Introduction
Actinomycosis is a rare, chronic and indolent
progressive granulomatous infection that is typically caused by the
bacteria, Actinomyces israelii (1–3).
Classically, actinomycosis presents in three clinical forms:
Cervicofacial, thoracic and abdominopelvic (1,2).
Cervicofacial actinomycosis accounts for around 60% of cases, with
the mandible being the most frequently affected anatomic site
(1–3).
Though the clinical manifestations vary, an abscess formation with
subsequent draining sinus and fistula formation is most commonly
observed (1–3). An adequate course of antibiotics is the
cornerstone of treatment (1–3). Surgical debridement is necessary in
certain circumstances (1). The
prognosis is positive, providing that early diagnosis and treatment
occurs (3). Sustained observation is
mandatory for detection of recurrence. Occurrence of nasopharyngeal
actinomycosis is rare, and infection can occur without prior
mucosal injury or an immunocompromised status (1). Therefore, it is advisable to always
maintain a high level of clinical suspicion when treating patients
with a persistent nasopharyngeal mass that presents with vague
symptoms. The present study described a case of this rare disease
entity. The clinical course, microbiologic findings and images were
also presented.
Case report
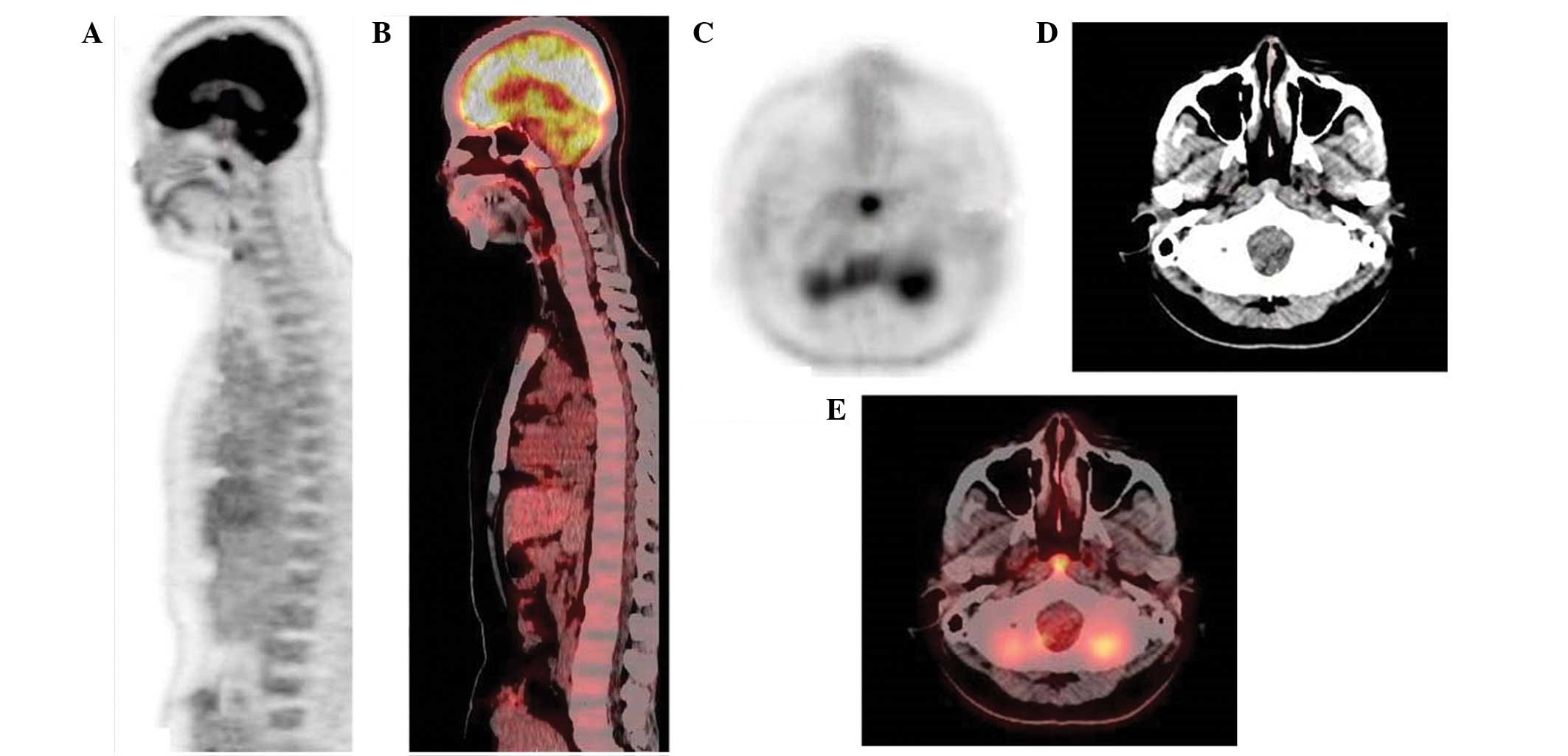
An otherwise healthy 46-year-old Asian female
underwent a 18F-fluorodeoxyglucose (18F-FDG)
positron emission tomography (PET)/computed tomography (CT)
whole-body cancer screening at the Kaohsiung Veterans General
Hospital (Kaohsiung, Taiwan). Intense, focal 18F-FDG
uptake (standard uptake value, 6.2) was identified over the
nasopharynx (Fig. 1). The patient was
transferred to the otolaryngology outpatient department following a
suspected nasopharyngeal malignancy in March 2013. A detailed
history identified no other symptoms affecting the four general
areas of compliant: aural, nasal, neck, or miscellaneous accounted
for by cranial nerve involvement. In addition, the medical history
of the patient, in relation to maxillofacial trauma or dental
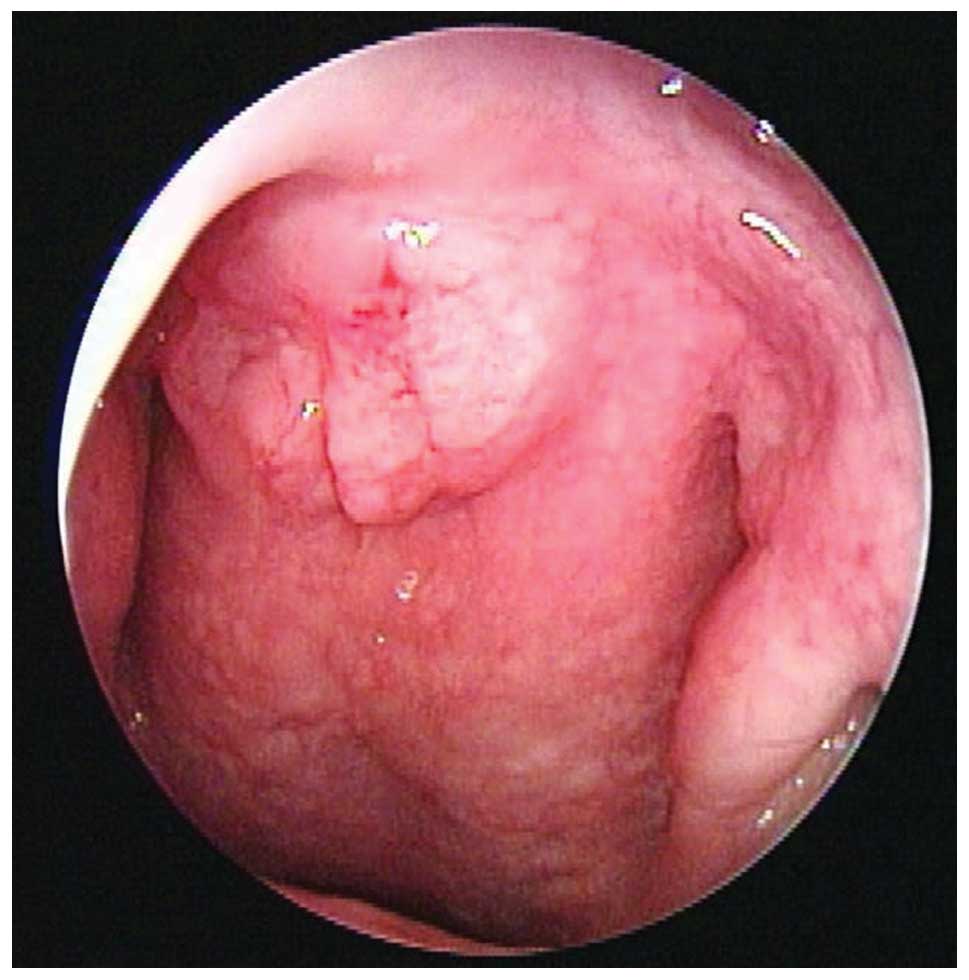
manipulation, was unremarkable. Direct nasopharyngoscopy with a
rigid telescope revealed an unclearly demarcated granular mass
originating from the roof of the nasopharynx (Fig. 2). A biopsy was performed and a sample
of the fluid from the mass was sent for comprehensive microbiology
and pathology analysis. The results revealed that the sample
contained Gram-positive filamentous rods, but was negative for
acid-fast staining. Despite this, the culture medium failed to grow
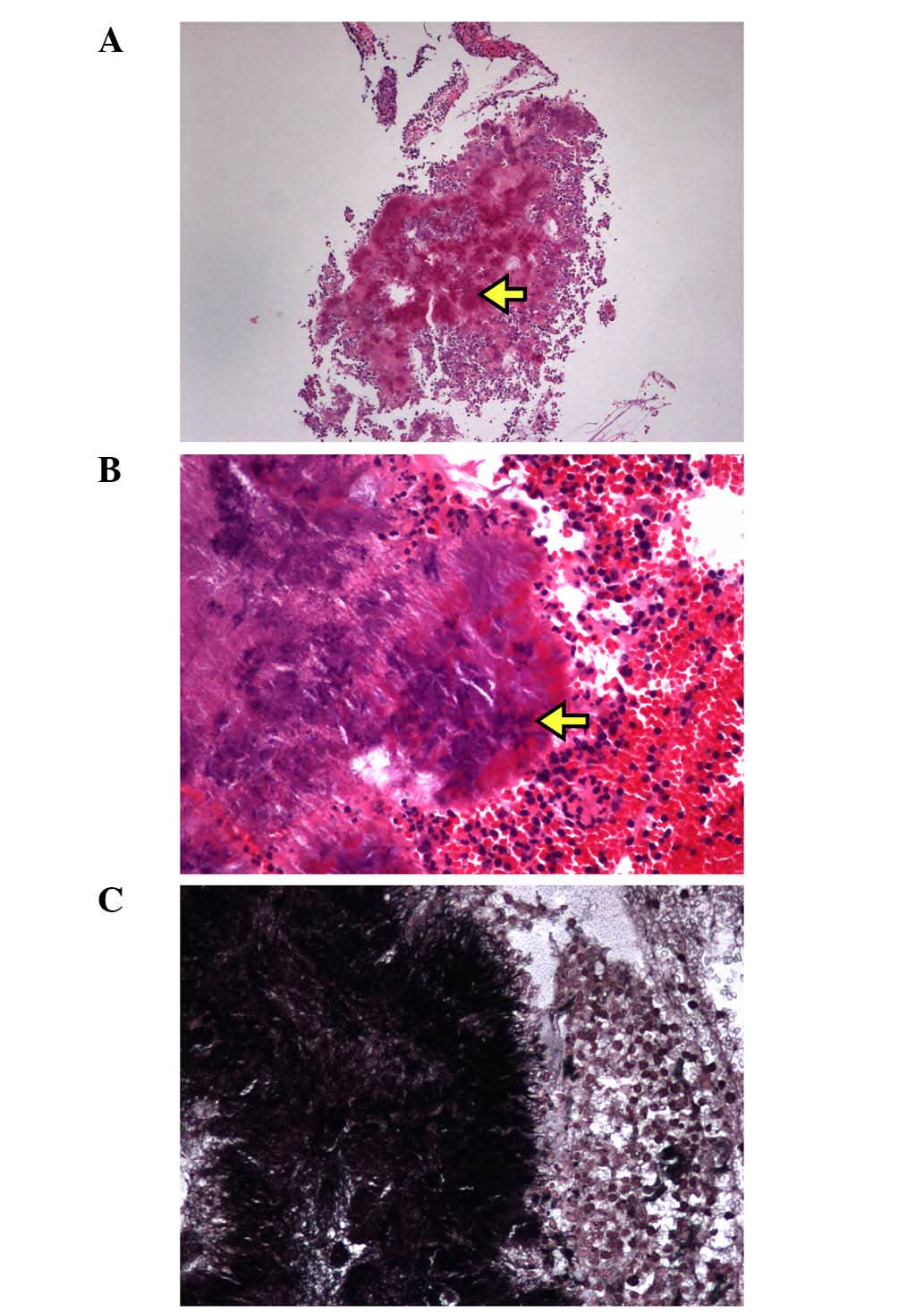
any colonies. Microscopic analysis at low magnification identified
cauliflower-shaped sulfur granules in association with acute and
chronic inflammation (Fig. 3A).
Higher-power microscopic examination revealed that these granules
were surrounded by a rosette of clubbed filaments (Fig. 3B). Furthermore, Grocott-Gomori
methenamine silver staining revealed the presence of filamentous
rods (Fig. 3C). Based on these
findings, the patient was diagnosed with nasopharyngeal
actinomycosis. After two months of oral antibiotic treatment with
500 mg amoxicillin four times per day, recovery was uneventful,
with no evidence of recurrence over the following 17 months.
Written informed consent was obtained from the patient prior to
publication of the study, and the study was approved by the Ethics
Committee of the Institutional Review Board of Kaohsiung Veterans
General Hospital (Kaohsiung, Taiwan).
Discussion
Human actinomycosis was first described in 1878 by
James Israel (4). Actinomycosis is a
rare anaerobic bacterial infection, typically caused by
Actinomyces israelii (1,2). The
members of the pathogenic Actinomyces species do not exist
freely in nature, but are commensals that normally inhabit the
oropharynx (particularly the tonsillar crypts and the gingivodental
crevices) (4), the abdominopelvic
region or the female genitourinary organs (1). Antecedent tissue injury with coinfection
by other pathogens that act in a synergistic manner may lead to
infection at any site in the body. Orocervicofacial actinomycosis
is the most common form of the disease, accounting for up to 60% of
all cases (2). Lesions are frequently
located at the angle of the jaw or in the submandibular region
(1). Common presenting features
include an acute painful abscess or chronic indolent soft-tissue
swelling, from which sinus tracts can develop over time. At
present, the clinical diagnosis of actinomycosis is challenging,
and therefore the disease has been referred to as a ‘masquerader of
head and neck’ disease (1–3).
Diagnosis is established most accurately by
isolating the Actinomyces species in cultures of clinical
specimens (1–3). However, previous studies have reported
that <50% of cases highly suspected to suffer from actinomycosis
lead to the growth of the organism in cultures (1–3). This is
considered to be due to the requirement of strict anaerobic
culturing conditions, previous antibiotic use or the overgrowth of
a concomitant organism (1–9). Clinicians must be knowledgeable when
submitting specimens in order to optimize the recovery of these
fastidious anaerobic bacteria. Under microscopic examination,
colonies of the organism form typical sulfur granules and present
as round or oval basophilic masses on hematoxylin-eosin slides, the
centres of which contain organized aggregates of filaments with
club-like eosinophilic structures that are referred to as the
Splendore-Hoeppli phenomenon (1–3). A
Gram-stained smear of the specimen may exhibit beaded, branched
Gram-positive filamentous rods (1–3). The
utilization of specific stains, including Grocott-Gomori
methenamine silver stain, MacCallum-Goodpasture stain,
p-aminosalicylic acid or Brown-Brenn stain, may aid in the
visualization of the bacilli (1). A
specific differential consideration is a diagnosis of nocardiosis
(9), which is positive for acid-fast
staining. Therefore, the combination of clinical images,
microbiological results and histological findings should enable a
successful diagnosis of actinomycosis (1–3).
The treatment of actinomycosis involves prolonged
antibiotic treatment and/or surgical resection (1–9). Surgery
may be reserved for certain circumstances, such as the excision of
the sinus tract, resection of necrotic tissue, sequestration of
bone and drainage of abscesses (1).
Although surgical intervention promotes recovery, it is not
curative by itself. High-dose penicillin (18–24 million units per
day) administered over a prolonged period is the standard form of
therapy (1–3). Doxycycline, clindamycin and erythromycin
may be used as effective alternative regimens, particularly for
patients who are allergic to penicillin (1–3). However,
previous data suggested that not all cases warrant long-term
antibiotics. Sharkawy (2) and Oostman
and Smego (3) stratified cases into
mild and complicated infections, and concluded that the modern
approach to treatment can be individualized depending on the site
of infection, severity of disease and the patient's response to
treatment. In addition, Daamen and Johnson (5) and Chiang et al (8) successfully treated patients with
nasopharyngeal actinomycosis using a four-week administration of
oral antibiotics.
To the best of our knowledge, nasopharyngeal
actinomycosis resulting in a draining fistula has not been
previously reported. Nasopharyngeal actinomycosis frequently
presents as a non-tender virulent granuloma that is capable of
expanding into contiguous tissue without regard for facial or
anatomical barriers. In terms of its mass effect, it may cause
unilateral otitis media with effusion (6), nasal airway obstruction (5) and carotid occlusion (7).
Since one of the hallmarks of nasopharyngeal
carcinoma is its marked racial/ethnic and geographic distribution
in Southeast Asia, recommendations for workup have changed over
time as technologies have improved. PET scanning, albeit not
routinely recommended, is not only capable of revealing the
location of tumors, but also provides valuable information
concerning metabolic tumor volume. Unlike in malignant disease,
positive FDG uptake depends on the presence and activity of
inflammatory leukocytes (10). In the
present study, it was hypothesized that acute inflammation with
direct actinomycetes invasion was the main cause of increased
uptake of 18F-FDG.
In conclusion, although the occurrence of
nasopharyngeal actinomycosis is extremely low, it is advisable to
always maintain a high level of clinical suspicion when treating
patients with a persistent nasopharyngeal mass that presents with
only vague symptoms. Healthy individuals may be infected without
any predisposing factors. A presumptive diagnosis is established by
the presence of sulfur granules containing Gram-positive
filamentous rods, but a negative result for acid-fast staining
(1). The prompt initiation of an
appropriate therapy is crucial for the eradication of this
insidious disease. In addition, prolonged observation and follow-up
are mandatory in order to detect recurrence. The present study
fills a breach in the clinical literature regarding this unique
disease entity. Future studies should aim to provide further
innovative information regarding the clinical evaluation and
management of nasopharyngeal actinomycosis.
References
|
1
|
Wong VK, Turmezei TD and Weston VC:
Actinomycosis. BMJ. 343:d60992011. View Article : Google Scholar
|
|
2
|
Sharkawy AA: Cervicofacial actinomycosis
and mandibular osteomyelitis. Infect Dis Clin North Am. 21:543–556.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Oostman O and Smego RA: Cervicofacial
actinomycosis: Diagnosis and management. Curr Infect Dis Rep.
7:170–174. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Melgarejo Moreno P, Hellin Meseguer D,
Marco Garrido A, Galindo Ortego X, Ruiz Macia JA and Hostalet F: A
correlation between age and Actinomyces in the adenotonsillar
tissue of children. B-ENT. 2:95–97. 2006.
|
|
5
|
Daamen N and Johnson JT: Nasopharyngeal
actinomycosis: a rare cause of nasal airway obstruction.
Laryngoscope. 114:1403–1405. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ono T, Yoshida Y, Izumaru S and Nakashima
T: A case of nasopharyngeal actinomycosis leading to otitis media
with effusion. Auris Nasus Larynx. 33:451–454. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kalra V and Malhotra A: Actinomycosis of
the nasopharynx causing carotid occlusion. Clin Neuroradiol.
23:129–131. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chiang CW, Chang YL and Lou PJ:
Actinomycosis imitating nasopharyngeal carcinoma. Ann Otol Rhinol
Laryngol. 109:605–607. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kolb CM, Ostrander S, Ramsey MJ, Burgos RM
and Belnap C: Pathology quiz case 1. Actinomycosis osteomyelitis of
the temporal bone. Arch Otolaryngol Head Neck Surg. 138:203–205.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rini JN and Palestro CJ: Imaging of
infection and inflammation with 18F-FDG-labeled leukocytes. Q J
Nucl Med Mol Imaging. 50:143–146. 2006.PubMed/NCBI
|