Introduction
In recent years, the application of positron
emission tomography-computed tomography (PET-CT), comprehensive
endoscopy involving random biopsies, laser-induced fluorescence
endoscopy, genetic testing and other techniques have significantly
increased the rate at which primary tumors are detected in cases of
cervical metastatic cancer (1–5). However,
the primary tumor cannot be found in 3–5% of these cases (6,7). In
certain cases during which patients with cervical metastatic cancer
involving an unknown primary tumor either do not receive prompt
treatment or receive inappropriate treatment during the course of
an individualized, multidisciplinary treatment process, metastatic
cancer may grow rapidly to form giant tumors that invade the blood
vessels, muscle and skin. Radiotherapy cannot be performed in these
cases due to the involvement of the skin, and chemotherapy is
frequently ineffective. As a consequence, salvage surgery followed
by post-operative chemoradiotherapy is the preferred therapeutic
approach for these cases.
Focal considerations of salvage radical neck
dissection include not only appropriately addressing issues
associated with the exposure of internal tissues, hemostasis, and
the treatment of the internal jugular vein and carotid artery, but
also protecting the vagus nerve, the cervical sympathetic trunk,
the phrenic nerve and the brachial plexus. After completing a
radical neck dissection, a suitable flap must be obtained for the
reconstruction of the affected region. The pectoralis major
myocutaneous flap includes a large quantity of tissue; thus, this
flap can adequately repair defects in cervical tissue caused by
radical neck dissection, and this flap may therefore be utilized
for a complete reconstruction that addresses these defects
(8–10). In addition, this flap has a rich blood
supply, exhibits strong resistance to infection and necrosis, and
heals rapidly. Thus, the use of this flap does not delay
post-operative chemoradiotherapy or raise concerns regarding the
exposure of the carotid artery due to post-operative flap necrosis.
Therefore, the flap meets the clinical requirements for the
treatment of patients with cervical metastatic cancer involving an
unknown primary tumor (8–10). The present study examined the
feasibility and efficacy of radical neck dissection combined with
reconstruction using the pectoralis major myocutaneous flap for the
treatment of giant cervical metastatic cancers that have developed
from unknown primary tumors and have invaded the skin.
Materials and methods
Ethics statement
The Ethical Committee of the Tumor Hospital of
Ganzhou Review Board (Ganzhou, Jiangxi, China) approved the study
protocol (20060502), and the study was conducted in accordance with
the principles of the Declaration of Helsinki regarding research
involving human subjects. Each of the patients provided written
informed consent to participate after the nature of the study had
been explained to them.
Case inclusion criteria
The included subjects were required to meet the
following criteria: i) Diagnosis of lymph node metastatic cancer
based on pathological examination; ii) no history of malignancy or
surgery for a tumor of unknown nature; iii) no clear symptoms
associated with particular organ systems and an absence of multiple
metastases outside of the cervical region; iv) no evidence of
primary tumors from clinical and laboratory tests; iv) lymph node
metastatic cancer that affects the skin, but does not infringe on
the hypopharynx, larynx or esophagus, with a maximum tumor diameter
of ≥10 cm; vi) a Karnofsky performance score of ≥80; vii) an
expected survival time of >6 months; viii) no lesions in vital
organs and the ability to tolerate the surgery; and ix) the patient
volunteered for the study and signed an informed consent form.
Case exclusion criteria
Patients were excluded from the study if they meet
any of the following criteria: i) A clear primary tumor; ii)
bilateral cervical lymph node metastasis; iii) lymph node
metastatic cancer that did not affect the skin, involved a maximum
tumor diameter of <10 cm, or affected the hypopharynx, larynx or
esophagus; and iv) lesions in vital organs or an inability to
tolerate the surgery.
Clinical data
A total of 16 patients were enrolled, including 14
males and 2 females. The enrolled patients were between 38 and 68
years of age, with a mean age of 54.7 years. Each individual was
subjected to a physical examination of the head and neck, enhanced
CT scanning of the nasopharynx, neck and chest, color Doppler
ultrasonography of the abdomen, laryngoscopy, esophageal endoscopy
and electronic bronchoscopy. Tumor markers and other indicators
revealed no primary tumors, and emission CT examinations revealed
no bone metastases. A total of 7 patients underwent routine PET-CT
examinations that did not identify any primary tumors or any
metastases other than the known cervical metastasis. The clinical
data are presented in Table I.
 | Table I.General clinical data for the examined
patients. |
Table I.
General clinical data for the examined
patients.
| Parameter | No. of cases (%) |
|---|
| Age, years |
|
|
30–45 | 5 (31.3) |
|
46–60 | 9 (56.2) |
| ≥61 | 2 (12.5) |
| Gender |
|
| Male | 14 (87.5) |
|
Female | 2 (12.5) |
| KPS score |
|
| ≥90 | 12 (75.0) |
|
80–89 | 4 (25.0) |
| Starting position of
the tumor |
|
| Upper
neck region (regions I-III) | 6 (37.5) |
| Lower
neck region (regions IV-V) | 2 (12.5) |
| Upper and
lower neck regions (regions I-III and regions IV-V) | 8 (50.0) |
| Pathological
type |
|
| Stage I
squamous | 3 (18.8) |
| Stage II
squamous | 6 (37.5) |
| Stage III
squamous | 5 (31.2) |
|
Unclassified | 2 (12.5) |
| N stage |
|
| N3 (10
cm≤N≤15 cm) | 11 (68.8) |
| N3
(N>15 cm) | 5 (31.2) |
| Skin invasion |
|
| <10
cm | 10 (62.5) |
| ≥10
cm | 6 (37.5) |
| Prior treatment
history |
|
| No
chemoradiotherapy | 3 (18.8) |
| Induction
chemotherapy, ≤2 treatments | 6 (37.5) |
| Induction
chemotherapy, >2 treatments | 7 (43.7) |
|
Radiotherapy | 0 (0.0) |
Surgery and reconstruction
Patients were subjected to radical neck dissection.
If necessary, a portion of the carotid artery was removed, and
vascular anastomosis or vascular grafting was performed.
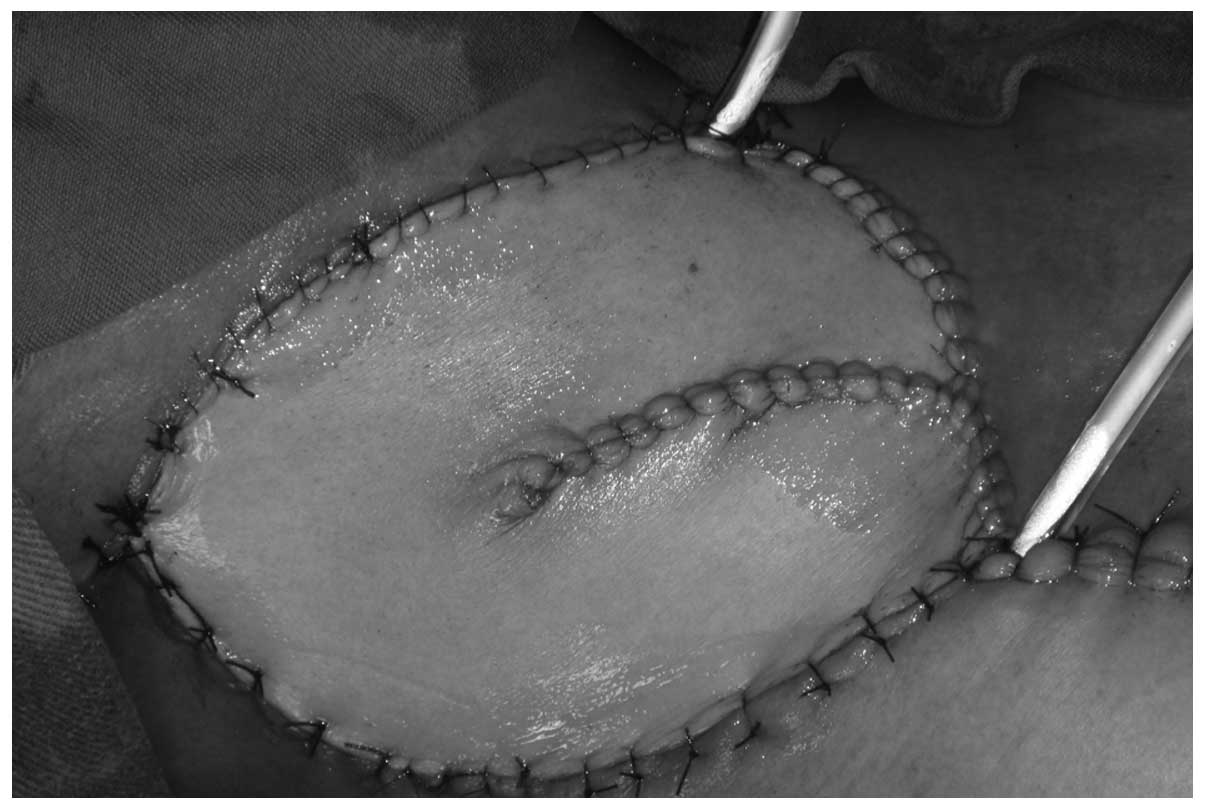
Subsequently, a reconstruction was conducted using the pectoralis
major myocutaneous flap. The shape and size of the flap obtained
for this purpose varied based on the size and shape of each skin
defect. The largest skin paddle used in this study had dimensions
of 23×15 cm.
Post-operative care
After surgery, various aspects of the flap,
including color, texture, temperature, degree of capillary filling
and swelling, were closely observed. A good airway and suction
drainage were ensured by careful observation and the provision of
relevant care. Care was also provided to strengthen patients'
postures, oral cavity health, nutritional status and psychological
conditions, as well as to alleviate pain.
Post-operative chemoradiotherapy
Chemoradiotherapy was started at 4–6 weeks
post-surgery. In cases of complete surgical resection with
pathologically negative margins, patients were subjected to 60–66
Gy in 30–33 fractions of radiotherapy for 6–7 weeks; in cases with
visible residual tumor tissue, patients received 66–70 Gy in 33–35
fractions of radiotherapy for 6–7 weeks. During radiotherapy,
concurrent chemotherapy involving 6 treatments of 30
mg/m2/week cisplatin (DDP) was administered.
Results
Surgical and post-operative
conditions
Among the 16 cases, there were no cases of major
hemorrhages due to carotid artery rupture. In 2 cases, direct
suture repair of blood vessels was performed, as the carotid artery
adventitia ruptured when a tightly adhering tumor was separated
from this artery. In 1 case, a segment ~1.5 cm in length was
resected from the carotid artery, and a tension-free end-to-end
anastomosis was performed once the artery was freed. There was 1
case in which the internal carotid artery was removed as
intraoperative findings revealed an occlusion in this artery. The
vagus nerve was partially removed in 2 cases, followed by a local
end-to-end anastomosis in 1 case and a long thoracic nerve graft
anastomosis in the other case. There were 2 cases of phrenic nerve
resection. The brachial plexus and cervical sympathetic trunk were
retained in all 16 cases. During the surgeries, frozen skin
exhibited negative margins, and the pectoralis major myocutaneous
flap was used for reconstruction in each case.
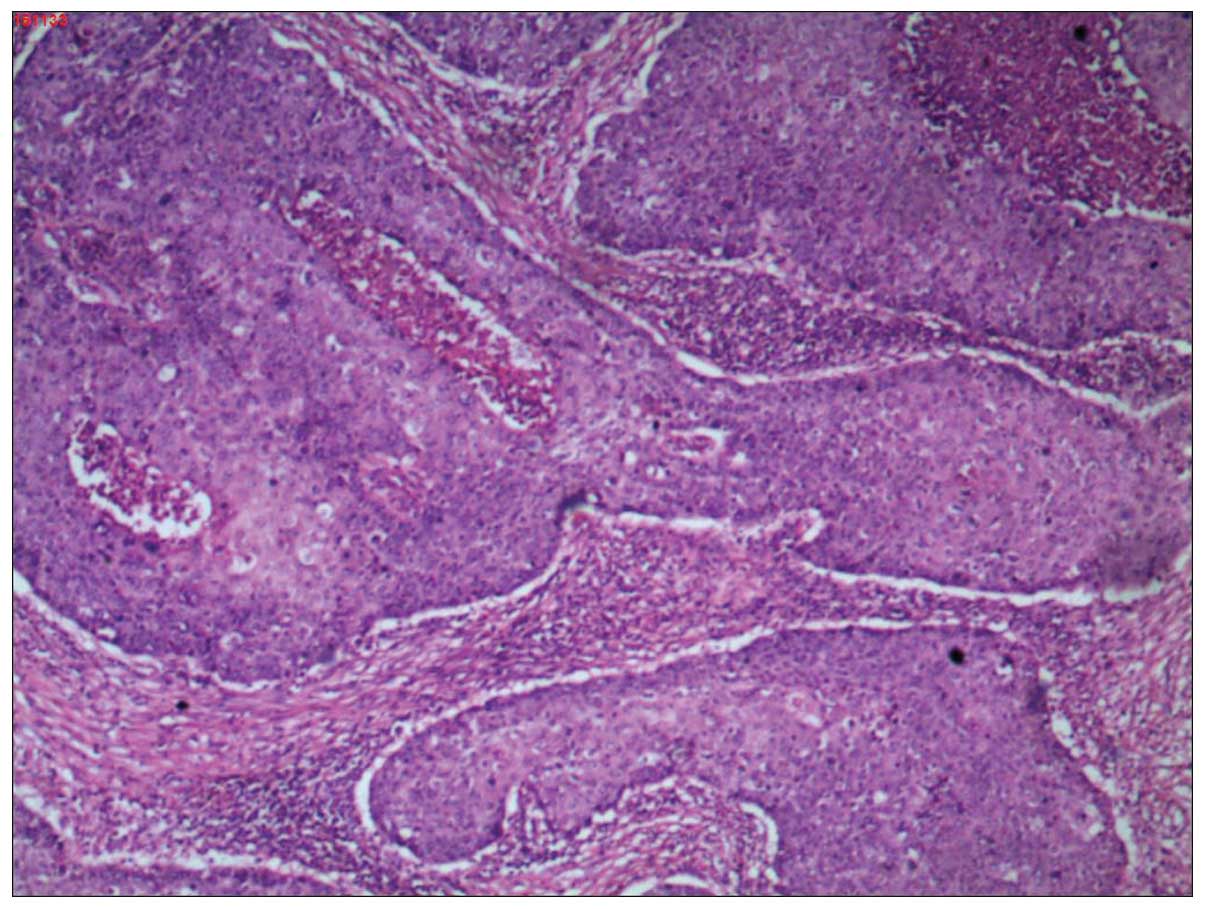
Post-operative pathology
Post-operative pathological analysis revealed that
there were 3 cases of well-differentiated squamous carcinoma, 8
cases of moderately-differentiated squamous carcinoma and 5 cases
of poorly-differentiated squamous carcinoma. The tumors had invaded
the muscle and skin in each examined case.
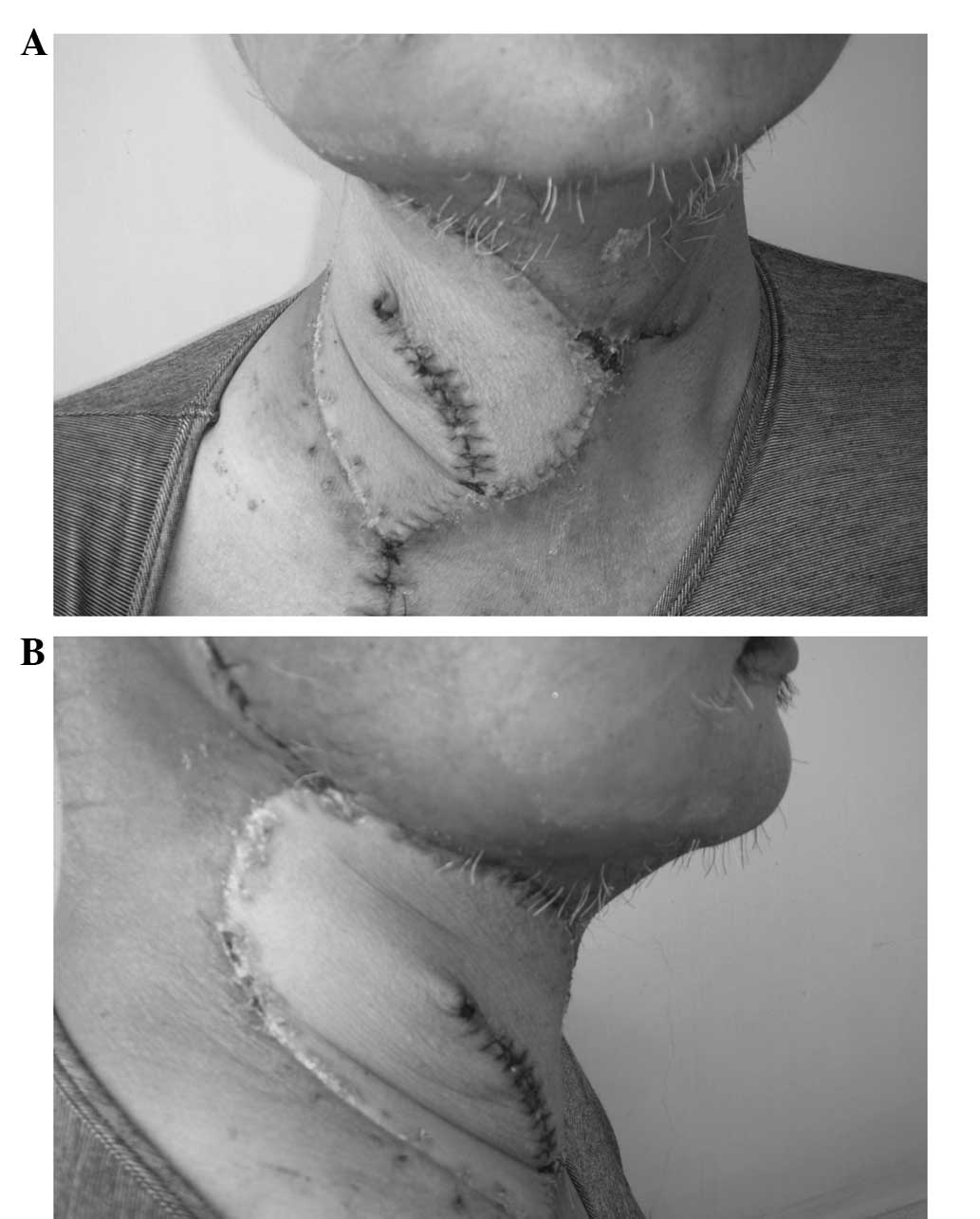
Appearance and chemoradiotherapy
tolerance
All pectoralis major myocutaneous flaps survived,
with no cases of necrosis. In 14 cases, primary healing of the
surgical wound occurred without incident; in the remaining 2 cases,
a small quantity of exudate from the surgical wound was observed
after the removal of cervical sutures, although the wounds healed
after their dressings were changed. Following cervical
reconstruction, the patients' necks were essentially symmetrical
and exhibited a satisfactory appearance. Chemoradiotherapy began
4–6 weeks after the surgery. In all cases, the flap exhibited good
tolerance during and after radiotherapy, and no interruptions in
radiotherapy occurred due to flap necrosis.
Donor region condition
In the 16 examined cases, no patients experienced
lymphedema, paresthesia or dysfunction of an upper extremity due to
the cutting of the pectoralis major muscle. In 9 cases, patients
were satisfied with their post-operative shoulder movement at the
donor site; in the remaining 7 cases, patients felt greater
weakness in this region following surgery relative to prior to
surgery. The 14 male patients were generally satisfied with the
post-operative appearance of the donor region, whereas the 2 female
patients were dissatisfied with the appearance of this region due
to the manifestations of differences in breast size and nipple
asymmetry.
Conditions during follow-up
Follow-up periods began on the date that
chemoradiotherapy was completed and ended on December 31, 2013. All
16 cases were followed, with follow-up periods ranging from 6 to 53
months. During follow-up, the recurrence of cervical tumors
occurred in 6 cases and mortality occurred in 9 cases. Detailed
follow-up information is presented in Table II.
 | Table II.Patients' surgical and follow-up
results. |
Table II.
Patients' surgical and follow-up
results.
| Case no. | Carotid
condition | Visible residual
tumor | Start time for
post-operative chemoradiotherapy, weeks | Follow-up duration,
months | Neck recurrence | Survival
condition | Cause of
mortality | Primary tumor |
|---|
| 1 | Normal | No | 4 | 22 | Yes | Succumbed | Lung metastasis | Unknown |
| 2 | Normal | No | 4 | 48 |
| Succumbed | Nasopharyngeal
hemorrhage | Nasopharyngeal
cancer |
| 3 | Normal | No | 4 | 36 | Yes | Alive |
| Unknown |
| 4 | Normal | No | 5 | 32 | Yes | Succumbed | Bone metastasis | Tonsil |
| 5 | Normal | Brachial plexus | 4 | 11 | Yes | Succumbed | Lung metastasis | Unknown |
| 6 | Adventitia
repair | No | 4 | 18 |
| Succumbed | Lung metastasis | Unknown |
| 7 | Normal | No | 4 | 25 | Yes | Succumbed | Neck recurrence | Unknown |
| 8 | Normal | No | 4 | 16 |
| Succumbed | Bone metastasis | Unknown |
| 9 | Normal | No | 6 | 22 |
| Alive |
| Unknown |
| 10 | Adventitia
repair | Brachial plexus | 5 | 10 | Yes | Succumbed | Neck
recurrence | Unknown |
| 11 | Normal | No | 4 | 18 |
| Alive |
| Unknown |
| 12 | Normal | No | 5 | 13 |
| Succumbed | Lung
metastasis | Unknown |
| 13 | Normal | No | 4 | 14 |
| Alive |
| Unknown |
| 14 | Normal | No | 4 | 11 |
| Alive |
| Esophageal
cancer |
| 15 | Artery
resection | No | 4 | 10 |
| Alive |
| Unknown |
| 16 | End-to-end
anastomosis | No | 5 | 6 | – | Alive | – | Unknown |
A report of a typical case
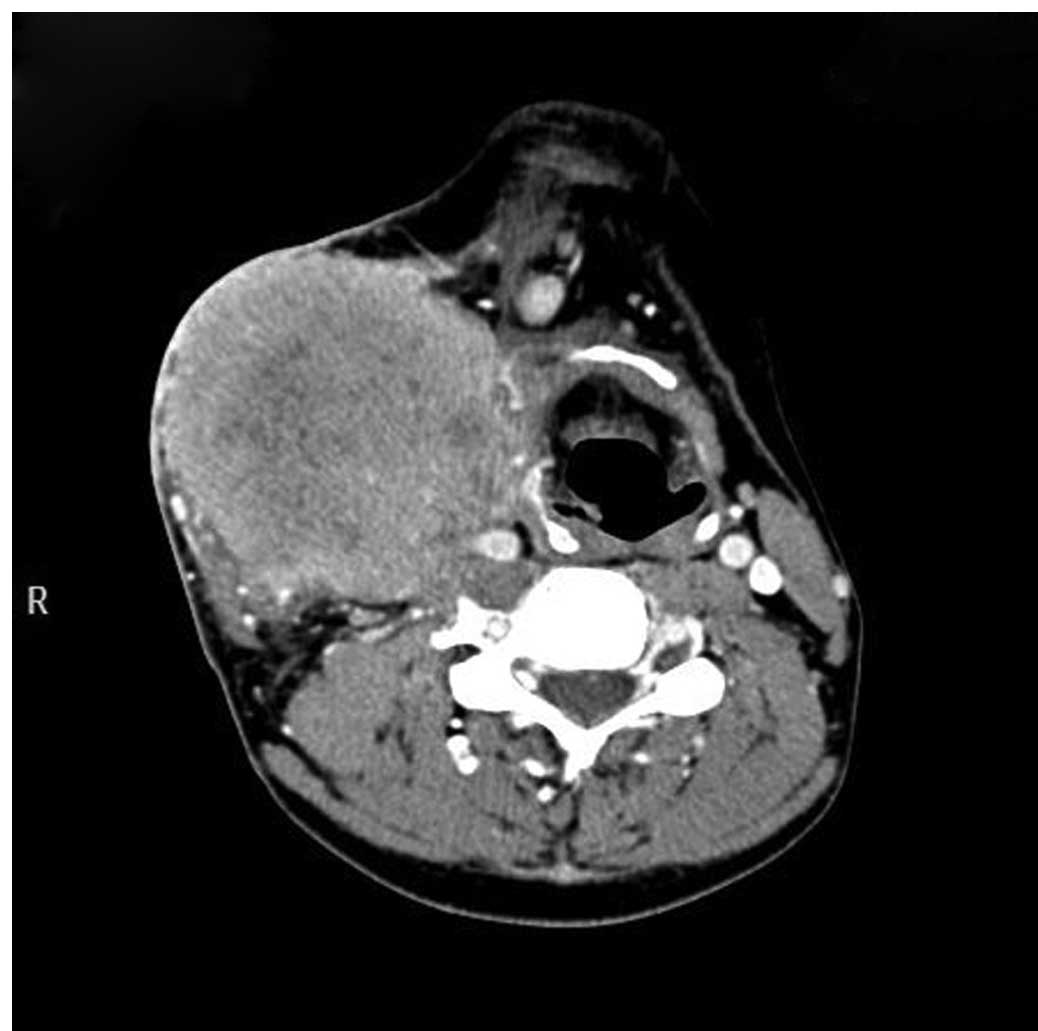
In early November 2011, a mass was inadvertently
discovered in the right side of the neck of a 39-year-old male.
This mass produced no pain or fever. The patient took self-selected
herbal medications, but this treatment produced no improvement.
Instead, the mass exhibited progressive enlargement and caused
intermittent needle-like pain; therefore, the patient was examined
in another hospital in January 2012. On January 31, CT examination
revealed nodules and patchy shadows in the upper lobe of the right
lung, which suggested the possibility of an old case of
tuberculosis. A re-examination of the right neck mass was therefore
recommended, and the idea that this mass was a neoplastic lesion
was considered. The results of a needle biopsy (C4942) on February
2 suggested that the mass could be a metastatic squamous cell
carcinoma with extensive hemorrhage and necrosis. PET-CT
examination (P0992) on February 10 revealed that the right-sided
neck mass exhibited central necrosis, which raised the possibility
of a malignant tumor (perhaps primary or neurogenic). Pressure on
the mass caused the trachea to shift to the left. Multiple small
nodules and cord-like shadows were observed in the apex of the
right lung, a finding consistent with the manifestations of
tuberculosis. Two three-week cycles of a chemotherapy regimen that
included docetaxel (75 mg/m2, day 1), DDP (75
mg/m2, day 1) and 5-fluorouracil (0.5 g/m2,
days 2–5) were administered; this treatment did not significantly
affect the tumor, but ameliorated the patient's symptom of
prickling sensations. The patient was hospitalized in the Tumor
Hospital of Ganzhou on April 2. A physical examination at this time
revealed no varicose veins, a soft neck, leftward deviation of the
trachea and a right-sided cervical tumor of ~13×10 cm in size. The
surface of the tumor was covered with ~10×8 cm of red skin, which
felt soft to the touch, indicating possible tissue necrosis, and
had relatively unclear boundaries; the mass was painful but
relatively rigid (Figs. 1 and
2). No palpable masses were found in
the left carotid region. Indirect endoscopic examination of the
nasopharynx revealed no tumors. Bilateral vocal cord activity was
normal, with no apparent space-occupying lesions in this region. No
primary tumor or other metastases beyond the cervical tumor were
identified in a comprehensive examination. CT examination revealed
a tumor without clear boundaries located in the right side of the
neck (Fig. 1). On April 14, under
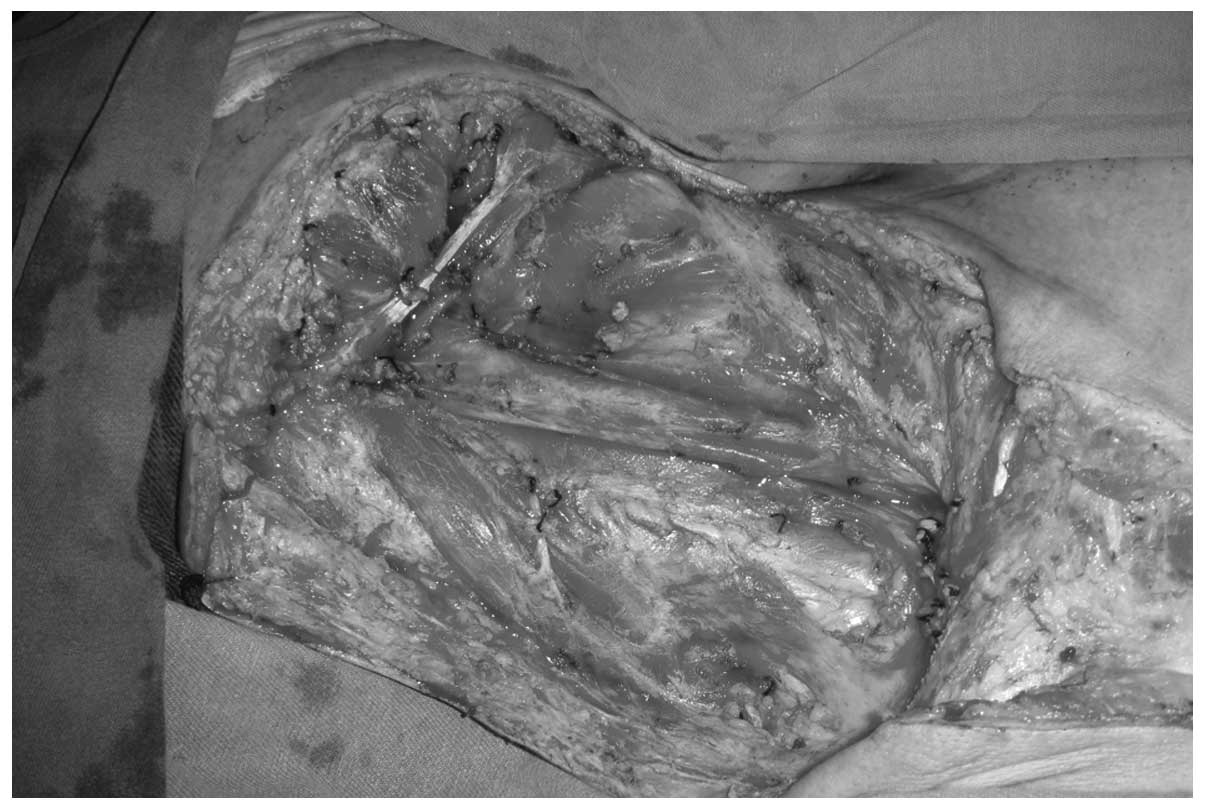
general anesthesia, the patient was subjected to a radical right
neck dissection combined with pectoralis major myocutaneous flap
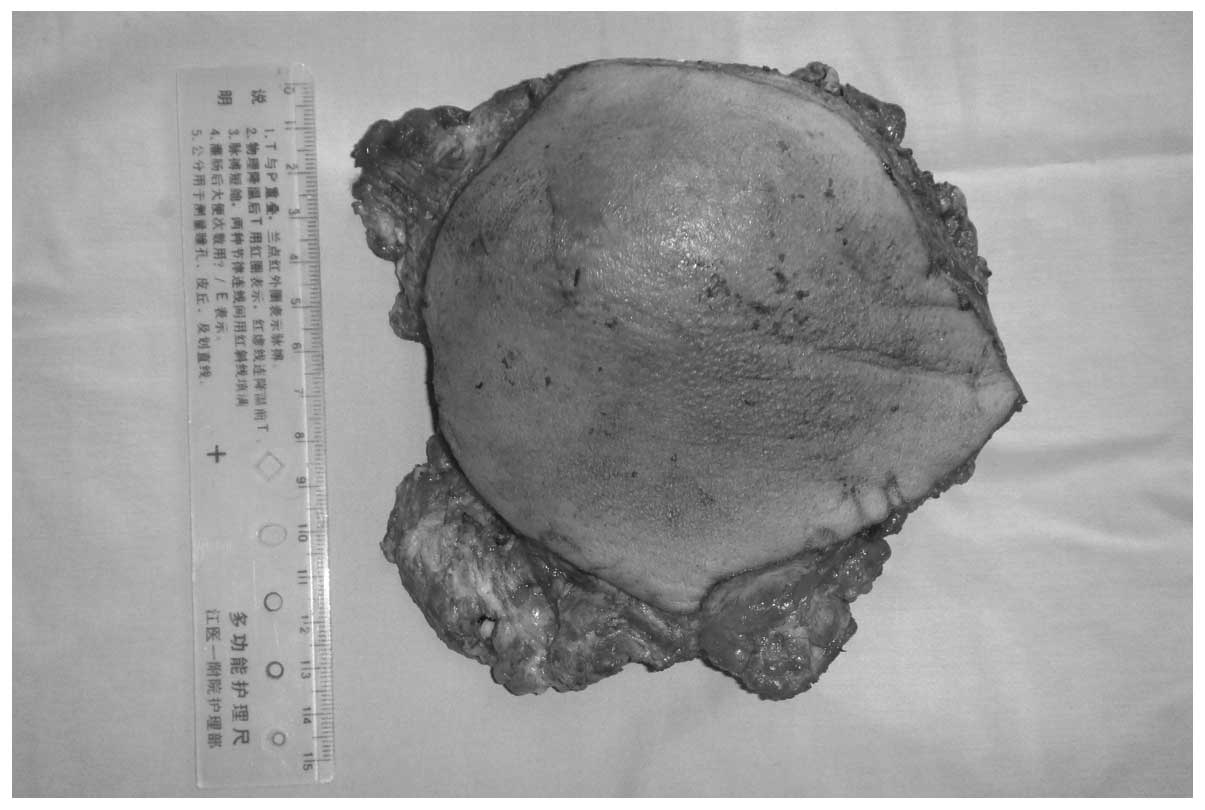
reconstruction (Figs. 3 and 4). The dissected pale yellow necrotic tissue
was 16×15×10 cm in diameter (Fig. 5)
which revealed a tumor mass, 12×10×10 cm in diameter.
Post-operative pathological examination revealed tumor cells with
large nuclei and abundant cytoplasm, as well as a number of
prominent nucleoli and keratosis (Fig.
6). Thus, a diagnosis of moderately-differentiated squamous
cell carcinoma was confirmed. Concurrent chemoradiotherapy was
provided beginning at 4 weeks post-surgery, including 35 radiation
treatments with a total absorbed dose of 70 Gy and 6 chemotherapy
treatments of 30 mg/m2/week DDP. During a return visit
in November, right pleural effusion was detected, resulting in a
diagnosis of tuberculosis. Symptomatic and anti-tuberculosis
treatments were administered, and the pleural effusion disappeared.
During the course of follow-up through December 2013, no primary
tumor was found and no recurrence of the cervical tumor or other
metastases was detected (Fig. 7).
Discussion
The main difficulties associated with the surgical
treatment of giant cervical metastatic tumors that have invaded the
skin and developed from unknown primary tumors include the
techniques not only for exposing blood vessels and separating these
vessels from the tumor during neck dissection, but also for
excising the flap and utilizing it for reconstruction. The main
post-operative issues include repairing arterial ruptures, stopping
bleeding associated with these ruptures and ensuring flap survival.
Thus, surgical incision choices should not only consider
aesthetics, but also be based on the principle of ensuring optimal
exposure of the relevant region. If part of a tumor is located
under the mandible or clavicle, causing difficulties with respect
to exposing blood vessels, one option to consider is truncating the
bone to enhance the exposure of these vessels and reduce surgical
difficulty (11). To avoid
intraoperative hemorrhage, the handling of blood vessels in
hazardous regions should only be performed under direct observation
and when the surgeon has absolute certainty regarding the
appropriate procedure. For the majority of patients with giant
cervical metastatic tumors, the carotid artery can be fully
separated from the tumor; if necessary, a portion of this artery
can be removed, and a vascular anastomosis or vascular graft can be
performed (12–14). If limited techniques are available for
the reconstruction of blood vessels or if a balloon occlusion test
on this carotid artery prior to surgery produces results indicating
the requirement for an carotid artery resection, then this artery
can be resected (12–14) during the course of the radical neck
dissection. The size and shape of the skin defect produced by a
radical neck dissection determines the size and shape of the
pectoralis major myocutaneous flap obtained for reconstruction. In
the present study, during surgery, after an exploration of the deep
surface of the pectoralis major muscle had clearly identified the
position of the pectoral branch of the thoracoacromial artery, the
pectoralis major muscle fiber tissue was completely cut at 1–2 cm
from the vascular pedicle, under direct visual observation. In this
manner, the pectoralis major myocutaneous flap was produced; this
flap was then shaped to the recipient area and used to repair the
large defects in the cervical tissue and skin produced by the neck
dissection. Following surgery, various aspects of the flap,
including color, texture, temperature, degree of capillary filling
and swelling, were closely observed, and intensive care for the
flap was provided as required. Successful surgical treatment was
performed for all 16 patients examined in this study. Therefore, if
a patient's condition is closely monitored prior to surgery,
appropriate surgical plans are conscientiously developed and the
patient is closely observed and well cared for after surgery, a
radical neck dissection followed by reconstruction using the
pectoralis major myocutaneous flap is a safe and effective approach
for treating giant cervical metastatic cancers that have invaded
the skin and developed from an unknown primary tumor.
In the 2013 National Comprehensive Cancer Network
guidelines for clinical practice in cases of head and neck cancer
(15), surgery remains the preferred
option for the radical treatment of cervical metastatic cancers
associated with an unknown primary tumor. Patel et al
(16) proposed the use of a radical
neck dissection combined with adjuvant post-operative
chemoradiotherapy for the treatment of pN3 cervical metastatic
cancers from unknown primary sites. Shoushtari et al
(17) reported that surgery combined
with chemoradiotherapy could provide survival benefits to patients
with pN3 cervical metastatic cancers from unknown primary origins.
If salvage surgery is not utilized for the treatment of these types
of cancers, the cervical tumors often fester, producing odors and
massive hemorrhages that severely compromise quality of life and
survival rates. Uncontrolled cervical tumors are the main cause of
chemoradiotherapy failure and patient mortality in these cases. The
surgical treatment of cervical lymph nodes by neck dissection
produces relatively high control rates and can improve rates of
patient survival (18,19). Therefore, radical neck dissection is
particularly important for patients with giant cervical metastatic
cancers that have invaded the skin and developed from unknown
primary tumors. Even in cases of palliative resection,
reconstruction with the pectoralis major myocutaneous flap can
reduce the festering of the cervical tumor and thereby improve
quality of life. Among the 16 examined patients in the present
study, there were 6 cases in which cervical tumors recurred after
surgery and chemoradiotherapy; however, only 2 patients succumbed
due to the recurrence of cervical tumors. Thus, this indicates that
radical neck dissection combined with reconstruction using the
pectoralis major myocutaneous flap and post-operative concurrent
chemoradiotherapy can enhance local control rates and quality of
life for patients who suffer from giant cervical metastatic cancers
that have invaded the skin and developed from unknown primary
tumors. This treatment approach can achieve satisfactory
outcomes.
References
|
1
|
Karapolat I and Kumanlıoğlu K: Impact of
FDG-PET/CT for the detection of unknown primary tumours in patients
with cervical lymph node metastases. Mol Imaging Radionucl Ther.
21:63–68. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mehta V, Johnson P, Tassler A, et al: A
new paradigm for the diagnosis and management of unknown primary
tumors of the head and neck: A role for transoral robotic surgery.
Laryngoscope. 123:146–151. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kulapaditharom B, Boonkitticharoen V and
Kunachak S: Fluorescence-guided biopsy in the diagnosis of an
unknown primary cancer in patients with metastatic cervical lymph
nodes. Ann Otol Rhinol Laryngol. 108:700–704. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bishop JA, Ma XJ, Wang H, et al: Detection
of transcriptionally active high-risk HPV in patients with head and
neck squamous cell carcinoma as visualized by a novel E6/E7 mRNA in
situ hybridization method. Am J Surg Pathol. 36:1874–1882. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Abuzeid WM, Bradford CR and Divi V:
Transoral robotic biopsy of the tongue base: A novel paradigm in
the evaluation of unknown primary tumors of the head and neck. Head
Neck. 35:E126–E130. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pavlidis N and Fizazi K: Cancer of unknown
primary (CUP). Crit Rev Oncol Hematol. 54:243–250. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dennis JL, Hvidsten TR, Wit EC, et al:
Markers of adenocarcinoma characteristic of the site of origin:
development of a diagnostic algorithm. Clin Cancer Res.
11:3766–3772. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Teo KG, Rozen WM and Acosta R: The
pectoralis major myocutaneous flap. J Reconstr Microsurg.
29:449–456. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jena A, Patnayak R, Sharan R, et al:
Outcomes of pectoralis major myocutaneous flap in female patients
for oral cavity defect reconstruction. J Oral Maxillofac Surg.
72:222–231. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ribeiro Salles Vanni CM, de Matos LL, Faro
Junior MP, et al: Enhanced morbidity of pectoralis major
myocutaneous flap used for salvage after previously failed
oncological treatment and unsuccessful reconstructive head and neck
surgery. ScientificWorldJournal. 2012:3841792012.PubMed/NCBI
|
|
11
|
Teng MS, Genden EM, Buchbinder D and Urken
ML: Subcutaneous mandibulotomy: A new surgical access for large
tumors of the parapharyngeal space. Laryngoscope. 113:1893–1897.
2003.PubMed/NCBI
|
|
12
|
Carpenter SG, Stone WM, Bower TC, et al:
Surgical management of tumors invading the aorta and major arterial
structures. Ann Vasc Surg. 25:1026–1035. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhengang X, Colbert S, Brennan PA, et al:
Surgical management of metastases that involve the carotid artery
in cases of primary squamous cell carcinoma of the head and neck.
Int J Oral Maxillofac Surg. 42:440–445. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Popescu B, Berteșteanu SV, Grigore R, et
al: Case reports - common and external carotid artery resection in
head and neck cancer patients. J Med Life. 6:180–184.
2013.PubMed/NCBI
|
|
15
|
NCCN Clinical Practice Guidelines in
Oncology (NCCN Guidelines), Head and Neck Cancers (Version 2.2013).
http://www.nccn.org/professionals/physician_gls/f_guidelines.asp
|
|
16
|
Patel RS, Clark J, Wyten R, et al:
Squamous cell carcinoma from an unknown head and neck primary site:
A ‘selective treatment’ approach. Arch Otolaryngol Head Neck Surg.
133:1282–1287. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shoushtari A, Saylor D, Kerr KL, et al:
Outcomes of patients with head-and-neck cancer of unknown primary
origin treated with intensity-modulated radiotherapy. Int J Radiat
Oncol Biol Phys. 81:e83–e91. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cizmarevic B, Lanisnik B and Dinevski D:
Cervical lymph node metastasis of squamous cell carcinoma from
unknown primary tumor. Coll Antropol. 36(Suppl 2): 27–32. 2012.
|
|
19
|
Park GC, Jung JH, Roh JL, et al:
Prognostic value of metastatic nodal volume and lymph node ratio in
patients with cervical lymph node metastases from an unknown
primary tumor. Oncology. 86:170–176. 2014. View Article : Google Scholar : PubMed/NCBI
|