11 months
post-treatment, and the other patient achieving complete remission.
This second patient remained alive and in good general condition at
15 months post-treatment, with no signs of local recurrence or
distant metastasis.
The present study reports a rare case of PMME in a
female patient. Treatment recommendations for PMME patients are
based almost exclusively upon small, retrospective studies;
systemically established optimal management strategies remain
unknown and require investigation. Surgical resection is currently
the preferred treatment strategy for PMME, however, the prognosis
of affected patients remains extremely poor, with a reported median
overall survival period of 10–14 months (3,4). The
majority of patients succumb due to fast disease recurrence even
after curative resection. In conclusion, considering the typically
poor outcomes of PMME patients, it is possible that the treatment
strategy received by the current patient (chemotherapy,
immunotherapy, esophagectomy and traditional Chinese medicine
treatment), particularly esophagectomy, may have contributed to the
patient's good condition 12 months after surgery.
References
|
1
|
Curado MP, Edwards B, Shin HR, et al:
Cancer Incidence in Five Continents. No. 160, Volume IX. IARC
Scientific Publications; Lyon: 2007
|
|
2
|
Jemal A, Siegel R, Ward E, et al: Cancer
statistics, 2009. CA Cancer J Clin. 59:225–249. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sabanathan S, Eng J and Pradhan GN:
Primary malignant melanoma of the esophagus. Am J Gastroenterol.
84:1475–1481. 1989.PubMed/NCBI
|
|
4
|
Chalkiadakis G, Wihlm JM, Morand G, et al:
Primary malignant melanoma of the esophagus. Ann Thorac Surg.
39:472–475. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang S, Tachimori Y, Hokamura N, et al:
Diagnosis and surgical outcomes for primary malignant melanoma of
the esophagus: a single-center experience. Ann Thorac Surg.
96:1002–1006. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sanchez AA, Wu TT, Prieto VG, et al:
Comparison of primary and metastatic malignant melanoma of the
esophagus: clinicopathologic review of 10 cases. Arch Pathol Lab
Med. 132:1623–1629. 2008.PubMed/NCBI
|
|
7
|
Mehra T, Grözinger G, Mann S, et al:
Primary localization and tumor thickness as prognostic factors of
survival in patients with mucosal melanoma. PLoS One.
9:e1125352014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Baur EH: A case of primary melanoma of the
esophagus. Arb Geb Pathol Anat Inst Tubingen. 5:343–354. 1906.(In
German).
|
|
9
|
De La Pava S, Nigogosyan G, Pickren JW and
Cabrera A: Melanosis of the esophagus. Cancer. 16:48–50. 1963.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Volpin E, Sauvanet A, Couvelard A, et al:
Primary malignant melanoma of the esophagus: a case report and
review of the literature. Dis Esophagus. 15:244–249. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bisceglia M, Perri F, Tucci A, et al:
Primary malignant melanoma of the esophagus: a clinicopathologic
study of a case with comprehensive literature review. Adv Anat
Pathol. 18:235–252. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ohashi K, Kato Y, Kanno J, et al:
Melanocytes and melanosis of the oesophagus in Japanese
subjects-analysis of factors effecting their increase. Virchows
Arch A Pathol Anat Histopathol. 417:137–143. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Allen AC and Spitz S: Malignant melanoma;
a clinicopathological analysis of the criteria for diagnosis and
prognosis. Cancer. 6:1–45. 1953. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Taniyama K, Suzuki H, Sakuramachi S, et
al: Amelanotic malignant melanoma of the esophagus: case report and
review of the literature. Jpn J Clin Oncol. 20:286–295.
1990.PubMed/NCBI
|
|
15
|
Joob AW, Haines GK III, Kies MS, et al:
Primary malignant melanoma of the esophagus. Ann Thorac Surg.
60:217–222. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Terada T: A clinicopathologic study of
esophageal 860 benign and malignant lesions in 910 cases of
consecutive esophageal biopsies. Int J Clin Exp Pathol. 6:191–198.
2013.PubMed/NCBI
|
|
17
|
Kimura H, Kato H, Sohda M, et al:
Flat-type primary malignant melanoma of the esophagus treated by
EMR: case report. Gastrointest Endosc. 61:787–789. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cheung MC, Perez EA, Molina MA, et al:
Defining the role of surgery for primary gastrointestinal tract
melanoma. J Gastrointest Surg. 12:731–738. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Naomoto Y, Perdomo JA, Kamikawa Y, et al:
Primary malignant melanoma of the esophagus: report of a case
successfully treated with pre- and post-operative adjuvant
hormone-chemotherapy. Jpn J Clin Oncol. 28:758–761. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Uetsuka H, Naomoto Y, Fujiwara T, et al:
Primary malignant melanoma of the esophagus: long-term survival
following pre- and postoperative adjuvant hormone/chemotherapy. Dig
Dis Sci. 49:1646–1651. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Asakage M, Kitayama J, Tsuno NH, et al:
Primary malignant melanoma of the esophagus treated by
esophagectomy and adjuvant dendritic-cell therapy. J Gastroenterol.
40:545–546. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ueda Y, Shimizu K, Itoh T, et al:
Induction of peptide-specific immune response in patients with
primary malignant melanoma of the esophagus after immunotherapy
using dendritic cells pulsed with MAGE peptides. Jpn J Clin Oncol.
37:140–145. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hulshof MC, Van Haaren PM, Zum Vörde Sive
Vörding PJ, et al: Radiotherapy combined with hyperthermia for
primary malignant melanomas of the esophagus. Dis Esophagus.
23:E42–E47. 2010. View Article : Google Scholar : PubMed/NCBI
|