Introduction
Glioblastoma multiforme (GBM) is the most frequently
occurring malignant primary brain tumor in adults. These tumors
generally develop in the fifth and sixth decades of life (1,2). However,
these lesions rarely occur in the cerebellum, with prior studies
reporting that only 0.4–3.4% of all GBM tumors occur in this
location (3–5). Hypertension, impaired balance and gait
disturbance are typical clinical manifestations (1). The best treatment for cerebellar
glioblastoma is removal of as much of the tumors as possible but
keeping surgical morbidity to a minimum (2). The prognosis of cerebellar glioblastoma
is similar to that of anaplasic astrocytoma (1). In the current study, a case of primary
cerebellar glioblastoma is presented, and the physiopathology,
clinical presentation, diagnosis, differential diagnosis, treatment
and general outcome of this disease is discussed.
Case report
A 61-year-old female with no other medical history
was referred to West China Hospital of Sichuan University (Chengdu,
China) and presented with nausea, vomiting and balance problems
that had persisted for >1 month. A neurological examination
demonstrated cerebellar signs, including positive bilateral
finger-nose and knee-shin tests. Tumor marker analysis and other
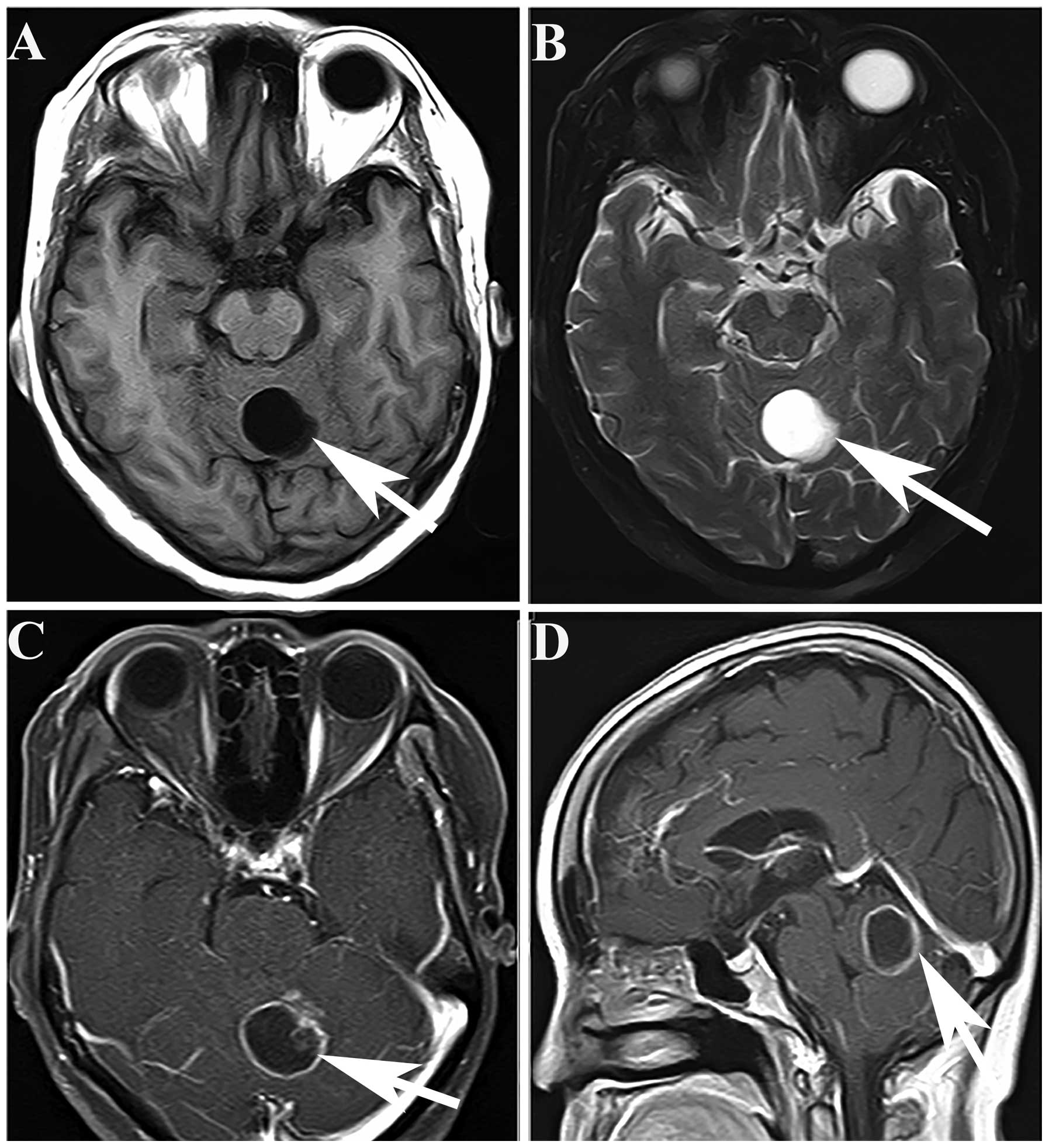
blood tests were negative. Cranial magnetic resonance imaging (MRI)
showed one regular contour of a mass lesion in the cerebellar
vermis. The mass was present as a hypointense and hyperintense
lesion in the cerebellar vermis in T1- and T2-weighted images,
respectively (Fig. 1A and B). The
mass had well-defined borders and large areas of central necrosis.
T1-weighted magnetic enhanced imaging showed a well-defined,
heterogeneously ring-enhancing lesion, with one additional enhanced
node (Fig. 1C and D). The provisional
diagnosis was of a metastatic lesion of the cerebellum. The patient
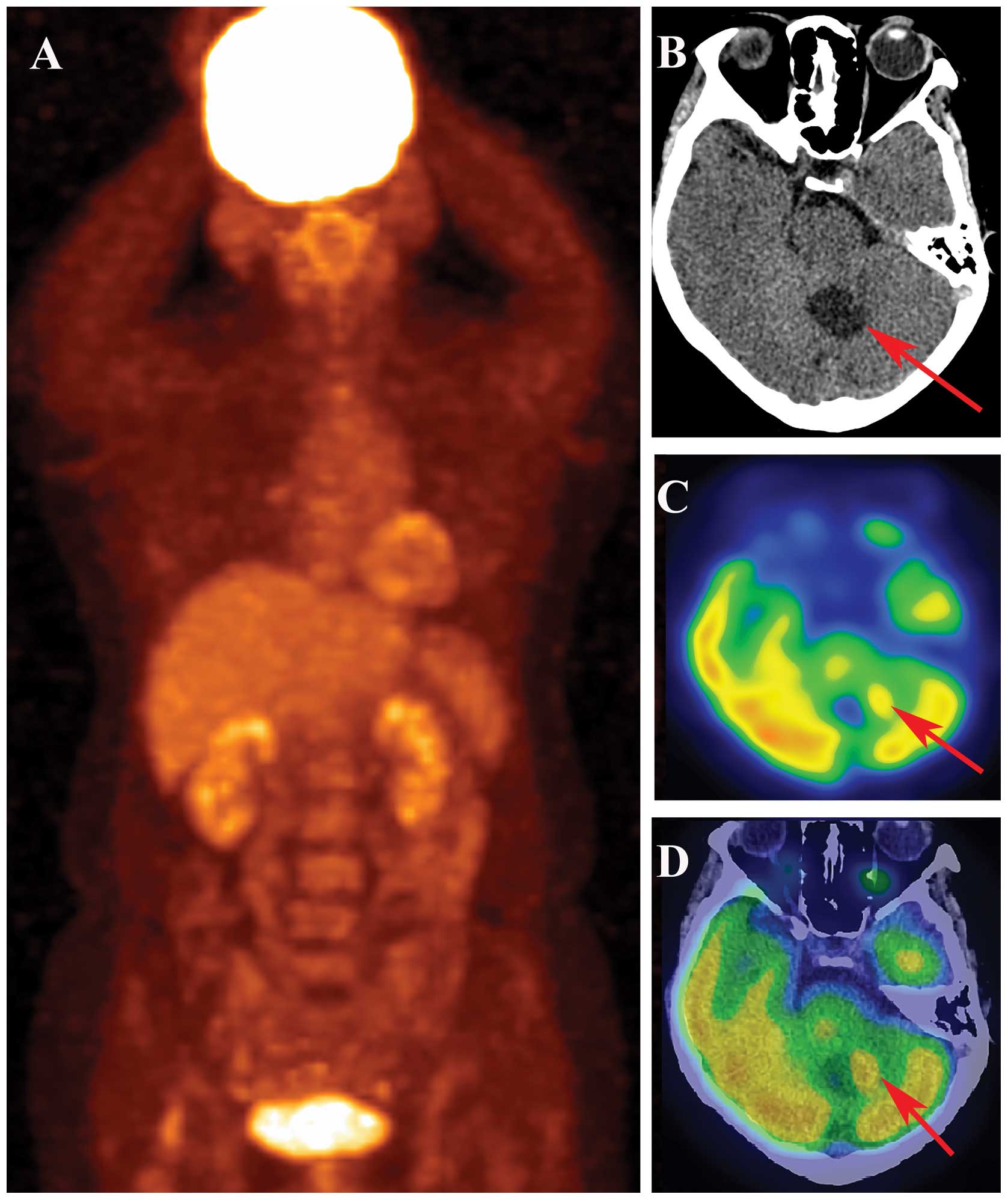
signed the written informed consent and then underwent a positron
emission tomography/computed tomography (PET/CT) examination. There
was no abnormal glucose uptake on coronal PET imaging (Fig. 2A). Cerebral CT showed one hypodense
lesion with a nodule alongside the cerebellar vermis (Fig. 2B). In PET imaging, the nodule was
observed to have much higher glucose uptake than other tissues
(Fig. 2C and D). Therefore, the
patient was diagnosed with primary brain tumors.
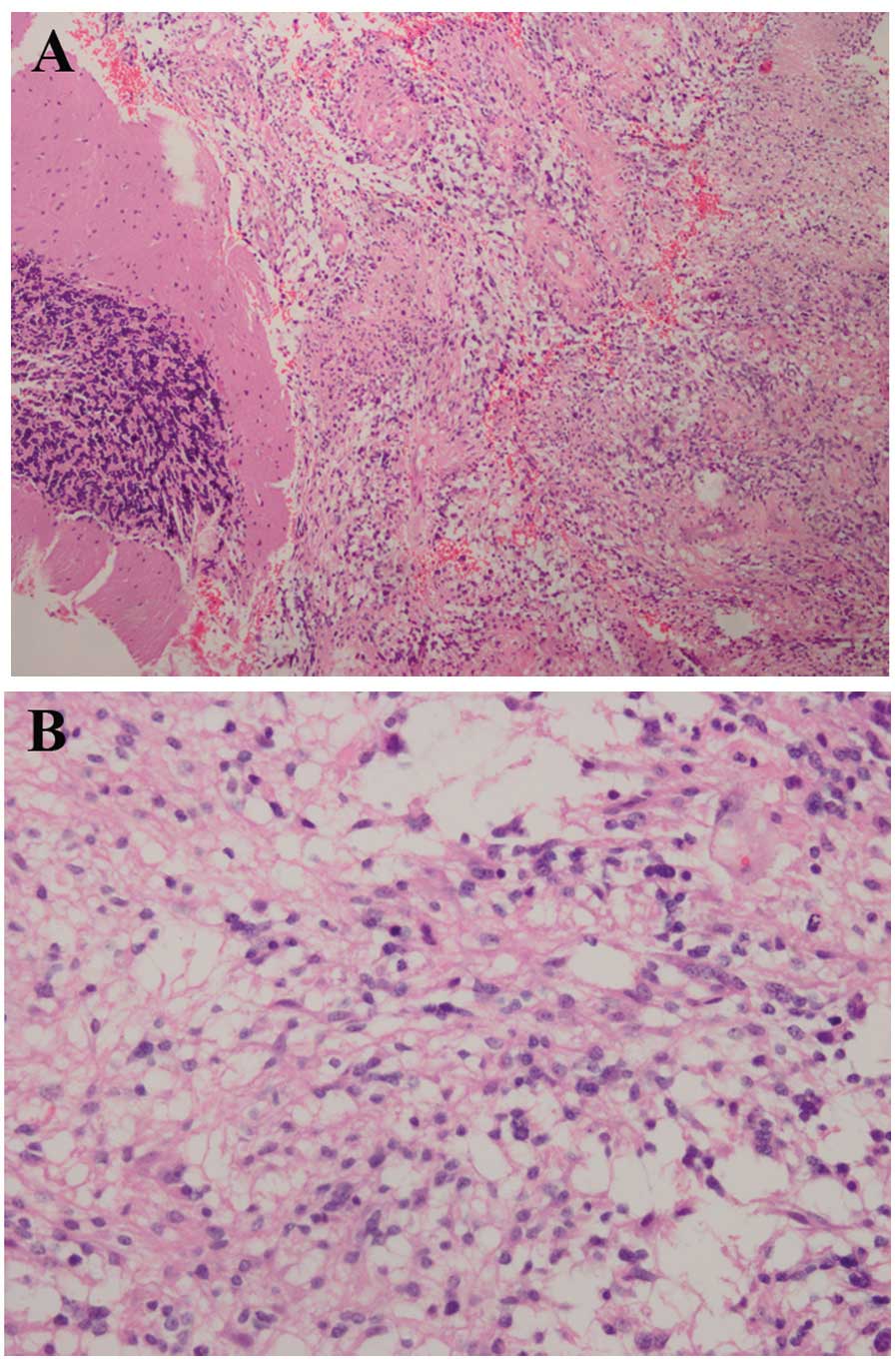
The patient underwent a cerebellar lesion resection
at West China Hospital of Sichuan University (Chengdu, China) and
the pathology of the lesion diagnosed a glioblastoma (class IV;
Fig. 3). Following the surgery,
histopathological examination revealed a cellular tumor, which was
consistent with glioblastoma that met the World Health Organization
criteria of grade 4 astrocytoma. The appearance of the tumor was
consistent with necrosis, pseudo-palisading and vascular
hyperplasia. Photomicrograph of tumor sections demonstrated an
intense cellular density and nuclear pleomorphism, which was
characterized by marked anisokaryosis and larger nuclei than is
normal. The cells had an abundant and eosinophilic cytoplasm and
umerous mitoses were observed (Fig.
3).
The patient had modest brain edema following the
surgery for a few days, but improved immediately after diuretics
were administered. The neurologic signs improved and the clinical
presentation disappeared. The patient did not receive radiotherapy
or chemotherapy after the surgery. There was no sign of tumor
recurrence after 18 months.
Discussion
Cerebellar GBM in adults is rare, and thus comprises
only a small proportion of all GBM tumors of the brain. GBM of the
cerebellum can be observed in all age groups. A study has shown
that the male-to-female ratio for this disease is 2:1, and that
~70% of the tumors occur in adults (average age, 46.7 years), while
30% occur in children (average age, 10.4 years) (6). GBM is a stage 4 tumor according to the
World Health Organization classification (7). The prognosis of this entity is
uncertain, and factors associated with prognosis have been unclear.
According to the case study of a 41-year-old male with a cerebellar
glioblastoma developing in the cerebellar hemisphere who was
treated 35 years previously by radiotherapy, radiation may be a
cause for inducing GBM (8): The
patient had medulloblastoma (MB) in the cerebellar vermis, and
postoperatively he received a total of 40 Gy radiations to the
whole brain and 30.5 Gy to the spine without chemotherapy (8).
Patients with GBM typically present with increased
hypertension, impaired balance and gait disturbance (1). Upon examination, patients exhibit
cerebellar signs, as occurred in the present case. The symptoms of
dizziness, mental confusion and neck pain can also be present
(9). A diagnosis of cerebellar GBM is
not usually pre-operatively suspected, although certain CT and MRI
characteristics may indicate it (6,9).
Cerebellar metastases, hemangioblastomas, brain abscesses and
anaplastic astrocytomas are common differential diagnoses in
adults. Brain abscesses often have symptoms of infection. Abscess
walls are mostly smooth without nodules. Enhanced CT and MRI scans
show incomplete ring-like reinforcements, which are thin and
uniform. Hemangioblastomas always occur singly, and >90% occur
in the cerebellar hemisphere. The CT and MRI indications are
similar to those in the present case. The pathology of a lesion can
only be confirmed after surgery. Brain metastases always have
necrosis within them and show greater than one lesion with marked
peripheral edema (1,2,4,9). The history of a primary tumor is
important. In fact, to identify these diseases, a number of
different examinations are required, and they may take a long time
to complete. At the West China Hospital of Sichuan University,
patients are provided with PET/CT examinations according to whether
lesions take up glucose or not, so that this disease can be
identified. However, reports of signs of different brain tumors in
PET/CT scans are rare. As PET/CT scans become increasingly common,
they may become a novel method for identifying brain tumors.
Cerebellar glioblastoma treatment is usually
palliative, consisting of surgery, radiotherapy and chemotherapy
(1,2).
Decisions regarding surgery depend on factors such as patient age,
performance, diseased region in the brain and resectability of the
tumor (1,2,4,6). Subsequent to surgery, patients can be
treated with radiotherapy and chemotherapy. However, GBM is the
highest graded astrocytoma and the recurrence rate following
surgery is high. Moreover, the prognosis of patients with
glioblastoma is poor, with a 2-year survival rate of 10% and <5%
of the patients surviving for a long period of time. The mean
survival time for patients with cerebellar glioblastoma after the
beginning of symptomatology has been reported to be 12–19 months
(6,10).
The present study reports a rare case of cerebellar
GBM. PET/CT examination may provide a novel method for diagnosing
GBM and providing differential diagnoses for metastases, abscesses
and hemangioblastomas in the cerebellum.
Acknowledgements
This study was supported by the National Natural
Science Foundation (grant nos. 81271532 and 30900378).
References
|
1
|
El El Maaqili MR, Hossini A, El Fatemi N,
et al: Primary glioblastoma of the cerebellum in a 19-year-old
woman: a case report. J Med Case Rep. 6:3292012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Grahovac G, Tomac D, Lambasa S, et al:
Cerebellar glioblastomas: Pathophysiology, clinical presentation
and management. Acta Neurochir. 151:653–657. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Babu R, Sharma R, Karikari IO, et al:
Outcome and prognostic factors in adult cerebellar glioblastoma. J
Clin Neurosci. 20:1117–1121. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kuroiwa T, Numaguchi Y, Rothman MI, et al:
Posterior fossa glioblastoma multiforme: MR findings. AJNR Am J
Neuroradiol. 16:583–589. 1995.PubMed/NCBI
|
|
5
|
Roth JG and Elvidge AR: Glioblastoma
multiforme: A clinical survey. J Neurosurg. 17:736–750. 1960.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mattos JP, Marenco HA, Campos JM, et al:
Cerebellar glioblastoma multiforme in an adult. Arq Neuropsiquiatr.
64:132–135. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Louis DN, Ohgaki H, Wiestler OD, et al:
The 2007 WHO classification of tumours of the central nervous
system. Acta Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hamasaki K, Nakamura H, Ueda Y, et al:
Radiation-induced glioblastoma occurring 35 years after radiation
therapy for medulloblastoma: case report. Brain Tumor Pathol.
27:39–43. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Demir MK, Hakan T, Akinci O and Berkman Z:
Primary cerebellar glioblastoma multiforme. Diagn Interv Radiol.
11:83–86. 2005.PubMed/NCBI
|
|
10
|
Kulkarni AV, Becker LE, Jay V, et al:
Primary cerebellar glioblastomas multiforme in children Report of
four cases. J Neurosurg. 90:546–550. 1999. View Article : Google Scholar : PubMed/NCBI
|