Introduction
Hepatocellular carcinoma (HCC) is the fifth most
common cancer and the third highest cause of cancer-related
mortality in the world (1,2). Although hepatic resection or liver
transplantation are the standard methods of treatment for liver
cancer, thermal ablation treatment, including radiofrequency
ablation (RFA), is also widely utilized. Numerous clinical trials
have demonstrated that thermal ablation treatment and curative
resection have similar one and three-year survival rates (95.7 and
74.4% vs. 95.1 and 78.9%, respectively) for tumors <5 cm in
diameter (3,4). Although it is a minimally invasive
treatment, thermal ablation may cause a number of common clinical
complications, including pain, fever, bowel injury, abdominal
bleeding, bile duct injury, liver abscess and implantation
metastasis of tumor cells (5). In
addition, rare complications may occur post-RFA, leading to more
serious consequences, such as intrahepatic infection, hemorrhage or
mortality. To the best of our knowledge, no cases of hepatic
abscess with hepatobronchial fistula post-RFA have been reported.
The current case report describes a rare complication of an hepatic
abscess, involving invasion of the lung via the diaphragm, leading
to hepatobronchial fistula following hepatic RFA. Despite treatment
through drainage and anti-infection medication, the patient
succumbed to respiratory failure. This report aims to discuss the
prevention and treatment of complications, and explore the
indications and contraindications of thermal ablation. Written
informed consent was obtained from the patient's family.
Case report
A 65-year-old male with a 20-year history of
hepatitis B and a five-year history of liver cirrhosis was admitted
to Renji Hospital (Shanghai, China) in December 2010, and
subsequently diagnosed with hepatocellular carcinoma (HCC) located
in segment II-III of the hepatic left lateral lobe. Five days
following admission, a hepatic resection was successfully
performed. The patient received regular postoperative follow-up
examinations, however, one year later due to tumor recurrence, the
patient was treated with three hepatic cycles of RFA. On July 31,
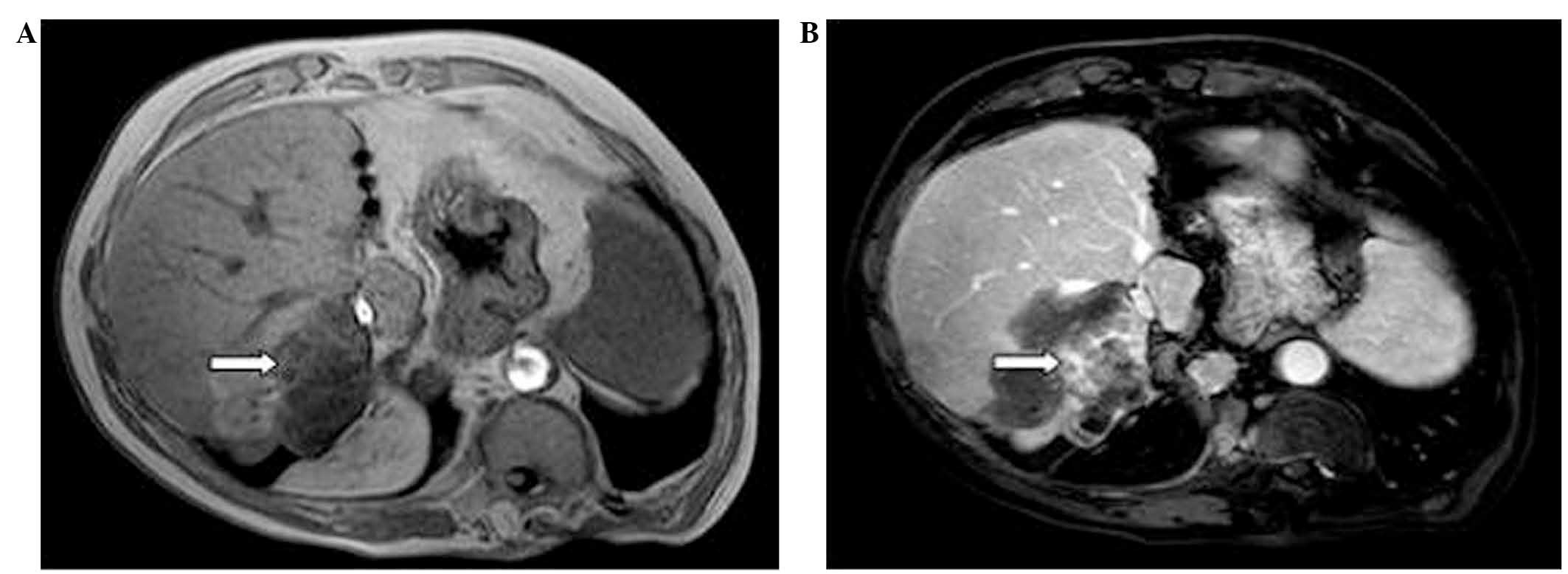
2012, magnetic resonance imaging during a follow-up visit revealed
a tumor measuring 5.5×3.5 cm in the right posterior hepatic lobe
(Fig. 1). Due to the large size of
the tumor, transarterial chemoembolization (TACE) was conducted. As
this treatment did not produce a satisfactory outcome, percutaneous
RFA was performed successfully under ultrasonographic guidance on
August 10, 2012. Anti-inflammatory (0.5 g intravenous imipenem,
every 8 h), hepatoprotective (500 mg intravenous
s-adenosylmethionine, once a day) and symptomatic treatments
(electrolyte and 10 g albumin supplements) were also administered.
The patient was discharged three days following RFA; however, after
a further two days, the patient was admitted to the emergency room
due to a sudden occurrence of hematemesis and unconsciousness,
which lasted for 1 h. Physical examination revealed that the
patient's blood pressure was 90/60 mmHg (normal range, 90–120/50–80
mmHg) and heart rate was 160 beats/min (normal range, 60–100
beats/min); therefore hemorrhagic shock was suspected. Following
hemostasis, electrolyte replacement and rehydration, and the
administration of hepatoprotective and other symptomatic
treatments, including parenteral nutrition, the patient stabilized
with blood pressure of 110/70 mmHg and a heart rate of 100
beats/min. After a further one day, the patient developed a high
fever (39.6°C) with chills and complained of physical weakness.
Laboratory test results revealed a white blood cell count of
14.75×109/l (normal range, 3.70–9.20×109/l),
red blood cell count of 3.48×1012/l (normal
range,3.68–5.74×1012/l), platelet count of
75×109/l (normal range, 85–320×109/l), and a
hemoglobin level of 103 g/l (normal range, 113–172 g/l). Biliary
retrograde infection of the hepatic ablation zone was suspected due
to the accumulation of gas in this region, observed on B-ultrasound
examination. The patient's condition improved following the
application of third-generation cephalosporin antibiotics,
nutritional support, hepatoprotective treatment and other
symptomatic treatments, such as rectal administration of 18.75 mg
indomethacin, once a day. On post-operative day 17, the patient
experienced sudden right upper quadrant abdominal pain that
radiated to the back, concurrent with dyspnea and a cough. A
physical examination revealed deep abdominal tenderness without
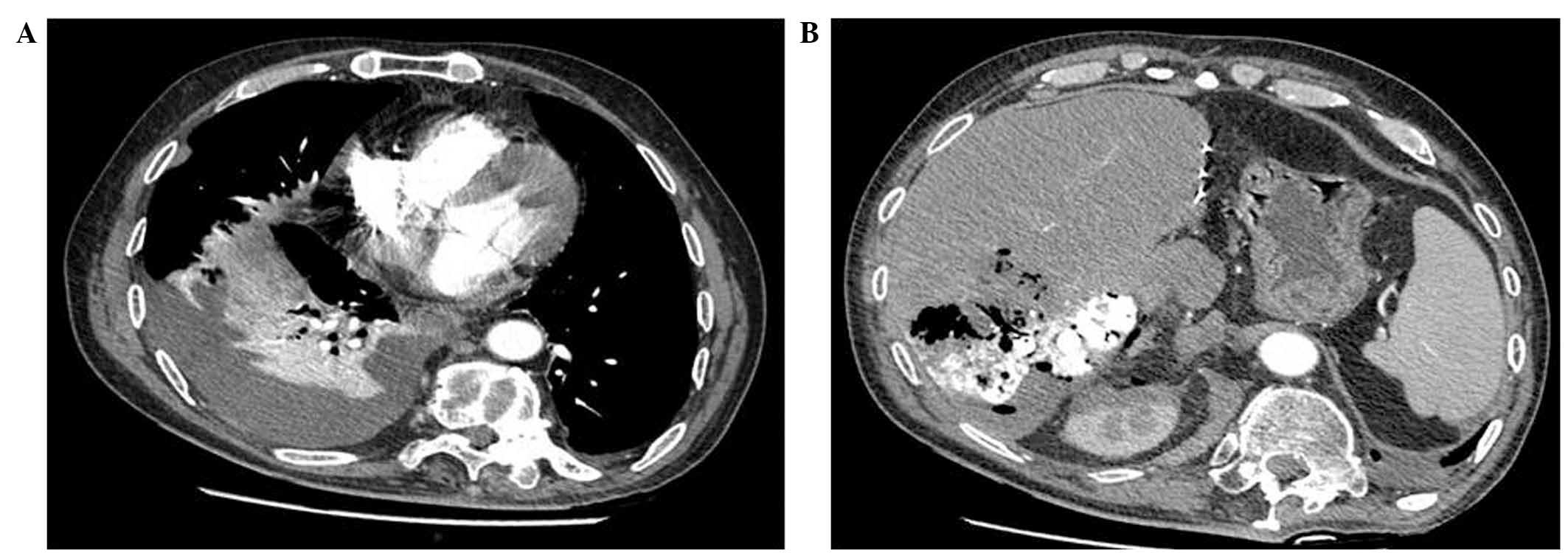
rebound pain. Computed tomography (CT) imaging of the lungs and
abdomen revealed lower right pulmonary atelectasis and pleural
effusion connected to the hepatic abscess (Fig. 2). Pleural fluid culture did not detect
bacteria. Following treatment with anti-inflammatory drugs and
thoracic cavity drainage, the patient's abdominal pain improved;
however, the dyspnea was not relieved. On post-operative day 20,
the patient complained of a worsened cough accompanied by thin
yellow sputum which was bitter in taste and was suspected to
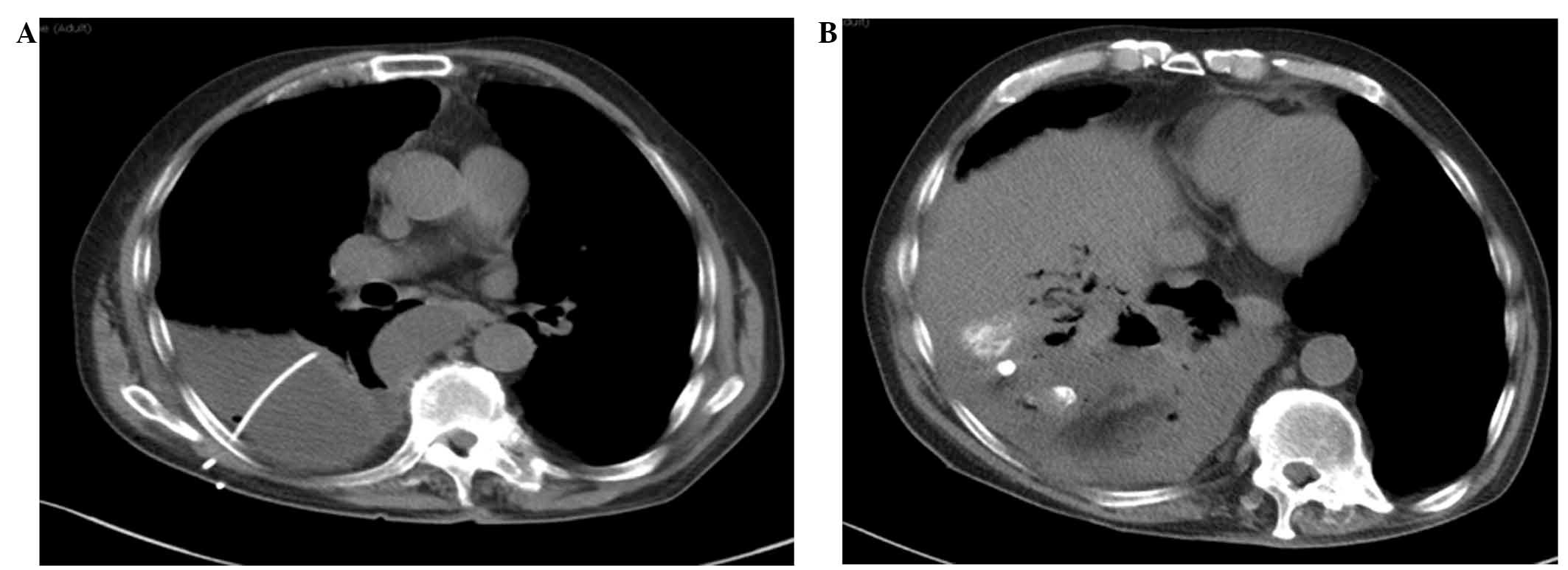
contain bile. Re-examination of the lungs by CT indicated that
effusion was still present on the right lung field, and the hepatic
abscess contained gas and had expanded, obscuring the boundary
between the liver and the lung (Fig.
3). The patient exhibited shortness of breath and oxygen
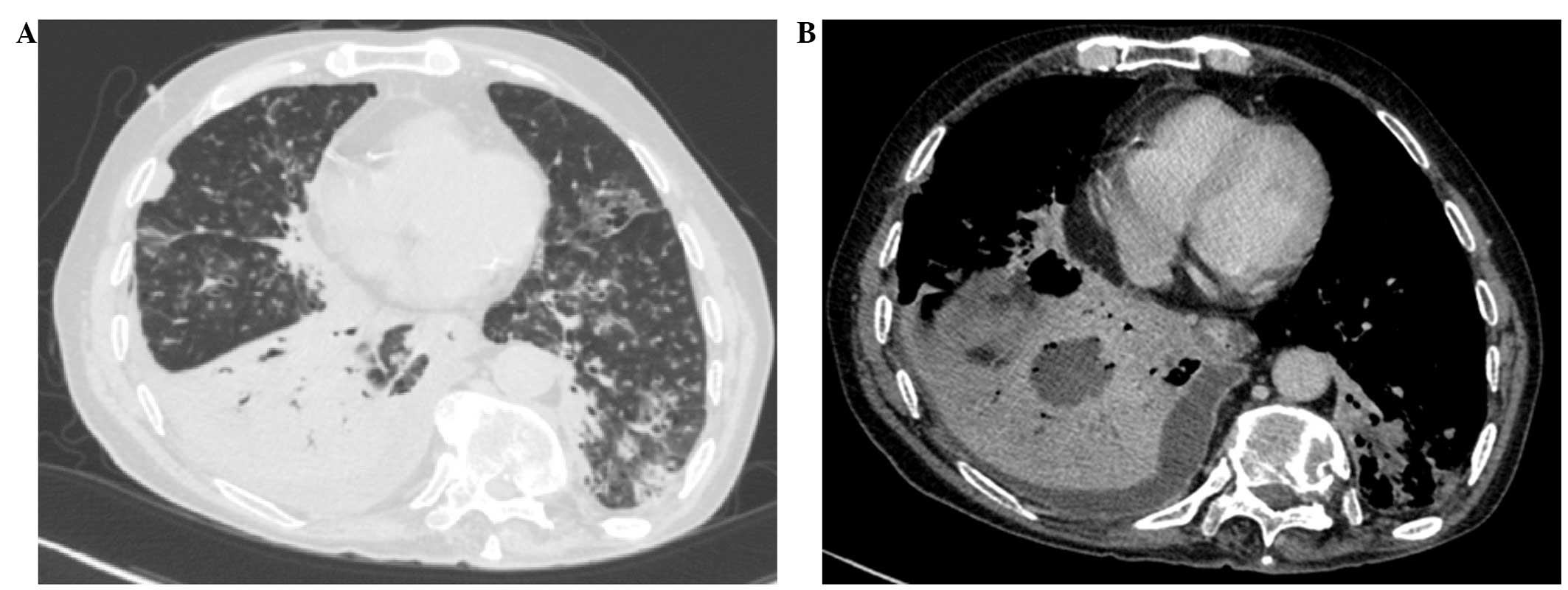
desaturation despite symptomatic treatments. CT imaging of the
chest and abdomen indicated atelectasis in the right lower lung
field, bilateral bronchiectasis in the lower lung fields, bacterial
(E. coli) lung infection and a fluid-filled space connected to the
intrahepatic focal ablation (Fig. 4).
The clinical symptoms and CT scan indicated a diagnosis of hepatic
abscess with hepatobronchial fistula, a rare complication of RFA,
which was caused by the invasion of intrahepatic infection and bile
leakage one month following RFA. Despite treatment with
anti-inflammatory drugs (third-generation cephalosporins) and
thoracic cavity drainage, the patient succumbed to respiratory
failure one day after treatment.
Discussion
Hepatocellular carcinoma, which often occurs with
liver cirrhosis, is a common primary liver tumor worldwide
(6). With the advancement of medical
techniques, a great variety of HCC treatments have been developed.
Optimal treatment must be selected according to the individual
conditions. RFA is one of the most widely used local ablative
therapies for small HCC (<5 cm in diameter), with an efficacy
that is comparable to surgical resection (7,8). The
criteria used to determine RFA suitability in cases of HCC include
the following: A single nodule <5 cm in size, or ≤3 nodules each
<3 cm in size; Child-Pugh class A or B; and the absence of
portal vein thrombosis or extrahepatic metastases (4). Compared with hepatic resection, RFA has
many advantages: i) It is minimally invasive with low risk; ii) it
enables excellent local tumor control; iii) it is associated with
rapid recovery and promising five-year survival rates; iv) it is a
multimodal approach (9). However, RFA
may cause certain complications, including peritoneal hemorrhage,
bile duct injury, bowel perforation, liver abscess and cancer
seeding along the electrode tract, liver infarction, diaphragmatic
perforation and hernia (9–12). Hepatic abscess with hepatobronchial
fistula is an extremely rare complication resulting from hepatic
RFA for the treatment of HCC.
In the current case, the patient's condition was
poor due to multiple surgeries, and the hepatic tumor was large and
tightly adjacent to the porta hepatis; this allowed necrotic
tissues resulting from RFA to invade the small bile duct, which
contributed to secondary infection. In the early stages of the
tumor, if percutaneous drainage is unable to drain the necrotic
tissues due to a lack of tumor tissue liquefaction, antibiotics are
the only remaining strategy that may be used to control infection
(13). If antibiotic therapy is
ineffective, the intrahepatic infection is able to spread and may
cause bacteremia (14). In the
present case, the diaphragm and adjacent organs were easily invaded
by the intrahepatic infectious focus close to the diaphragm. RFA
damaged the bile ducts, leading to intrahepatic infection caused by
leakage of bile to the hepatic abscess, and subsequently, the
invasion of the diaphragm and right lung by the intrahepatic
infection and bile. Due to the continual erosion by the
intrahepatic infection, the lung infection could not be controlled,
resulting in mortality due to the respiratory failure. Therefore,
patients who have undergone RFA treatment, particularly those with
large tumors, must be carefully monitored in order to prevent
intrahepatic infection. Once infection is detected, anti-infective
agents must be administered and drainage of the liver abscess must
be performed immediately.
The present case demonstrates the importance of CT
imaging of the chest, abdomen and pelvis following RFA, to detect
possible thermal injuries beyond the liver. The patient's
diaphragmatic defect was not formed during RFA treatment (data not
shown); the hepatic abscess with hepatobronchial fistula formation
primarily resulted from intrahepatic infection. The infection and
bile penetrated the diaphragm causing bacterial and chemical
erosion of the bronchus. In this case, medical and surgical methods
were unable to eliminate the infection, which invaded the diaphragm
and caused uncontrollable pulmonary infection. In such conditions,
prognosis is typically poor, and the rapid prevention and/or
treatment of the infection is essential. For the prevention or
minimization of intraoperative and postoperative complications, the
following recommendations must be considered: i) For patients whose
tumor location is complicated, particularly if close to the porta
hepatis, RFA must be performed under laparoscopy or by
pneumoperitoneum and the appropriate RFA electrodes and frequency
must be selected to avoid overheating, which may cause damage to
adjacent tissues and organs (15);
ii) for patients with large tumors, depending on the patient
condition, preoperative TACE/TAE may be performed to reduce the
tumor volume prior to RFA treatment (13); iii) during and following the surgery,
surgeons must carefully monitor the patient's vital signs.
The current case report describes a case of hepatic
abscess with hepatobronchial fistula, occurring five days following
hepatic RFA. To the best of our knowledge, no other reports of this
condition have been published. The unfavorable outcome of the
present case demonstrates that, although RFA is a minimally
invasive and effective method to treat liver cancer, the
indications of RFA, such as early tumor stage and small tumor size,
must be precisely determined, and careful monitoring for potential
postoperative complications that may lead to mortality must be
conducted. This is essential to improve the success rate of
RFA.
Acknowledgements
This study was supported by a grant from sTNFr-13
horizontal subject (no. 101005.335) to Jianjun Zhang.
References
|
1
|
Lau WY, Leung TW, Yu SC and Ho SK:
Percutaneous local ablative therapy for hepatocellular carcinoma: a
review and look into the future. Ann Surg. 237:171–179. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Livraghi T, Mäkisalo H and Line PD:
Treatment options in hepatocellular carcinoma today. Scand J Surg.
100:22–29. 2011.PubMed/NCBI
|
|
3
|
Tombesi P, Di Vece F and Sartori S:
Resection vs thermal ablation of small hepatocellular carcinoma:
What's the first choice? World J Radiol. 5:1–4. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Baldan A, Marino D, DE Giorgio M, et al:
Gene - Gruppo Epatocarcinoma NORD-EST: Percutaneous radiofrequency
thermal ablation for hepatocellular carcinoma. Aliment Pharmacol
Ther. 24:1495–1501. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Howenstein MJ and Sato KT: Complications
of radiofrequency ablation of hepatic, pulmonary, and renal
neoplasms. Semin Intervent Radiol. 27:285–295. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shirai K, Tamai H, Shingaki N, et al:
Clinical features and risk factors of extrahepatic seeding after
percutaneous radiofrequency ablation for hepatocellular carcinoma.
Hepatol Res. 41:738–745. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Khan MR, Poon RT, Ng KK, et al: Comparison
of percutaneous and surgical approaches for radiofrequency ablation
of small and medium hepatocellular carcinoma. Arch Surg.
142:1136–1143. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Guglielmi A, Ruzzenente A, Valdegamberi A,
Pachera S, et al: Radiofrequency ablation versus surgical resection
for the treatment of hepatocellular carcinoma in cirrhosis. J
Gastrointest Surg. 12:192–198. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rhim H and Lim HK: Radiofrequency ablation
of hepatocellular carcinoma: pros and cons. Gut Liver. 4:S113–S118.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chiu YC, Chuang CH, Tsai HM and Chen CY:
Massive hepatic infarction after pure ethanol injection and
radiofrequency ablation therapy for hepatocellular carcinoma: a
case report. Kaohsiung J Med Sci. 25:156–159. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhou M, He H, Cai H, et al: Diaphragmatic
perforation with colonic herniation due to hepatic radiofrequency
ablation: A case report and review of the literature. Oncol Lett.
6:1719–1722. 2013.PubMed/NCBI
|
|
12
|
Ke S, Ding XM, Qian XJ, et al:
Radiofrequency ablation of hepatocellular carcinoma sized < 3
and ≤ 5 cm: is ablative margin of more than 1 cm justified? World J
Gastroenterol. 19:7389–7398. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang Z, Zhuang Z, Xu Z, et al:
Post-operative pericardial effusion following treatment of small
hepatocellular carcinoma with radiofrequency ablation: a case
report. Oncol Lett. 7:345–348. 2014.PubMed/NCBI
|
|
14
|
Thiemann M, Benhidjeb T, Anders S, et al:
Hepato-pericardial fistula following radiofrequency ablation (RFA)
for liver metastasis: a case report and review of the literature.
Langenbecks Arch Surg. 393:1013–1016. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wood TF, Rose DM, Chung M, et al:
Radiofrequency ablation of 231 unresectable hepatic tumors:
indications, limitations, and complications. Ann Surg Oncol.
7:593–600. 2000. View Article : Google Scholar : PubMed/NCBI
|