Introduction
Neuroblastoma is the most common extracranial solid
tumor to occur during childhood. The cancer arises in the
sympathetic nervous system and mainly affects the adrenal glands
and retroperitoneum, with a distribution pattern that is similar in
children and adults. In total, >90% of the tumors are diagnosed
in children <10 years old (1). The
incidence in those >20 years old has been reported to be only
0.12 cases/1 million individuals (2).
Renal neuroblastomas are extremely uncommon, particularly in
adults. To the best of our knowledge, to date only one case of
adult intrarenal neuroblastoma has been reported in the literature
(3). The number of studies on the
pathogenesis, biological characteristics, treatment and prognosis
of the cancer have been limited due to this low incidence. The
present study reports a case of left renal neuroblastoma in an
adult patient with multiple bone and joint metastases, and
discusses its clinical manifestations, diagnosis and treatment.
Written informed consent was obtained from the patient's
family.
Case report
In December 2013, a 22-year-old female was admitted
to the Affiliated Hospital of Guangdong Medical College (Zhanjiang,
China)with abdominal and joint pain that had been present for
>10 days. There was no significant medical history. The patient
had experienced no fever, chills, diarrhea, nausea, vomiting or
hematuria. A physical examination revealed that the abduction,
internal rotation and extension of the left shoulder and hip were
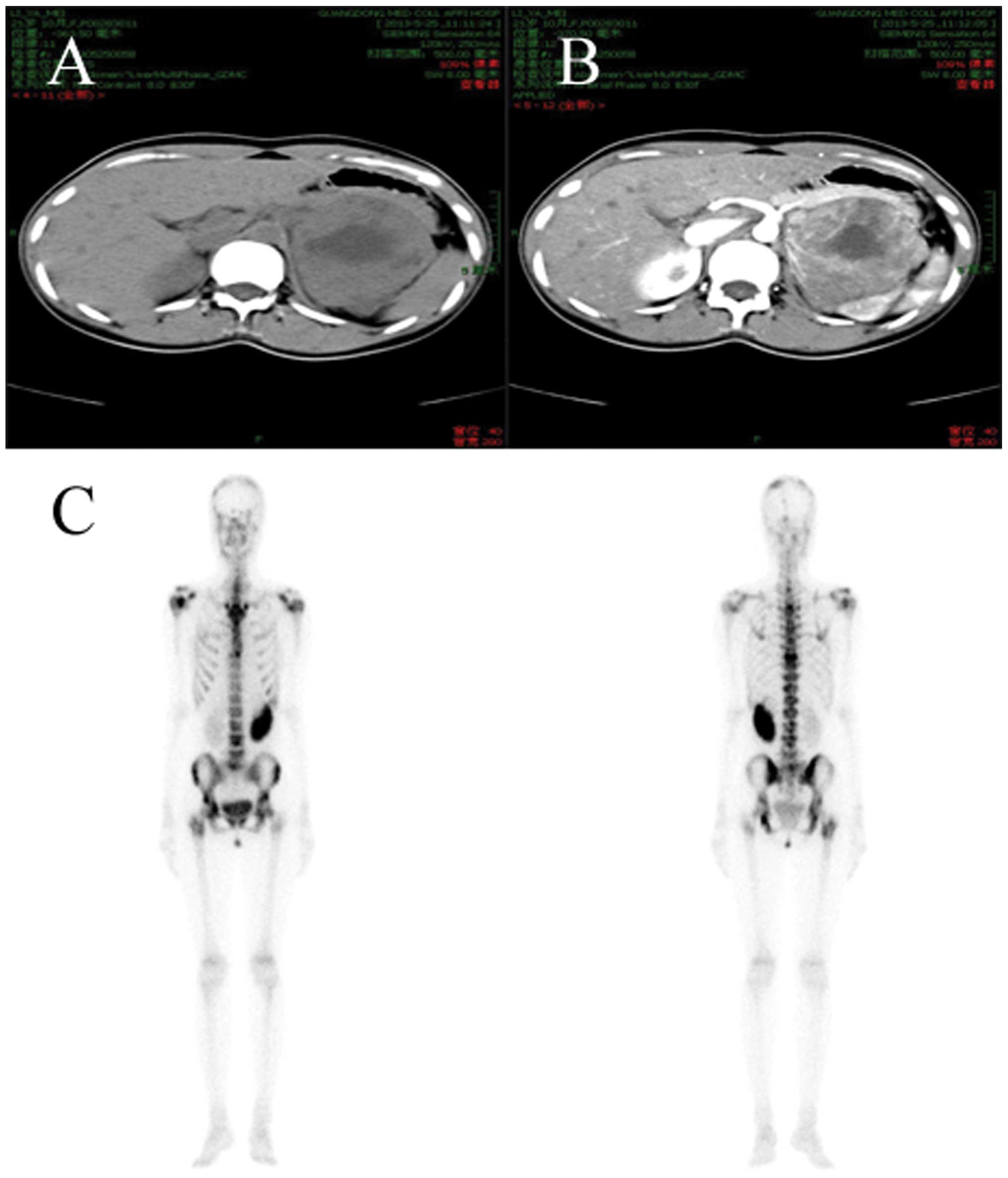
limited. Computed tomography (CT) of the abdomen and pelvis showed
a large heterogeneous and centrally necrotic mass, measuring
8.2×7.3×3.1 cm, in the upper pole of the left kidney (Fig. 1A and B). A number of retroperitoneal
lymph node shadows were apparent, along with multiple small,
low-density lesions in the lumbar region. Round low-density nodules
were also present in the liver. Additionally, the bone scan showed
multiple bone and joint metastases (Fig.
1C).
The patient underwent a left nephroureterectomy and
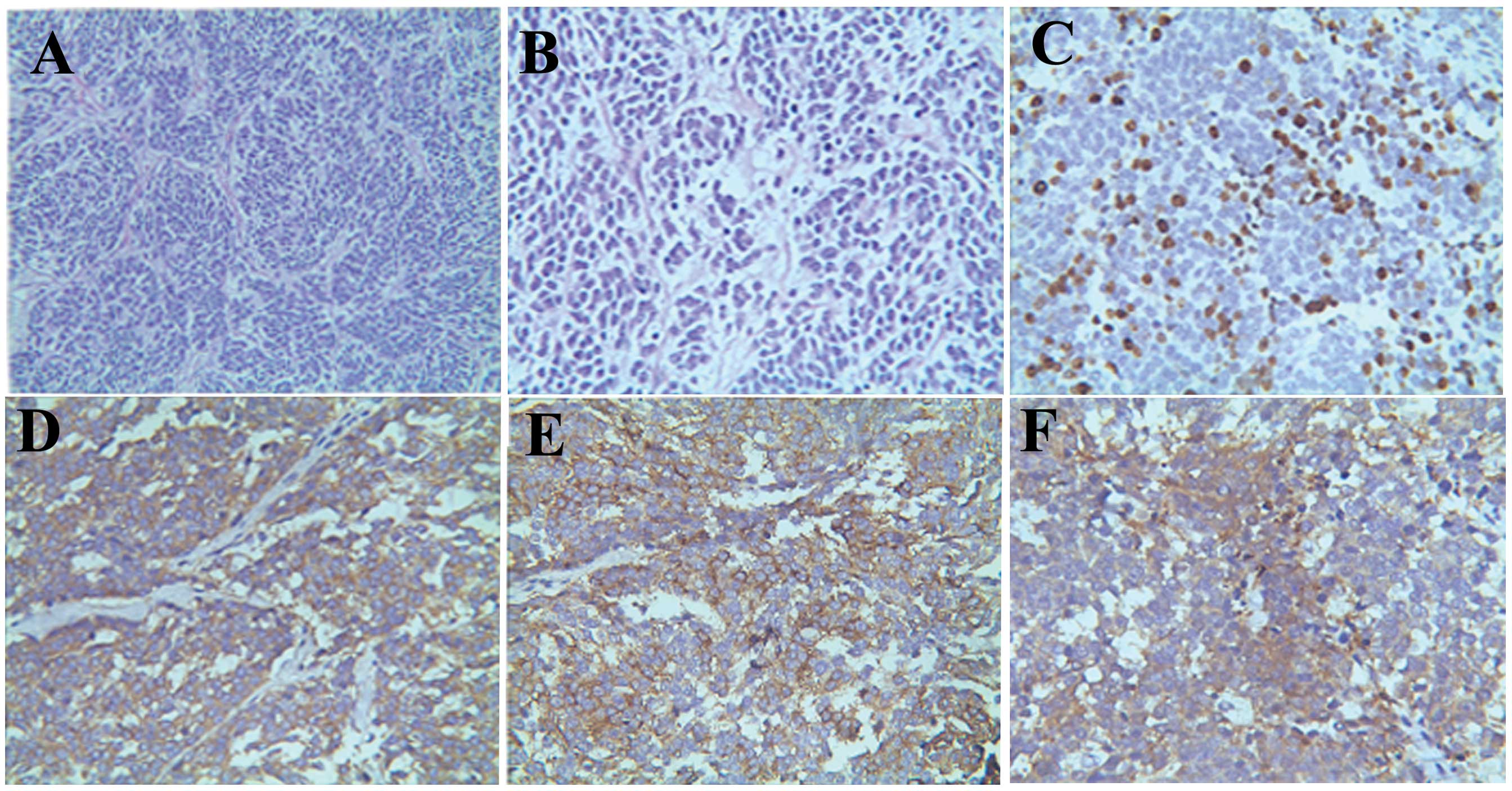
ipsilateral lymph node dissection. Pathological examination showed
that the cells contained small, uniform, hyperchromatic nuclei,
with coarse chromatin. Occasional larger ganglion-like cells were
present and focal anaplasia was also evident. The tumor cells
stained strongly for chromogranin, synaptophysin, neuron-specific
enolase, cluster of differentiation (CD)56 and vimentin, with a
positive Ki-67 expression rate of ~20%. Focal dot negativity was
exhibited for cytokeratin. Staining for epithelial membrane
antigen, CK, leucocyte common antigen, S-100, CD10 and CD99 was
negative in the renal tumor cells. These findings are consistent
with renal neuroblastoma (Fig. 2).
Post-operative radiotherapy (40 Gy) was administered for four weeks
and the pain in the joints and abdomen consequently disappeared.
The patient was discharged 60 days after admittance. At the
nine-month follow-up examination, the patient showed no evidence of
recurrence, progression or metastatic disease on CT scans of the
chest, abdomen and pelvis.
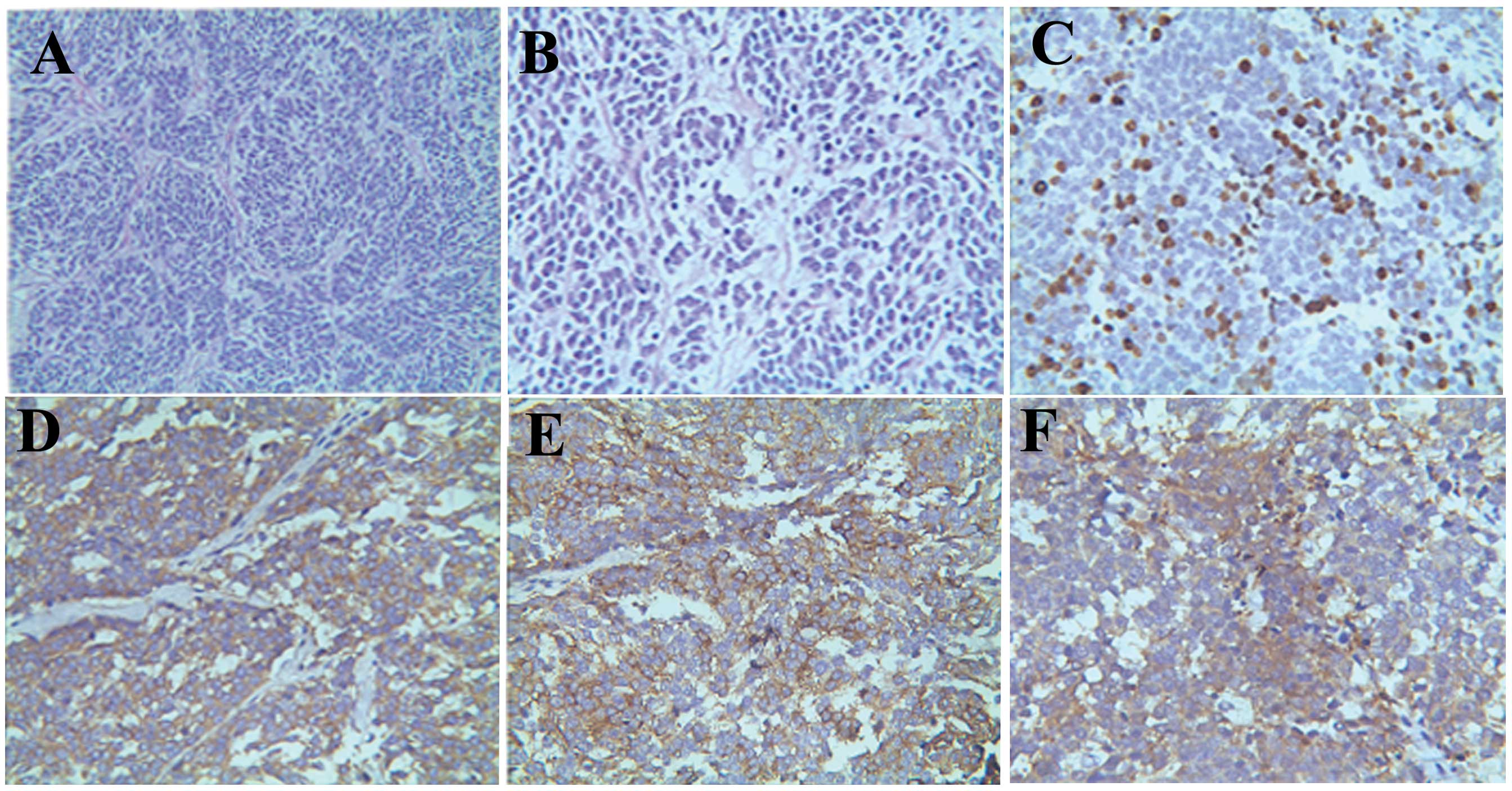 | Figure 2.Pathological examination showed (A)
cells containing small, uniform, hyperchromatic nuclei, with coarse
chromatin (hematoxylin staining; original magnification, x200). (B)
Occasional larger ganglion-like cells were present and focal
anaplasia was also evident (hematoxylin staining; original
magnification, x400). The tumor cells were strongly stained for (C)
Ki-67 (original magnification, x400), (D) synaptophysin (original
magnification, x400), (E) chromogranin (original magnification,
x400) and (F) neuron-specific enolase (original magnification,
x400). |
Discussion
Neuroblastoma is the second most prevalent solid
pediatric malignancy, with >90% of tumors diagnosed in children
<10 years old (1). To the best of
our knowledge, the youngest recorded patient with a neuroblastoma
was 30 weeks old (4) and the oldest
patient was 79 years old (5). A
recent study found that the incident rate of neuroblastoma (80 per
1 million individuals) ranked first highest and that the 5-year
survival rate (93.4%) was ranked third highest, amongst all types
of cancer in the 309 cases of diagnosed cancer between 1998 and
2007 (6). Studies on the
pathogenesis, biological characteristics, treatment and prognosis
of renal neuroblastoma have been limited due to the low incidence
of the cancer. At present, the pathogenesis of neuroblastoma
remains extremely unclear. The pathogenesis of neuroblastoma may be
associated with ALK, PTPN11, ATRX, MYCN, NRAS, CHEK2, PINK1 and
BARD1 (7).
According to the current literature (8), the diagnosis of neuroblastoma depends
mainly on ultrasound, CT, magnetic resonance imaging,
post-operative pathology and fine-needle aspiration (FNA) cytology.
For example, Serrano et al (9)
diagnosed two primary renal neuroblastomas by CT-guided FNA
cytology in a 6-year-old male and a 7-month-old male, thus
demonstrating the usefulness of CT-guided FNA in diagnosing renal
neuroblastoma. The treatment modalities for this cancer are
surgery, surgery plus chemotherapy and surgery plus radiotherapy. A
previous study has shown that 177Lu-DOTATATE could be
used to treat children with relapsed or primary refractory
high-risk neuroblastoma, and no significant renal toxicity has yet
been observed (10). Due to the lack
of specific treatment programs, clinicians do not have clear
treatment guidelines to refer to and thus, they treated this
patient according to pediatric guidelines. Tiu et al
(5) presented one case of kidney
neuroblastoma with unfavorable histological features that was
treated with surgery alone. Long-term post-operative follow-up was
also performed, which revealed no evidence to indicate recurrence.
Bayrak et al (3) also reported
one case in which a patient with stage I intrarenal neuroblastoma
did not receive adjuvant therapy post-operatively; this patient
also showed no evidence of recurrent residual disease at 30 months
post-surgery. There is currently no evidence to show the difference
between adjuvant chemotherapy and radiotherapy with regard to
improving survival times and reducing recurrence. Gohji et
al (11) reported two cases of
kidney neuroblastoma in two adult cases; one patient was treated
with post-operative cobalt therapy and the other was treated with
post-operative adjuvant chemotherapy. Upon comparison, no
difference in tumor recurrence was found after a follow-up time of
five years. Moreno et al (12)
analyzed a large number of high-risk neuroblastoma survivors from a
multi-institutional randomized trial that included the use of
induction chemotherapy, surgery for the primary tumor and high-dose
melphalan, with stem cell rescue. The study found no differences in
the late toxicities between treatment arms for a median follow-up
period of 12.9 years (range, 6.9–16.5 years). The literature shows
no difference in the recurrence and late toxicities of
post-operative adjuvant treatment. Perwein et al (13) found a five-year overall survival rate
[mean ± standard deviation (SD)] of 54.3±9% and a five-year
event-free survival rate (mean ± SD) of 44.9±9% amongst 31 patients
with stage IV neuroblastoma treated between 1984 and 2009. There
was, however, a high incidence of severe long-term sequelae in the
hepatobiliary, musculoskeletal and pulmonary systems, as well as
unilateral blindness and secondary neurological neoplasms.
In the present study, CT of the abdomen and pelvis
was used to locate the renal mass, while the bone scan showed
multiple bone and joint metastases. The patient subsequently
underwent a radical left nephroureterectomy and ipsilateral lymph
node dissection. The post-operative pathology confirmed a diagnosis
of renal neuroblastoma. The patient was also treated with
post-operative radiotherapy, and nine months of follow-up revealed
no significant side-effects or recurrence. For more detailed data,
such as the five-year survival rate and the presence of any future
recurrence, a longer follow-up is required.
In conclusion, renal neuroblastoma is extremely
uncommon in adults, and its diagnosis and treatment is complicated
by this low incidence, the lack of specific treatment guidelines,
the advanced disease state due to late presentation, and its
associated co-morbidities. Further study is required on the
pathogenesis, biological and clinical characteristics, and
treatment of renal neuroblastoma in order to provide an optimal
treatment and to improve the patient's quality of life.
References
|
1
|
Franks LM, Bollen A, Seeger RC, et al:
Neuroblastoma in adults and adolescents: an indolent course with
poor survival. Cancer. 79:2028–2035. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Esiashvili N, Goodman M, Ward K, et al:
Neuroblastoma in adults: incidence and survival analysis based on
SEER data. Pediatric Blood Cancer. 49:41–46. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bayrak O, Seckiner I, Erturhan S, et al:
Adult intrarenal neuroblastoma presenting as renal cell carcinoma.
Can Urol Assoc J. 6:E144–E146. 2012.PubMed/NCBI
|
|
4
|
Garnier S, Maillet O, Haouy S, et al:
Prenatal intrarenal neuroblastoma mimicking a mesoblastic nephroma:
a case report. J Pediatr Surg. 47:e21–e23. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tiu A, Latif E, Yau L, et al: Primary
renal neuroblastoma in adults. Urology. 82:11–13. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rabinowicz R, Barchana M, Liphshiz I, et
al: Cancer incidence and survival among infants in Israel,
1998–2007. Pediatr Hematol Oncol. 30:646–654. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pugh TJ, Morozova O, Attiyeh EF, et al:
The genetic landscape of high-risk neuroblastoma. Nat Genet.
45:279–284. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Polishchuk AL, Dubois SG, Haas-Kogan D, et
al: Response, survival and toxicity after
iodine-131-metaiodobenzylguanidine therapy for neuroblastoma in
pre-adolescents, adolescents and adults. Cancer. 117:4286–4293.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Serrano R, Rodriguez-Peralto JL, De Orbe
GG, et al: Intrarenal neuroblastoma diagnosed by fine-needle
aspiration: a report of two cases. Diagn Cytopathol. 27:294–297.
2002. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gains JE, Bomanji JB, Fersht NL, et al:
177Lu-DOTATATE molecular radiotherapy for childhood neuroblastoma.
J Nucl Med. 52:1041–1047. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gohji K, Nakanishi T, Hara I, et al: Two
cases of primary neuroblastoma of the kidney in adults. J Urol.
137:966–968. 1987.PubMed/NCBI
|
|
12
|
Moreno L, Vaidya SJ, Pinkerton CR, et al:
European neuroblastoma study group; Children's Cancer and Leukaemia
Group (CCLG) (formerly UKCCSG): Long-term follow-up of children
with high-risk neuroblastoma: the ENSG5 trial experience. Pediatr
Blood Cancer. 60:1135–1140. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Perwein T, Lackner H, Sovinz P, et al:
Survival and late effects in children with stage 4 neuroblastoma.
Pediatr Blood Cancer. 57:629–635. 2011. View Article : Google Scholar : PubMed/NCBI
|