Introduction
Liposarcoma is a common type of soft tissue sarcoma
(1), which occurs most commonly in
the extremities (52%), followed by the retroperitoneum (19%)
(2). Retroperitoneal liposarcoma is
usually asymptomatic until the liposarcoma is large enough to
compress the surrounding organs (3).
It is often misdiagnosed due to its rarity and absence of symptoms.
In the experience of the authors, symptoms would only occur if the
liposarcoma presses on the surrounding organs. However, the
retroperitneum is a large space in which the retroperitoneal
liposarcoma to grow. The symptoms of the tumor would not arise
until the tumor grows to a certain dimension. The management is
surgical intervention. Even with complete removal of the
liposarcoma, prognosis remains poor. The 5-year survival rate of
well-differentiated retroperitoneal liposarcoma is 83%, while it is
20% for the dedifferentiated tumor subtype (4). Successful complete resection of
retroperitoneal liposarcoma may increase the 5-year survival rate.
To the best of our knowledge, there is currently no evidence that
chemotherapy or radiotherapy improve survival rates. The current
study presented a patient diagnosed with retroperitoneal
liposarcoma who was treated in April 2014. In addition, 13 cases of
retroperitoneal liposarcoma from the Chinese literature were also
reviewed. Recurrence was observed in 5/14 patients. All the
patients underwent complete resection and 5 received combined
multiple organs resection. The aim of the present study was to
report a giant retroperitoneal liposarcoma, and to discuss the
epidemiology, histopathology, imaging characteristics and the
management of retroperitoneal liposarcoma. Approval for the present
study was obtained from the ethics committee of Zhejiang University
(Hangzhou, China) and informed consent was provided by the
patient.
Case report
A 48 year-old female was admitted to the Department
of Surgery, The Second Affiliated Hospital, College of Medicine,
Zhejiang University (Hangzhou, China) in April 2014, presenting
with abdominal pain in the left side for one month, accompanied by
abdominal distention following eating. The past medical and
surgical history of the patient had no relevance to the case. The
physical examination indicated a 25×35 cm oval mass with medium
texture below the left costal margin without tenderness or rebound
tenderness. The laboratory examinations, including routine blood
and urine tests. CA199, 10.8 U/ml (normal range, <37 U/ml);
CA153 7.5 U/ml (normal range, <30 U/ml); CA125 5.4 U/ml (noraml
range, <35 U/ml); CEA 1.1 ng/ml (normal range, <5 ng/ml); and
AFP, 0.9 ng/ml (normal range, <20 ng/ml). All the results were
within the reference ranges and therefore normal. Routine blood
test: Red blood cell count, 4.51×1012/l (normal range,
3.5–5.0×1012/l); white blood cell count,
6.6×109l (normal range: 4.0–10.0×109/l);
platelet count, 198×109/l (normal range,
100–300×109/l); hemoglobin, 121 g/l (normal range,
110–150 g/l). Routine urine test: Urine specific gravity, 1.013
(normal range, 1.010–1.030); pH 5.5 (normal range: pH 5.0–7.0); red
blood cell count, 0/HP (normal range, 0–3/HP); white blood cell
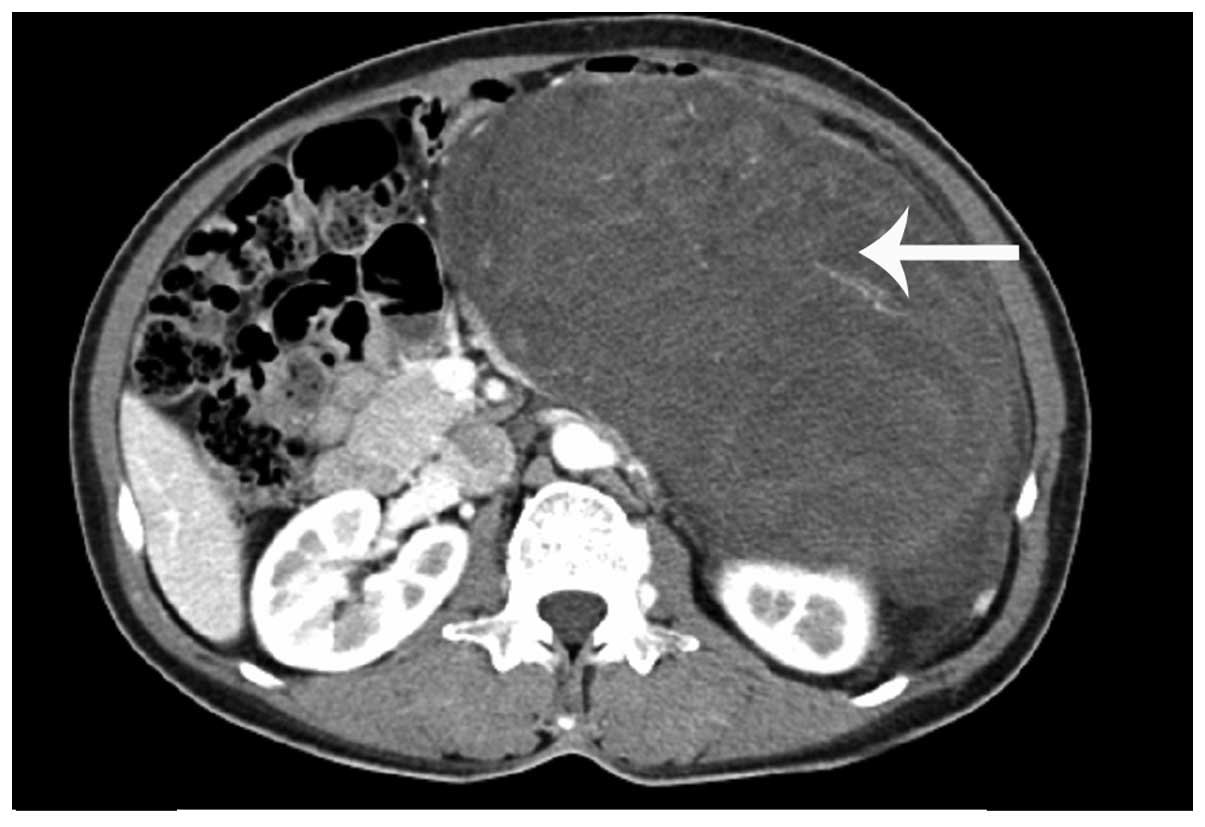
count, 1/HP (normal range, 0–5/HP). Computed tomography (CT;
Fig. 1) and magnetic resonance
imaging (MRI) demonstrated a giant mass in the left abdomen,
pressing into the left kidney and pancreas; therefore, it was
decided surgery was necessary.
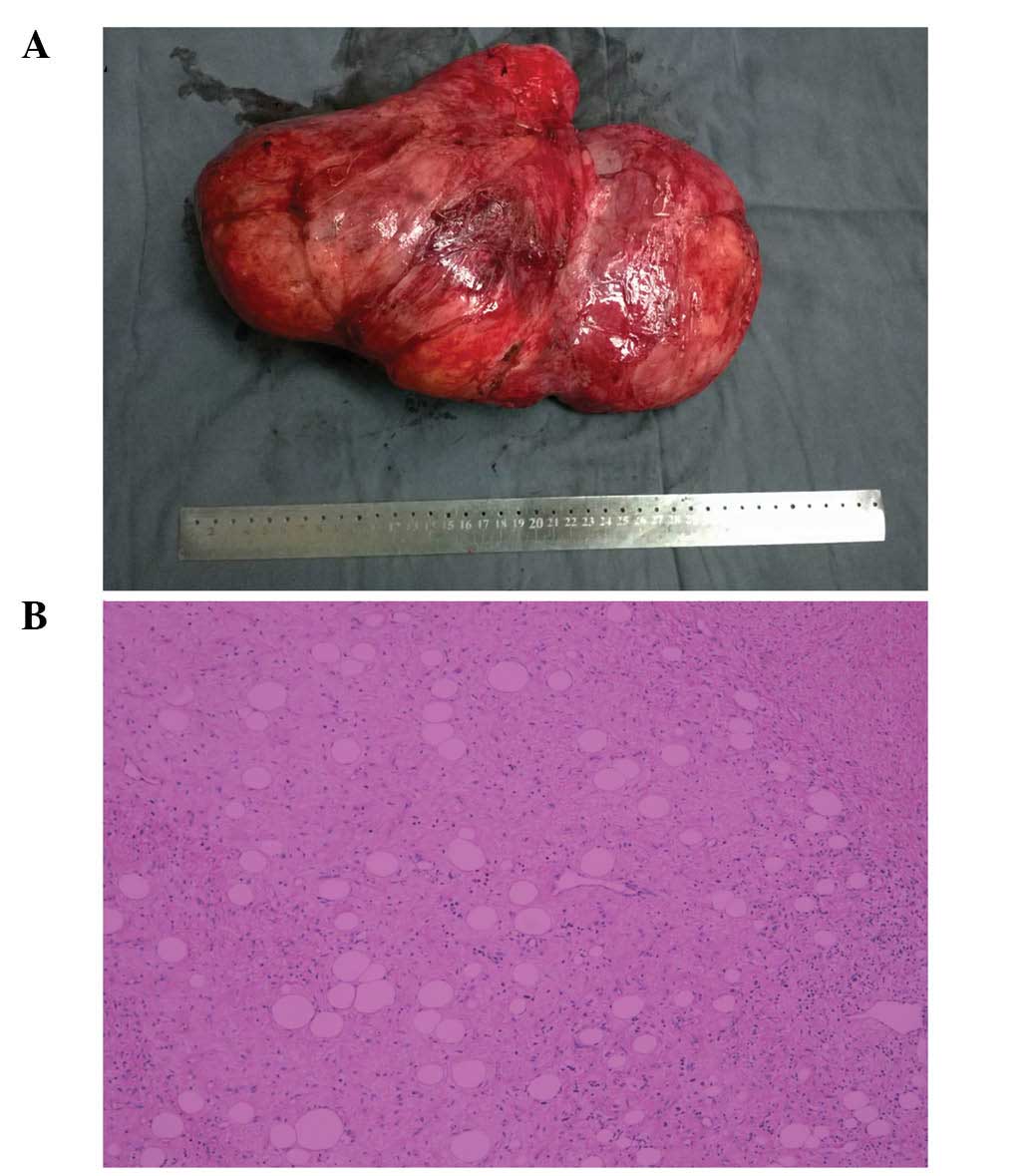
During surgery, it was determined that the mass
originated from the left fatty renal capsule and the kidney was
partly invaded. The patient received complete resection of the
liposarcoma and partial resection of the left kidney. The mass was
30×20×15 cm in size (Fig. 2A).
The mass was pathologically identified as myxoid
liposarcoma (Fig. 2B). The
immunohistochemical analysis was conducted at the Department of
Pathology at The Second Affiliated Hospital of the College of
Medicine, Zhejiang University (Hangzhou, China), and revealed that
the mass was positive for vimentin, weakly positive for S-100 and
negative for cytokeratin (AE1/AE3). A few tumor cells were positive
for the proliferation marker Ki-67. The patient recovered well and
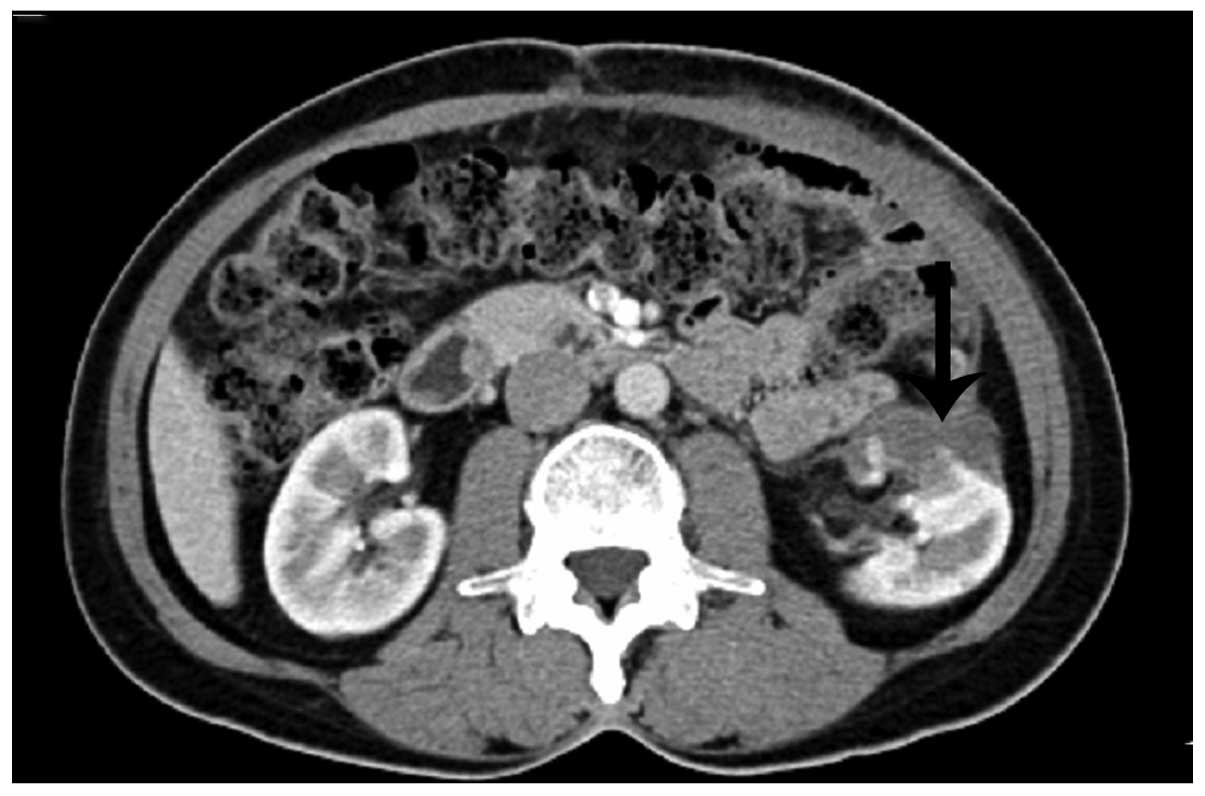
was discharged 1 week following surgery. However, 3 months
following the surgery, recurrence was observed in the remainder of
the left kidney (Fig. 3).
The Chinese Biology and Medicine Database
(sinomed.imicams.ac.cn/zh), the Chinese periodical Database of
Science and Technology (lib.cqvip.com) and the China Hospital
Knowledge Database (www.chkd.cnki.net) were searched for historical cases
of retroperitoneal liposarcoma between January 2005 and December
2014. Duplicate reports were excluded and 13 cases along with the 1
case treated in the current study were identified (Table I). Of the 8 cases with follow-up, none
have succumbed to the disease.
 | Table I.Clinical data of the 14 patients. |
Table I.
Clinical data of the 14 patients.
| First author,
year | (ref) | Gender/age | Examination | Primary or
recurrent | Size (cm) | Subtype | Surgical
treatment |
|---|
| Zhai, 2010 | (5) | M/56 | CT | Primary | 35×25×15 | WD | CR |
| Zhuang, 2009 | (6) | F/61 | CT | Primary | 30×20×12 10×10×10
8×8×8 | DD | CR |
| Liu, 2013 | (7) | F/55 | CT | Primary | 40×30×20 | WD | CR |
| Liu, 2008 | (8) | M/65 | NA | Recurrent (tenth
time) | 25×25 (the largest
one) | NA | CR + multiple
visceral organ resection |
| Chen, 2007 | (9) | F/36 | CT &
ultrasonography | Primary | 36×27×13 | WD | CR + nephrectomy |
| Liu, 2013 | (10) | F/54 | CT &
ultrasonography | Primary | >15 | Mixed | CR |
| Shen, 2009 | (11) | F/53 | CT &
ultrasonography | Primary | 20×15×10 | WD | CR |
| Xie, 2006 | (12) | M/73 | CT, MRI &
ultrasonography | Recurrent (third
time) | 25×15×8 | WD | CR |
| Xie, 2006 | (12) | F/41 | CT &
ultrasonography | Primary | 43×40×25 | WD | CR |
| Wan, 2004 | (13) | F/53 | CT &
ultrasonography | Recurrent (fourth
time) | 18×12 (the largest
one) | myxoid | CR |
| Zhen, 2011 | (14) | M/55 | CT | Primary | 40×30×20 | NA | CR + nephrectomy |
| Liu, 2012 | (15) | F/55 | MRI &
ultrasonography | Recurrent (third
time) | 20×20×20 (the largest
one) | DD | CR + sigmoid colon
resection |
| Wang, 2008 | (16) | F/52 | CT | Primary | 30×28×25 (the largest
one) | WD | CR |
| Present |
| F/48 | CT & MRI | Primary and recurs 3
months later | 30×20×15 | myxoid | CR + partial
nephrectomy |
The mean age of the 14 patients at presentation was
54.1 years (range, 36–73 years) and the male/female ratio was 2:5.
CT was the most common auxiliary examination used for diagnosis
(12/13), followed by MRI and ultrasonography. No cases were
diagnosed using preoperative biopsy. Recurrence was observed in
5/14 patients, ranging between 1 and 10 times. The liposarcoma size
ranged between 8×8×8 and 43×40×25 cm. Of the 12 cases with a
reported histological subtype, 7 were well-differentiated, 2 were
dedifferentiated, 2 were myxoid and 1 was of a mixed subtype. All
the patients underwent complete resection, of whom 5 received
additional visceral organ resection (3 nephrectomy, 1 sigmoid colon
and 1 multiple visceral organ resection). However, no patients
received chemotherapy or radiotherapy.
Discussion
Retroperitoneal tumor predominantly originates from
fat, loose connective tissue, fascia, muscles, lymphatic tissue or
residual embryonic tissue, of which 80% is malignant.
Retroperitoneal liposarcoma is the most frequently observed subtype
of retroperitoneal tumor, with an incidence of ~2.5 per million
individuals (17). It usually occurs
at 40–60 years of age, and the ratio between the genders is ~1:1
(1,18). In the review of the literature for the
present study, the mean age of the patients was 54.1 years.
The large volume of the intra-abdominal space allows
liposarcoma to grow without compressing the vital organs, resulting
in rare early diagnosis. When clinical symptoms do present, the
retroperitoneal liposarcoma has usually grown very large in size,
oppressing or invading the surrounding organs.
To differentiate from other soft tissue tumors,
auxiliary examinations are required, including ultrasonography, CT
and MRI. These examinations provide information on the tumor's
position and size, in addition to an appropriate staging of the
tumor extension and involved structures, which aids greatly in
designing a surgical scheme. Ultrasonography is usually selected
prior to CT scan and MRI for its convenience. On a CT scan,
retroperitoneal liposarcoma usually appears as a large encapsulated
mass containing variable amounts of fatty and soft tissue
components (19). MRI is important
for the diagnosis of liposarcoma invasion of the abdominal aorta or
inferior vena cava. Biopsy is not generally recommended due to the
probability of tumor seeding (20).
In the present study, the literature review reported that 12
patients received CT scans for diagnosis in the 13 cases with
available auxiliary examinations data. Ultrasonography and MRI were
also selected in a number of cases. No cases used preoperative
biopsy for diagnosis.
The final diagnosis of retroperitoneal liposarcoma
is dependent on the pathological and immunohistochemical analyses.
Liposarcoma can be histologically subdivided into 5 subtypes:
Well-differentiated, myxoid, round cell, pleomorphic and
dedifferentiated (21). Generally,
round cell, pleomorphic and dedifferentiated subtypes are regarded
as high-grade; whilst well-differentiated and myxoid liposarcoma
are low-grade (22). With the
development of pathological analysis, greater importance has been
attached to the subtypes of retroperitoneal liposarcoma. High
histological grade is one of the most important negative prognostic
factors in patients with retroperitoneal liposarcoma.
Well-differentiated liposarcomas may recur locally, but the
metastatic potential is low, while pleomorphic liposarcomas have
high metastatic potential, which may reduce the survival rate
(22).
With regards to the high recurrence rate of
liposarcoma, the standardization of the original surgery becomes
particularly important. Complete resection is the predominant
treatment. The principle of the surgery is to resect the tumor and
any invaded organs without any residue of the liposarcoma or
membrane remaining. Successful complete resection of
retroperitoneal liposarcoma may increase the 5-year survival rate
from 16.7 to 58% (23). However,
complete resection is a challenge, particularly in the
well-differentiated subtype, for the reason that the margins are
not easily distinguishable (24).
Combined resection is occasionally required to achieve macroscopic
clearance; the kidney is the most commonly removed organ, followed
by the colon (24). In the present
study, all the patients underwent complete resection, of whom 5
received additional visceral organ resection (3 nephrectomy, 1
sigmoid colon and 1 multiple visceral organs). In the present case,
the liposarcoma invaded the left renal capsule and was completely
macroscopically removed. Regardless, recurrence was observed. This
raises the question: Should the management of the liposarcoma in
the present case have been more aggressive? Should the whole kidney
be resected rather than the renal capsule and part of the kidney
(if the renal function of the contralateral kidney is sufficient)?
Certain previous studies support the above argument and indicate
that if the liposarcoma invaded the kidney, then combined resection
of the kidney is necessary (9,25). There
is no evidence that chemotherapy or radiotherapy improve survival
rates (26). In the present study, no
patients in the studied literature were administered chemotherapy
or radiotherapy.
Even with complete removal of the liposarcoma,
prognosis remains poor. The 5-year survival rate of
well-differentiated retroperitoneal liposarcoma is 83%, while it is
20% for the dedifferentiated tumor subtype (22). The total recurrence rate was 5/14
patients in the present literature review and the recurrence
frequency ranged between 1 and 10 times. Local recurrence remains
the preliminary cause of mortality in retroperitoneal liposarcoma
(27). The survival rate was improved
in the patients who received a complete resection of their
recurrent tumor compared with the patients who did not. Therefore,
the gold standard treatment remains to be removal of the recurrence
(25). The difficulty of the
secondary operation is that the anatomical relationship would be
more complex. The reason for this is that after the initial
surgery, the anatomical position would have altered and the tissues
may adhere to one another or to important vessels, resulting in the
increased difficulty of the secondary surgery. Combined resection
of the surrounding organs may be unavoidable when attempting to
achieve complete resection. The purpose of the secondary operation
is to remove the tumor, in addition to relieving the compression of
vital viscera. When radical surgery is not possible, palliative
resection is advisable. In order to detect recurrence, a CT scan
every 3 months for the first 2 years, every 6 months for 2–5 years
and annually thereafter is generally recommended.
In conclusion, retroperitoneal liposarcoma is a rare
disease with a high rate of recurrence. Complete resection is the
benchmark for treatment, however the combined resection of adjacent
organs is occasionally necessary. The present study reports a case
of giant retroperitoneal liposarcoma and puts it into context with
previously reported cases in the literature; in addition to the
authors experience of the surgery, in order to summarize the
standard therapy.
References
|
1
|
Mendenhall WM, Zlotecki RA, Hochwald SN,
Hemming AW, Grobmyer SR and Cance WG: Retroperitoneal soft tissue
sarcoma. Cancer. 104:669–675. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Russell WO, Cohen J, Enzinger F, et al: A
clinical and pathological staging system for soft tissue sarcomas.
Cancer. 40:1562–1570. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bradley JC and Caplan R: Giant
retroperitoneal sarcoma: A case report and review of the management
of retroperitoneal sarcomas. Am Surg. 68:52–56. 2002.PubMed/NCBI
|
|
4
|
Fabre-Guillevin E, Coindre JM, Somerhausen
NS, Bonichon F, Stoeckle E and Bui NB: Retroperitoneal
liposarcomas: follow-up analysis of dedifferentiation after
clinicopathologic reexamination of 86 liposarcomas and malignant
fibrous histiocytomas. Cancer. 106:2725–2733. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhai HX, Ma XM and Jia QQ: A case report
of giant retroperitoneal liposarcoma. Chin Community Doct.
12:167–168. 2010.(In Chinese).
|
|
6
|
Zhuang GY, Dong CW, Li JQ and Li MJ:
Multiple retroperitoneal dedifferentiated liposarcoma: a case
report. Chin J Curr Adv Gen Surg. 12:89–90. 2009.(In Chinese).
|
|
7
|
Liu B, Wang QF, Yu JH, Wang DG, Zhang Y
and Xu YC: Giant abdominal liposarcoma: a case report. Chin J
Gerontol. 33:4522013.(In Chinese).
|
|
8
|
Liu CL and Zhang HY: Multiple
retroperitoneal and abdominal liposarcoma: a case report. Chin J
Gen Surg. 23:3202008.(In Chinese).
|
|
9
|
Chen RF and Peng DT: Giant retroperitoneal
liposarcoma: a case report. Chin J Dig Surg. 6:3802007.(In
Chinese).
|
|
10
|
Liu CZ, Xin H, Li GD and Wang LL: Giant
retroperitoneal liposarcoma: a case report. Jilin Med J.
34:5535–5536. 2013.(In Chinese).
|
|
11
|
Shen Y, He XJ, Li Y, Lv RG and Li P: Giant
retroperitoneal liposarcoma: a case report. The Journal of
Practical Medicine. 25:5162009.(In Chinese).
|
|
12
|
Xie M, Zeng QL and Wen KM: Giant
retroperitoneal liposarcoma: experiences in diagnosis and treatment
of two cases. Guizhou Med J. 30:30–31. 2006.(In Chinese).
|
|
13
|
Wan HM, Li LS, Zhang G and Wang ZY:
Resection of giant retroperitoneal liposarcoma for the 4th time: a
case report. Chin J Prac Surg. 24:4362004.(In Chinese).
|
|
14
|
Zheng SW, Wang SL and An WK: Giant
retroperitoneal liposarcoma: a case report. Clin J Med Offic.
39:3332011.(In Chinese).
|
|
15
|
Liu J, Bai YC, Zhang YX, Sun Y and Zhang
MZ: Multiple giant retroperitoneal liposarcoma: a case report. Prac
J Med & Pharm. 29:2922012.(In Chinese).
|
|
16
|
Wang XH and Wang HG: Giant retroperitoneal
liposarcoma. Chin Med Her. 5:1182008.(In Chinese).
|
|
17
|
Neuhaus SJ, Barry P, Clark MA, Hayes AJ,
Fisher C and Thomas JM: Surgical management of primary and
recurrent retroperitoneal liposarcoma. Br J Surg. 92:246–252. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mack TM: Sarcomas and other malignancies
of soft tissue, retroperitoneum, peritoneum, pleura, heart,
mediastinum, and spleen. Cancer. 75:(Suppl). 211–244. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chang IY and Herts BR: Retroperitoneal
liposarcoma. J Urol. 189:1093–1094. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Clark MA and Thomas JM: Portsite
recurrence after laparoscopy for staging of retroperitoneal
sarcoma. Surg Laparosc Endosc Percutan Tech. 13:290–291. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Singer S, Antonescu CR, Riedel E and
Brennan MF: Histologic subtype and margin of resection predict
pattern of recurrence and survival for retroperitoneal liposarcoma.
Ann Surg. 238:358–371. 2003.PubMed/NCBI
|
|
22
|
Nijhuis PH, Sars PR, Plaat BE, Molenaar
WM, Sluiter WJ and Hoekstra HJ: Clinico-pathological data and
prognostic factors in completely resected AJCC stage I-III
liposarcomas. Ann Surg Oncol. 7:535–543. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lee SY, Goh BK, Teo MC, et al:
Retroperitoneal liposarcomas: the experience of a tertiary Asian
center. World J Surg Oncol. 9:122011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chen ZH and Song XM: The theraputic
progress in retroperitoneal liposarcoma. Chin J Gen Surg. 24:81–83.
2009.(In Chinese).
|
|
25
|
Bautista N, Su W and O'Connell TX:
Retroperitoneal soft-tissue sarcomas: Prognosis and treatment of
primary and recurrent disease. Am Surg. 66:832–836. 2000.PubMed/NCBI
|
|
26
|
Perez EA, Gutierrez JC, Moffat FL Jr, et
al: Retroperitoneal and truncal sarcomas: prognosis depends upon
type not location. Ann Surg Oncol. 14:1114–1122. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Milone M, Pezzullo LS, Salvatore G,
Pezzullo MG, Leongito M, Esposito I and Milone F: Management of
high-grade retroperitoneal liposarcomas: personal experience.
Updates Surg. 63:119–124. 2011. View Article : Google Scholar : PubMed/NCBI
|