Introduction
Chronic neutrophilic leukemia (CNL) presents as a
distinct clinicopathological entity, exhibiting the characteristics
of mature neutrophilic leukocytosis and splenomegaly with bone
marrow granulocytic hyperplasia without evidence of dysplasia or
striking reticulin fibrosis (1).
Multiple myeloma (MM) is a condition that is associated with the
monoclonal proliferation of plasma cells that have differentiated
from lymphoid B cells (2). Thus, the
abnormal cell types observed in CNL and MM are markedly different,
originating from myeloid and lymphoplasmacytic cell lineages,
respectively (3,4). A small number of cases of CNL occurring
concurrently with MM have been reported, however, the
clinicopathological characteristics of the disease remain unclear,
and the clonal cytogenetic abnormalities have not been identified
in this specific group of patients. The current study presents the
case of a patient with concurrent CNL and MM who subsequently
developed acute myeloid leukemia. The patient achieved complete
remission (CR) following induction chemotherapy with decitabine and
the cytarabine, aclarubicin and granulocyte-colony stimulating
factor (G-CSF) (CAG) priming regimen. Consent was obtained from the
family of the patient.
Case report
A 78-year-old male presented with leukocytosis
(leukocyte count, 47,500/µl; normal range, 4,000–10,000/µl) on a
routine complete blood count prior to cataract surgery in The First
Affiliated Hospital of Nanjing Medical University, Jiangsu
Hospital, (Nanjing, China) in 2009. Hemoglobin and thrombocyte
counts were within the normal ranges. The patient experienced no
subjective symptoms. Moderate hepatosplenomegaly was identified,
however, no lymphadenopathy was evident. A bone marrow aspirate
smear revealed hypercellularity with a large number of neutrophils,
including segmented neutrophils (40.4%), band forms (19.6%),
myelocytes (13.6%), lymphocytes (6%) and a few rare cells, such as
blast cells and plasma cells.. The peripheral blood film contained
segmented neutrophils (80%), band forms (6%), lymphocytes (11%),
monocytes (2%) and eosinophils (1%).
Neutrophil alkaline phosphatase staining indicated
that the neutrophils were strongly positive with a high score.
Conventional cytogenetic analysis was performed on bone marrow
cells using the direct method (5), as
well as 24 h of non-stimulated culture of fresh heparinized bone
marrow cells. R-banding results revealed that the karyotype of the
patient was 46,XY [20]. Dual color dual fusion fluorescence in
situ hybridization (FISH) using BCR/ABL probes (Vysis, Inc.,
Downers Grove, IL, USA) to detect the Philadelphia chromosome was
also performed to exclude chronic myeloid leukemia (CML), and the
results showed that screening for BCR/ABL fusion was negative in
all 300 examined interphase cells. Polymerase chain reaction
analysis was performed to determine BCR/ABL fusion gene status,
which was also confirmed to be negative. Reactive neutrophilia and
other myeloproliferative neoplasms were excluded by clinical and
laboratory observation. A diagnosis of CNL was established
according to the criteria of the World Health Organization
Classification of Tumors of Hematopoietic and Lymphoid Tissues
(6) and thus, the patient was
administered hydroxyurea at a dose of 1 g twice per day., with the
dose adjusted according to the leukocyte count.
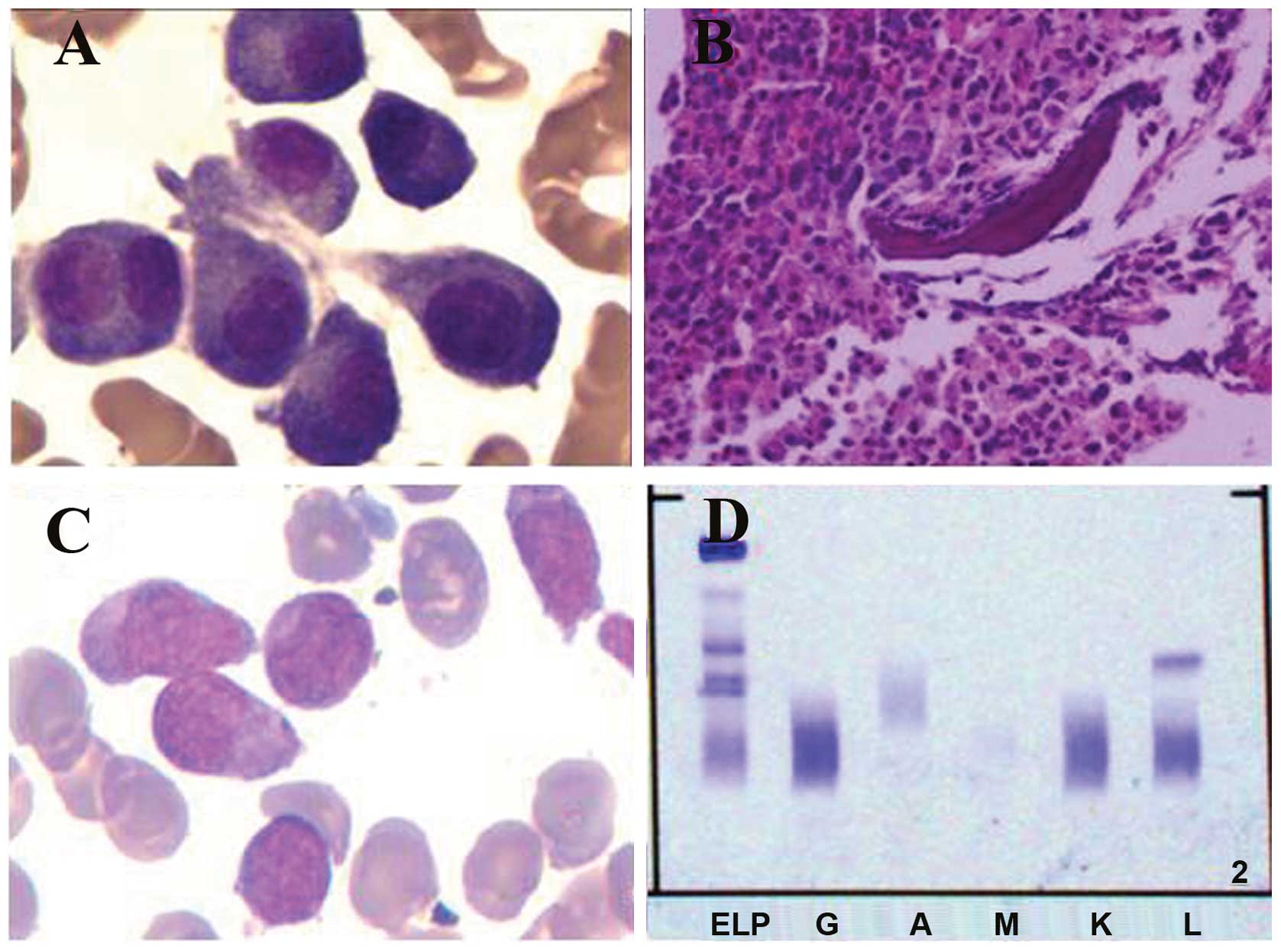
After ∼14 months, a bone marrow aspirate revealed
that the number of plasma cells was increased to 6.4%, including
plasmablastic, immature plasma and multinucleated plasma cells
(Fig. 1). The bone marrow biopsy
indicated the coexistence of myeloproliferative and plasma
neoplasms. The abnormal plasma cells were cluster of
differentiation (CD)38(+), CD138(+) and epithelial membrane
antigen(+/-) (Fig. 1). Karyotype
analysis was repeated and again revealed a karyotype of 46,XY [15].
Interphase FISH analysis combined with magnetic-activated cell
sorting (MACS), which markedly enhances the sensitivity of
cytogenetic analysis, was performed. Five different probes specific
for the regions containing 13q14.3, 14q32, 1q21, 1p12 and 17p13
were used to detect chromosomal aberrations. Positive values were
identified for 13q14.3, 17p13 and 1q21, while negative values were
identified for the probes specific for 1p13 and 14q32.
Immunoglobulin (Ig) tests showed an IgM level of 0.27 g/l (normal
range, 0.4–2.3 g/l), while IgG and IgA levels were within the
normal ranges. The β2 microglobulin level was 5.17 mg/l (normal
range, 0–3 mg/l) and the urine κ- and λ-light chains for 24 h were
70.8 and 434 mg, respectively. Serum protein immunofixation
electrophoresis showed a sharp positive band for the λ-light chain
subtype (Fig. 1). Bone magnetic
resonance imaging (MRI) indicated diffused lesions in multiple
vertebrae. The concurrent existence of MM was established and thus,
cyclophosphamide (50mg daily, d1-21), prednisone (30mg daily,
d1-21) and thalidomide (100mg, every night) were subsequently
administered for the treatment of MM. Each cycle was 1 month.
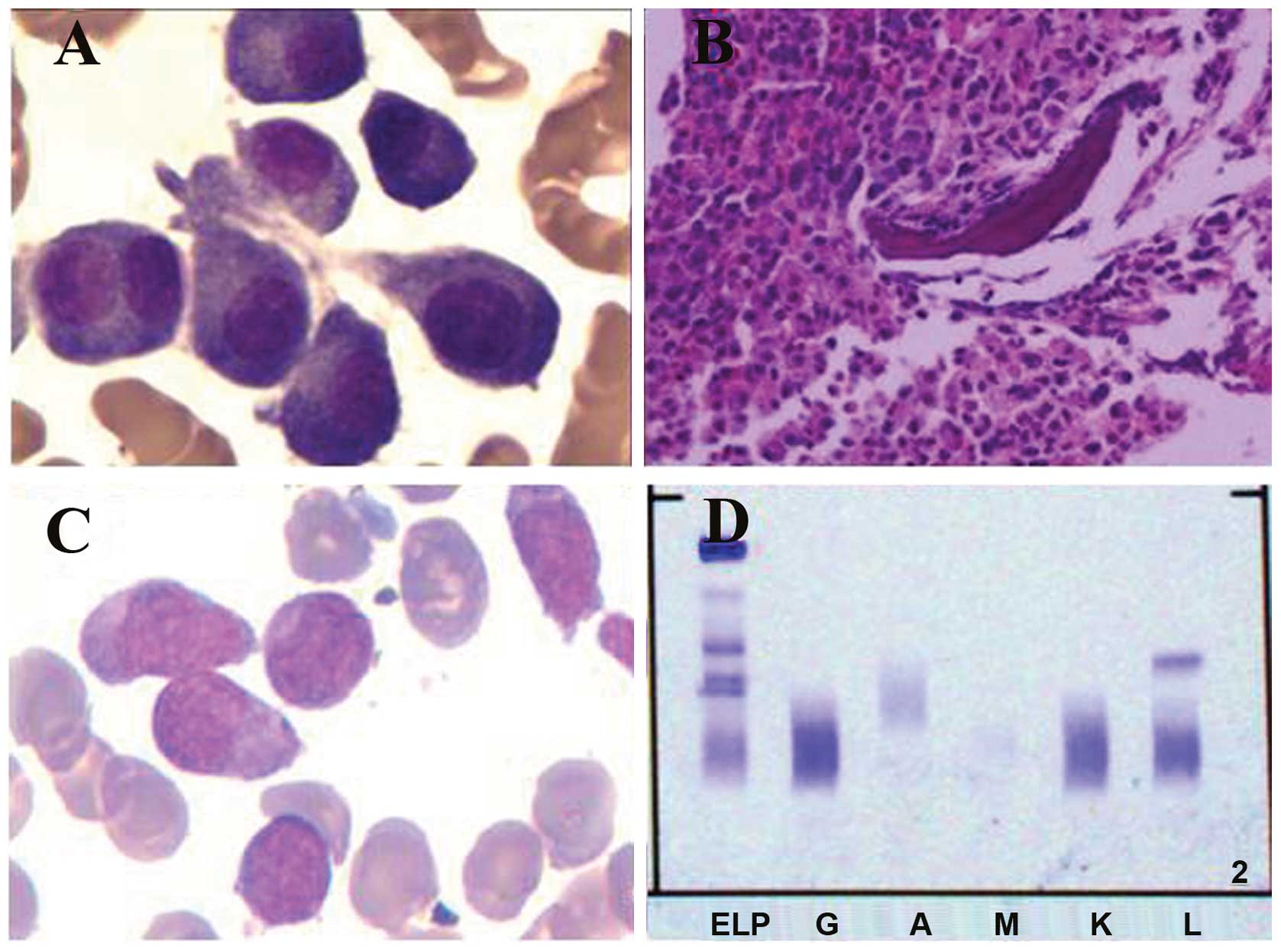 | Figure 1.A bone marrow aspirate and biopsy were
performed. (A) Bone marrow aspirate results showing a cluster of
abnormal plasma cells, including multinucleated plasma cells. (B)
Bone marrow biopsy analysis showing an accumulation of myeloid
cells, dominated by band forms and segmented neutrophils. A number
of clusters of middle-sized cells with abundant cytoplasm were
identified and immunochemistry results were CD38(+), CD138(+) and
epithelial membrane antigen(+/-). (C) Bone marrow smear results
demonstrating hypercellularity, with monoblast cells and
promonocytes accounting for 58% of nucleated cells, indicating that
the patient had progressed to acute monocytic leukemia. (D) Serum
protein immunofixation electrophoresis showing a sharp positive
band for the λ-light chain subtype. CD, cluster of differentiation.
ELP, electrophoresis of protein; G, IgG; A, IgA; M, IgM; K, κ light
chain; L, λ light chain. |
After two years, the patient's bone marrow smear
demonstrated hypercellularity, with monoblast cells and
promonocytes accounting for 58% of nucleated cells, indicating that
the patient had progressed to acute monocytic leukemia, according
to the French-American-British classification criteria (Fig. 1) (7).
The patient achieved CR after one cycle of induction chemotherapy
with the decitabine regimen (15 mg/m2 every day, on days
1–5) combined with low-dose CAG (10 mg/m2 cytarabine,
every 12 h, on days 3–9; 10 mg aclarubicin, on days 3–6; and 200
µg/m2 G-CSF, every day). Each cycle was 1 month.
Subsequent consolidation chemotherapy (cytarabine 2g/m2
twice daily for 3 days) was administered. The patient completed two
cycles in our hospital and refused any other chemotherapy. After
approximately one year, the patient relapsed and succumbed to the
disease soon after.
Discussion
CNL is a rare myeloproliferative neoplasm that is
characterized by persistent leukocytosis consisting of mature
neutrophils, bone marrow granulocytic hyperplasia,
hepatosplenomegaly and the absence of the Philadelphia chromosome
or BCR-ABL fusion gene. The incidence and pathogenesis of CNL
remains unclear. In ≤20% of reported cases, neutrophilia is
associated with an underlying neoplasm, most frequently MM
(6). The coexistence of CNL and MM is
extremely rare and thus, only a small number of cases have been
reported (3,4). However, MM coexisting with other
myeloproliferative neoplasms, including CML (8), polycythemia vera (9), essential thrombocytosis (10) and primary myelofibrosis (11), has been reported, which may indicate
an association between these distinct hematological disorders,
rather than a random simultaneous occurrence.
In total, ∼90% of CNL patients do not exhibit any
cytogenetic abnormalities. In the remaining patients, aberrant
clonal karyotypes may include add(8), add(9), add(21), del(20q),
del(11q) and del(12p) (3). In the
present case, no clonal chromosome abnormalities were identified by
the conventional cytogenetic method. However, clonal abnormalities,
such as del(13q14.3), del(17p13) and add(1q21), were detected by
the FISH technique using MACS to purify MM cells, which confirmed
it as malignant disease.. Standen et al (3) reported two cases of CNL and concurrent
MM, and identified a disproportionate excess of λ-light chain
restriction in those patients. The study also reported that
IgG-λ-type paraprotein and λ-light chains were identified in four
and nine of the 11 previously reported cases of CNL associated with
MM, respectively (4). In CML patients
with concurrent MM, IgG-κ-type monoclonal paraprotein was
predominant in the reported cases (9). In the present case, the patient was
confirmed as λ-type by immunofixation electrophoresis, identical to
the main type (λ-type) of CNL concurrent with MM. The patient
received chemotherapy for MM and disease progression did not occur
for 2 years.
CNL is generally considered as a slowly progressive
disorder (3); however, the survival
of patients is variable, ranging between six months and >20
years. In the present study, the patient developed acute monocytic
leukemia after three years, which indicated a poor prognosis. The
differential diagnosis of chronic myelomonocytic leukemia was
re-evaluated and excluded on the basis of a low monocyte count. The
patient developed MM after the diagnosis of CNL, and succumbed to
blast crisis within two years. Whether MM accelerates this process
remains unclear and thus, the mechanism of this specific disorder
requires further investigation.
The patient presented in this case was 78 years old
and the performance status revealed that intensive chemotherapy was
unsuitable. Hypermethylation, which is an epigenetic mutation that
leads to a decrease in transcription via promoter regions of tumor
suppressor genes causing gene silencing, has been identified as an
important promoter of myeloid leukemogenesis (12). Therefore, demethylating agents are
being investigated to reverse the silencing of critical tumor
suppressor genes. Decitabine is a demethylating agent that
functions as a cytosine analogue. The CAG regimen, which was
originally designed in Japan, rapidly became popularized in China
for the treatment of acute myeloid leukemia and myelodysplastic
syndrome patients due to the relatively mild toxicity exhibited by
the regimen. The CR rate of acute myeloid leukemia patients treated
with the CAG regimen (56.7%) appears to be marginally lower than
the CR rate of patients treated with the standard daunorubicin and
cytarabine regimen (DA; 45 mg/m2 daunorubicin and
100–200 mg/m2 cytarabine; 57–65%) (13). However, no randomized control trial
studies regarding the efficacy of the CAG and DA regimens have been
performed. In the present study, the patient achieved CR following
combined treatment with decitabine and the CAG regimen, which
exhibited a low toxicity when compared with standard
chemotherapy.
In this case, a CNL patient with concurrent MM,
which was confirmed by bone marrow examination, immunofixation
electrophoresis and MRI techniques, was presented. We hypothesize
that the neutrophilia was a neoplasm or secondary to abnormal
cytokine release from the neoplastic plasma cells or other cells
regulated by plasma cells. In this case, CNL was diagnosed prior to
MM, and then it transformed into acute monocytic leukemia,
indicating that the neutrophilia was malignant and a diagnosis of
CNL concurrent with MM was accepted. The occurrence of the two
malignancies in one patient supports the hypothesis that the two
malignancies are derived from hematopoietic progenitor stem cells,
which may differentiate into lymphoplasmacytic or myeloid cell
lines. Treatment with decitabine in combination with the CAG
priming regimen may present a good treatment strategy for elderly
patients with acute myeloid leukemia.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant no. 81000216).
References
|
1
|
Elliott MA: Chronic neutrophilic leukemia:
a contemporary review. Curr Hematol Rep. 3:210–217. 2004.PubMed/NCBI
|
|
2
|
Bird JM, Owen RG, D'Sa S, et al:
Haemato-oncology Task Force of British Committee for Standards in
Haematology (BCSH) and UK Myeloma Forum: Guidelines for the
diagnosis and management of multiple myeloma 2011. Br J Haematol.
154:32–75. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Standen GR, Jasani B, Wagstaff M and
Wardrop CA: Chronic neutrophilic leukemia and multiple myeloma. An
association with lambda light chain expression. Cancer. 66:162–166.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dinçol G, Nalçaci M, Doğan O, Aktan M,
Küçükkaya R, Ağan M and Dinçol K: Coexistence of chronic
neutrophilic leukemia with multiple myeloma. Leuk Lymphoma.
43:649–651. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shen Y, Xue Y, Li J, Pan J and Wu Y:
Clinical, cytogenetic and dual-color FISH studies on five cases of
myelodysplastic syndrome or acute myeloid leukemia patients with
1;7 translocation. Chin Med J (Engl). 116:231–234. 2003.PubMed/NCBI
|
|
6
|
Swerdlow SH, Campo E, Harris NL, Jaffe ES,
Pileri SA, Stein H, et al: WHO Classification of Tumours of
Haematopoietic and Lymphoid Tissues4th. IARC Press; Lyon, France:
2008
|
|
7
|
Bennett JM, Catovsky D, Daniel MT,
Flandrin G, Galton DA, Gralnick HR and Sultan C: Proposals for the
classification of the acute leukaemias. French-American-British
(FAB) co-operative group. Br J Haematol. 33:451–458. 1976.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tanaka M, Kimura R, Matsutani A, Zaitsu K,
Oka Y and Oizumi K: Coexistence of chronic myelogenous leukemia and
multiple myeloma. Case report and review of the literature. Acta
Haematol. 99:221–223. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chang H and Shih LY: Concurrence of
multiple myeloma and idiopathic erythrocytosis. Acta Clin Belg.
64:434–435. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Eskazan AE, Ongoren S, Ar MC, Soysal T,
Ferhanoglu B, Aki H and Aydin Y: Essential thrombocythemia and
multiple myeloma: two rare diseases in one patient. Clin Lymphoma
Myeloma Leuk. 11:442–445. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kawauchi K, Mori H, Sugiyama H, Oshimi K
and Hirayama A: Multiple myeloma with coexistent myelofibrosis:
improvement of myelofibrosis following recovery from multiple
myeloma after treatment with melphalan and prednisolone. Jpn J Med.
30:483–486. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ganetsky A: The role of decitabine for the
treatment of acute myeloid leukemia. Ann Pharmacother.
46:1511–1517. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wei G, Ni W, Chiao JW, Cai Z, Huang H and
Liu D: A meta-analysis of CAG (cytarabine, aclarubicin, G-CSF)
regimen for the treatment of 1029 patients with acute myeloid
leukemia and myelodysplastic syndrome. J Hematol Oncol. 4:462011.
View Article : Google Scholar : PubMed/NCBI
|