Introduction
Lung cancer is one of the most frequently diagnosed
types of cancer and is the leading cause of cancer-associated
mortality worldwide (1). In China,
the incidence and mortality rate of lung cancer have been
increasing dramatically in the previous three decades and lung
cancer is becoming a notable medical problem (2). Pulmonary atelectasis is a common
complication in patients with lung cancer, particularly central
type lung cancer. It has been reported that 30% of lung cancer
patients present with obstruction of the central airway, such as
the trachea or main bronchi, which manifests as symptoms of
respiratory distress, bleeding or infection (3). Pulmonary atelectasis decreases quality
of life (QOL) and may impair anti-tumor therapy. Due to a low
possibility for resection, palliative therapy plays an important
role in this condition. Currently, a variety of interventional
modalities, including neodymium-doped yttrium aluminium garnet
laser therapy, stenting, photo-dynamic therapy and endoluminal
brachytherapy, are utilized to relieve airway obstruction, owing to
the development of the flexible bronchoscope. Therapy choice
depends on the presence of comorbidities, pulmonary function of the
patient, previous treatment administered and life expectancy of the
patient. High-dose-rate (HDR) endoluminal brachytherapy, with or
without additional combined therapy, has been demonstrated to be an
effective treatment modality in this condition (4,5). However,
due to the high expenses of HDR endoluminal brachytherapy, the
application of this technology has been tremendously restricted. As
a type of novel therapy technology, 125I radioactive
seed implantation has been revealed as efficient in numerous types
of malignant tumors (6,7).
The present study aimed to evaluate the feasibility,
safety and efficacy of low-dose-rate (LDR) interstitial
brachytherapy trans-bronchoscopy with 125I radioactive
seed implantation in patients with pulmonary atelectasis induced by
lung cancer. To the best of our knowledge, the present study is the
first to evaluate the feasibility, safety and efficacy of LDR
125I seed implantation as a palliative therapy in
patients with malignant obstructive pulmonary atelectasis induced
by lung cancer.
Patients and methods
Patient eligibility and
characteristics
Between April 2008 and June 2011, 15 patients with
central type lung cancer and secondary obstructive pulmonary
atelectasis underwent interventional bronchoscopy with
125I implantation for symptomatic palliation of
pulmonary atelectasis at either the Department of Oncology, Guizhou
Astronautics Hospital (Zunyi, Guizhou, China) or the Department of
Imaging and Intervention Radiology, Cancer Center of Sun Yat-sen
University (Guangzhou, Guangdong, China). All patients were
diagnosed with primary lung cancer involving the central airway,
which was confirmed by biopsy, and were not candidates for surgical
resection. All patients had previously received chemotherapy at
least four times, with a poor response rate (RR). Three patients
had received prior radiation therapy at a dose between 40 and 50
Gy, at a conventional fractionation. The other patients did not
undergo external beam radiation therapy due to numerous causes.
Pre-operative evaluation and treatment decision making was based on
the health of the patients, previous bronchoscopy exam, computed
tomography (CT) scan, previous therapy and the willingness of
patients. The patients consisted of 15 patients with airway
obstructive atelectasis that presented with various symptoms, such
as respiratory distress, cough, hemoptysis and pneumonia. All
patients presented with a cough and respiratory distress, and 9
patients (60%) presented with hemoptysis. Squamous cell carcinoma
was the most common histological diagnosis in 11 patients. The
patient characteristics are reported in Table I. Symptoms of acute obstruction and
medium to severe hemoptysis were considered unsuitable for the
present study and patients exhibiting these symptoms were excluded
from the study.
 | Table I.Background characteristics of patients
before 125I seed implantation (n=15). |
Table I.
Background characteristics of patients
before 125I seed implantation (n=15).
| Patient
characteristic | Value |
|---|
| Gender, n (%) |
|
| Male | 11 (73.3) |
|
Female | 4 (26.7) |
| Age, years |
|
|
Median | 62.1 |
|
Range | 43-80 |
| Pathology type,
n |
|
| Squamous
cell cancer | 12 |
|
Adenocarcinoma cell
cancer | 3 |
| Main clinical
presentation, n |
|
|
Respiratory distress | 15 |
|
Cough | 15 |
|
Bleeding | 9 |
|
Infection | 5 |
|
Other | 11 |
| Obstructive location,
n |
|
| Right
bronchus | 10 |
| Left
bronchus | 5 |
| Clinical stage,
n |
|
| IIIA | 2 |
| IIIB | 5 |
| IV | 8 |
| Previous therapy,
n |
|
|
Chemotherapy | 15 |
| External
beam radiotherapy | 3 |
Pre-operative preparation and surgical
procedure
The present study used 0.7 mCi 125I
radioactive seeds (catalog no., CIAE-6711; Chinese Atomic Energy
Science Institution, Beijing, China). The dose of the radioactive
seeds was determined according to the following empirical formula:
Total dose (mCi) = (length + width + height) / 3 × 5. The number of
seeds was calculated as follows: Number of seeds = total dose /
0.7. The prescription dose determined from this formula was
expected to reach 100–130 Gy. The endoscope was obtained from
Olympus (BF-IT40; Olympus Corporation, Tokyo, Japan).
Implantation of 125I
seeds
The technique for this therapy was, overall, the
same as regular bronchoscope examination (8). All procedures were performed under
airway topical anesthesia with monitoring of electrocardiogram,
pulse, blood pressure and blood oxygen saturation. A unilateral
nasal catheter was placed prior to the procedure for the purpose of
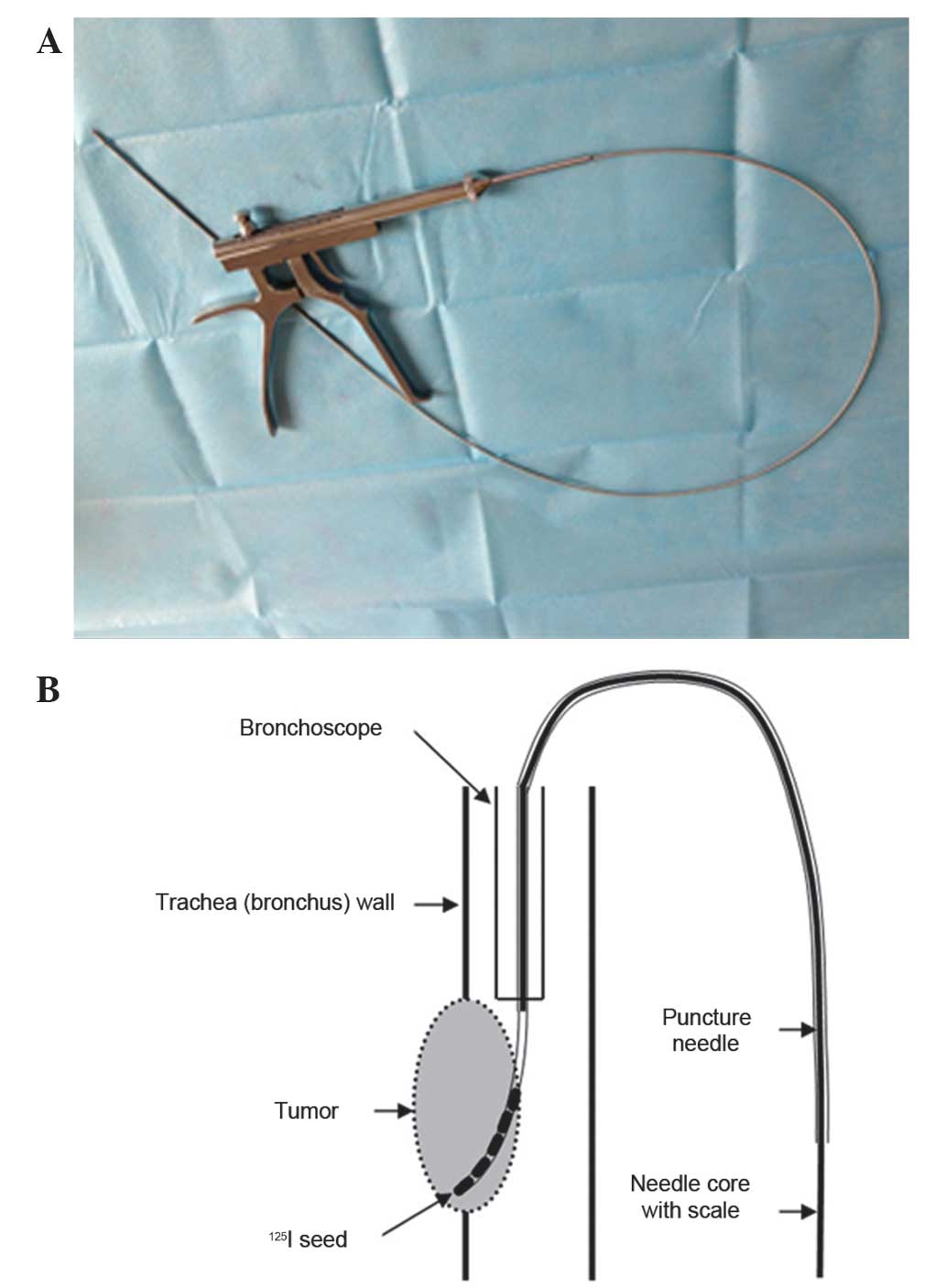
oxygen supply. Using a specialized instrument (Endoscope with
particle pusher; Innovative Medical Device Technology Co., Ltd.
Jinan, Shandong, China; Fig. 1), a
channel was created to implant the radioactive seeds into the
tumor.
Monitoring of patients
All 15 patients that underwent this therapy were
followed up clinically or by telephone, and surveillance
bronchoscopy and CT scans were performed two months subsequent to
the first procedure and every subsequent two months. At each
follow-up, the patients were clinically evaluated through a
thorough history and physical examination, and the patients were
assessed to determine their Karnofsky performance status (KPS)
score. Additional bronchoscopies and CT scans were performed based
upon the symptoms of the patients.
Assessment of the efficacy of
pulmonary atelectasis reopening
Assessment of pulmonary reopening was based on the
follow-up CT scan, and the CT image was evaluated by two
independent radiologists. The efficacy was defined as follows:
Complete reopening (CR), lung expansion had returned to the normal
size and there was no atelectasis residue; partial reopening (PR),
lung expansion was partial and the maximum diameter of pulmonary
atelectasis was reduced by >50%; and no reopening (NR), lung
expansion was not evident, or the maximum diameter of pulmonary
atelectasis reduced <50% and progressed <20%. Progressive
disease (PD) was defined as the maximum diameter of pulmonary
atelectasis increasing by >20%.
Assessment of QOL
Data from the assessment of the QOL of all patients
was obtained using the KPS score. KPS measurements range between 0
and 100. A high score represents a high QOL. The KPS scores were
determined by clinicians prior to trans-bronchoscopy with
implantation of 125I radioactive seeds, and again at
each subsequent follow-up.
Statistical analysis
Statistical analysis was performed using SPSS
software, version 13.0 (SPSS Inc., Chicago, IL, USA). The survival
time was calculated from the time between the date of the procedure
and time of mortality. Survival was calculated using the
Kaplan-Meier method, and KPS data were analyzed using a
paired-samples t-test. P<0.05 was considered to indicate
a statistically significant difference.
Ethical approval and patient
consent
Ethical approval was obtained prior to the
commencement of the study from the Ethical Committee of the Sun
Yat-sen University Cancer Center and the Ethical Committee of
Guizhou Astronautics Hospital. The present study was performed in
accordance with national law and the Helsinki Declaration of 1975,
in its current, revised form (9).
Written informed consent was obtained from all patients prior to
the commencement of the treatment procedure.
Results
Technical feasibility
The present study enrolled 15 patients, 11 male and
4 female, with a median age of 62.1 years. A total of 15
interventional bronchoscopies were performed. The procedure time
ranged between 20 and 50 min, with an overall average duration of
35 min. The present study was easily performed and was well
tolerated by all patients. No procedure-associated mortalities
occurred and no patient required a prompt discontinuation of the
surgical procedure.
Complications
No patient succumbed to disease within 30 days of
the initial procedure. An irritable cough and temporary increase of
hemoptysis occurred in 11 (73.3%) and 10 (66.7%) patients,
respectively, and were the most common complications. Other
complications, including chest pain and fever, were mild and
considered acceptable. No patients required additional emergency
bronchoscopic treatment subsequent to the initial intervention.
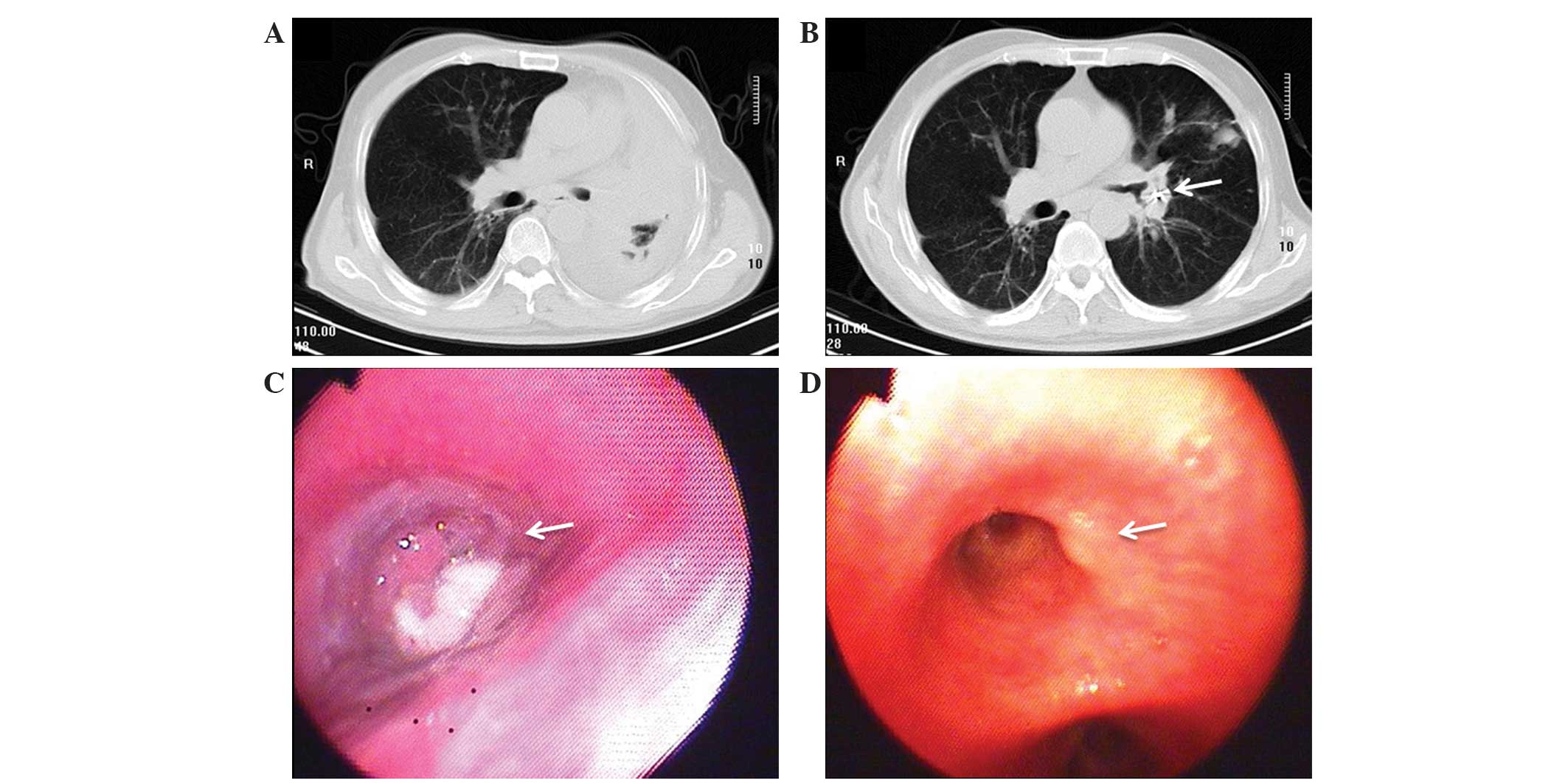
Pulmonary atelectasis control
Overall, lung reopening was observed in the majority
of patients between the procedure and the last follow-up. The
reopening rate, calculated as the sum of the CR and PR, was 86.7,
76.9, 80.0, 75.0 and 50.0% in patients at 2, 6, 12, 18 and 24
months, respectively. The pulmonary atelectasis control rate is
reported in Table II. A typical case
is illustrated in Fig. 2.
 | Table II.The effect of trans-bronchoscope
125I radioactive seeds implantation for the treatment of
atelectasis in 15 patients with central type lung cancer. |
Table II.
The effect of trans-bronchoscope
125I radioactive seeds implantation for the treatment of
atelectasis in 15 patients with central type lung cancer.
|
|
| Reopening of
atelectasis |
|
|---|
|
|
|
|
|
|---|
| Follow-up time,
months | Patients, n | CR | PR | NR | PD | Reopening rate,
% |
|---|
| 2 | 15 | 5 | 8 | 2 | 0 | 86.7 |
| 6 | 13 | 3 | 7 | 2 | 1 | 76.9 |
| 12 | 10 | 2 | 6 | 1 | 1 | 80.0 |
| 18 | 8 | 2 | 4 | 1 | 1 | 75.0 |
| 24 | 4 | 1 | 1 | 2 | 0 | 50.0 |
QOL response
The majority of the patients demonstrated an
improvement in KPS scores subsequent to the surgery, particularly
in those with a lower KPS score prior to the procedure. The
improvement in symptoms and feeling of well-being was observed 2–3
weeks subsequent to the procedure and was maintained until the
final follow-up in the majority of patients. In addition, there was
a significant improvement in the pre- and post-operative KPS
scores. The mean KPS score was 72.3±5.6 prior to the procedure and
was improved to 84.7±4.8 one month later (P=0.004; Table III).
 | Table III.KPS scores for the 15 patients pre-
and post-implantation of 125I radioactive seeds. |
Table III.
KPS scores for the 15 patients pre-
and post-implantation of 125I radioactive seeds.
|
|
|
| KPS score |
|---|
|
|
|
|
|
|---|
| Patient number | Gender | Age, years |
Pre-implantation | 1-month
follow-up | 2-month
follow-up | 6-month
follow-up | 1-year
follow-up | 2-year
follow-up |
|---|
| 1 | M | 65 | 65 | 75 | 80 | 80 | – |
|
| 2 | M | 64 | 70 | 80 | 80 | 85 | 80 | – |
| 3 | M | 60 | 60 | 85 | 85 | 85 | 80 | 85 |
| 4 | M | 63 | 70 | 80 | 80 | 80 | 75 |
|
| 5 | M | 46 | 75 | 85 | 80 | 80 | 80 | – |
| 6 | M | 72 | 80 | 90 | 90 | – |
|
|
| 7 | M | 69 | 75 | 90 | 90 | 85 | 80 | – |
| 8 | M | 80 | 75 | 90 | 85 | – |
|
|
| 9 | M | 60 | 70 | 80 | 85 | 80 | – |
|
| 10 | M | 43 | 70 | 85 | 90 | 80 | 80 | – |
| 11 | F | 57 | 70 | 85 | 90 | 90 | 80 | – |
| 12 | F | 63 | 75 | 85 | 85 | 85 | 85 | 80 |
| 13 | F | 67 | 80 | 90 | 85 | 85 | 80 | – |
| 14 | F | 54 | 80 | 90 | 90 | 80 | – |
|
| 15 | F | 68 | 70 | 80 | 85 | 80 | 80 | – |
| Mean ± SD |
| 62.1±9.5 | 72.3±5.6 | 84.7±4.8 | 85.4±4.0 | 82.7±4.3 | 80.0±2.4 | 82.5±3.5 |
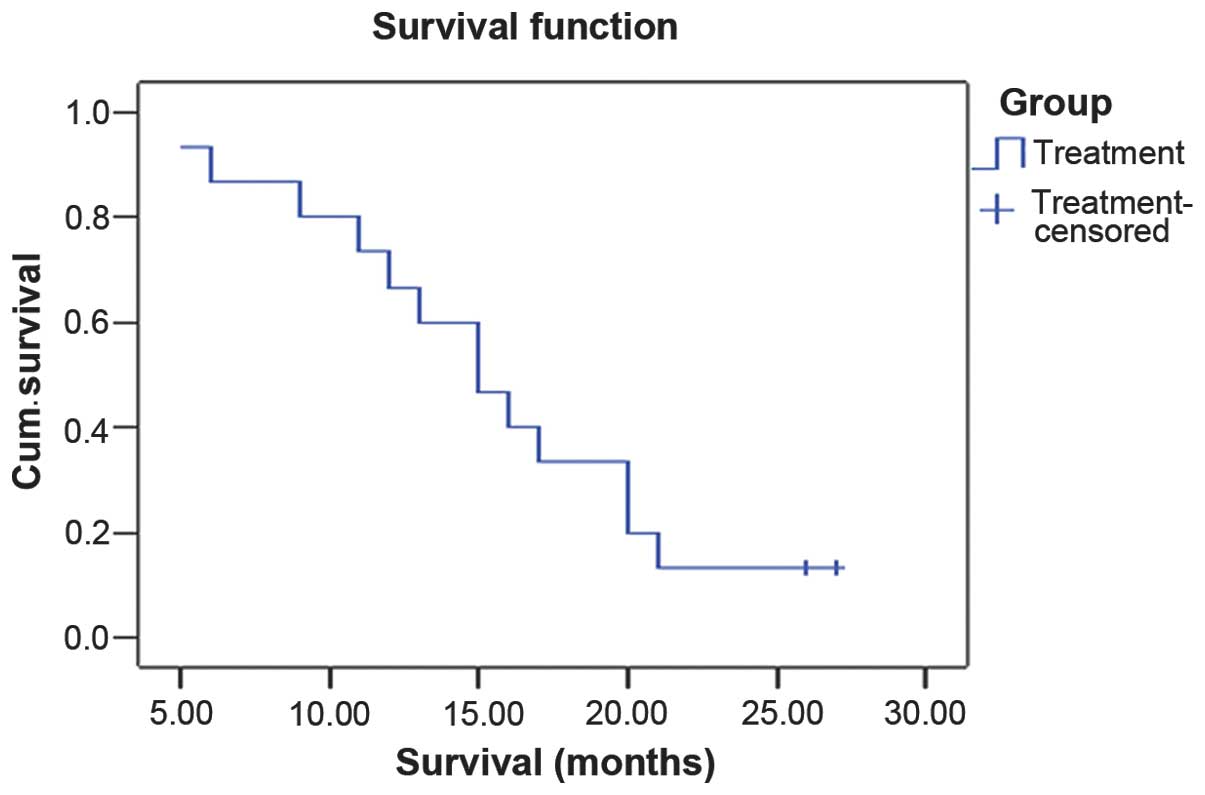
Survival analysis
The median follow-up time was 20.8 months (range,
5–27). The median survival time was 15.6 months, and the survival
rate was 86.7% at 6 months, 66.7% at 12 months and 13.3 at 24
months subsequent to the procedure (Fig.
3).
At the time of analysis, 13 patients had succumbed.
Nine patients had succumbed to progressive disease, including
locoregional progression and brain metastasis, two patients had
succumbed to a brain-vascular accident, one of which possessed a
history of hypertension, one patient with a history of coronary
artery disease succumbed to sudden cardiac arrest, and one patient
with a history of COPD experienced heart failure. The
characteristics of the 125I seed implantation and
outcome of the treatment with 125I seed implantation is
reported in Table IV.
 | Table IV.Characteristics of the patients that
underwent 125I seed implantation and the outcome of the
treatment. |
Table IV.
Characteristics of the patients that
underwent 125I seed implantation and the outcome of the
treatment.
|
|
|
| Treatment and
follow-up result |
|---|
|
|
|
|
|
|---|
| Patient number | Gender | Age, years | Pathology | Clinical stage | Seeds, n | Alive | Survival time,
months | Cause of
mortality | Medical
history |
|---|
| 1 | M | 65 | SC | IV | 10 | No | 9 | Heart failure | COPD |
| 2 | M | 64 | SC | IV | 9 | No | 16 | Brain
metastases | Diabetes |
| 3 | M | 60 | SC | IIIA | 6 | Yes | >26 | – |
|
| 4 | M | 63 | SC | IV | 8 | No | 13 | CVD | Coronary
disease |
| 5 | M | 46 | SC | IIIB | 8 | No | 21 | Tumor
progression |
|
| 6 | M | 72 | SC | IV | 8 | No | 6 | Brain
metastases | COPD |
| 7 | M | 69 | SC | IV | 10 | No | 15 | Brain
metastases | Diabetes |
| 8 | M | 80 | SC | IV | 10 | No | 5 | AMI | COPD, diabetes |
| 9 | M | 60 | SC | IIIB | 9 | No | 15 | Tumor
progression |
|
| 10 | M | 43 | SC | IV | 12 | No | 11 | Brain
metastases |
|
| 11 | F | 57 | SC | IIIA | 10 | No | 20 | Tumor
progression | Diabetes |
| 12 | F | 63 | AC | IIIB | 7 | Yes | >27 | – |
|
| 13 | F | 67 | AC | IIIB | 11 | No | 17 | Tumor
progression | Hypertension |
| 14 | F | 54 | SC | IV | 13 | No | 12 | Brain
metastases |
|
| 15 | F | 68 | AC | IIIB | 14 | No | 20 | Tumor
progression |
|
Discussion
Lung cancer remains the leading cause of cancer
mortality worldwide, and only 25–30% of patients with non-small
cell lung cancer present with locally-advanced disease on initial
diagnosis, whereas 40–50% present with metastatic disease (1,10).
Although the majority of the patients with inoperable lesions
experience clinical benefit subsequent to receiving chemotherapy,
radiotherapy and even targeted therapy, the overall survival (OS)
rate remains suboptimal, with a five-year survival rate of <1%
(11). The overall survival time was
8–10 months and the one-year survival rate was 30–35% (12). The majority of patients with lung
cancer eventually require palliative treatment (13). Obstruction of the central airway is
frequently encountered in patients with inoperable lung cancer, and
may be caused by an intraluminal tumor growth, extrinsic
compression or weakness of the bronchial wall. A variety of
bronchoscopic techniques are currently available for the management
of malignant obstruction of the central airway (14). For all these bronchoscopic techniques,
several studies have reported excellent palliation with varying
rates of complications in patients treated with endobronchial
brachytherapy (15,16).
For locally advanced lung cancer, there are several
studies (17–19) that have demonstrated the effectiveness
of 125I radioactive seeds implantation in the local
control and improvement of OS time and rate. However, for central
type lung cancer, the technique of percutaneous puncture means
great risk of hemorrhage and pneumothorax. However, the development
of the technology used in interventional bronchoscopy makes the
trans-bronchoscopy procedure with 125I radioactive seed
implantation possible and flexible. In the present study, all 15
patients completed this therapy safely. The procedure time was
20–50 min, with an average duration of 35 min in all patients, and
there was no procedure-associated mortality. The present result
revealed that this technique is safe and flexible.
Complications of HDR intraluminal brachytherapy are
mild and infrequently reported in the majority of previous studies,
while severe complications, such as fatal hemoptysis and
broncho-esophageal fistula, were occasionally observed (15,20,21).
Therefore, the adverse effects of HDR brachytherapy on the airways
are more thoroughly considered. Compared with HDR, LDR demonstrates
an improved relative biological effect (RBE) (22,23). The
present results revealed that the treatment complications were mild
and acceptable, mainly presenting as a transient increase in
hemoptysis, chest pain and fever. However, the duration of the
complications was short and the majority of patients did not
require additional therapy. There were no severe complications
compared with those reported for HDR intraluminal brachytherapy.
Probable explanations include that LDR has more excellent radiation
biology characteristics compared with that of HDR. LDR
brachytherapy is a type of continuous therapy with reduced peak
dose. In addition, HDR intracavitary therapy requires several
surgical procedures, and this increases the risk of complications.
Notably, in the current study, one patient expelled two radioactive
seeds two weeks subsequent to the procedure. This case resulted in
certain requirements for radiological safety. Therefore, a small
lead bottle was prepared for each patient in the present study to
store any seeds that were coughed out so that the radioactive seeds
would not harm the environment or other individuals.
The atelectasis reopening rate, calculated from the
sum of the CR and PR, was revealed to be 86.7, 76.9, 80.0, 75.0 and
50.0% in patients at 2, 6, 12, 18 and 24 months subsequent to the
procedure, respectively. Compared with a previous study (20), the atelectasis recanalization effect
was good, and the effect was similar between the two studies, but
demonstrated a longer duration in the present study. A possible
reason is that the implantation of 125I radioactive
seeds by intraluminal brachytherapy has a longer therapeutic effect
compared with HDR intraluminal brachytherapy. The majority of
patients in the present study demonstrated an improved KPS score
subsequent to the surgical procedure. The mean KPS score was
72.3±5.6 prior to the procedure and improved to 84.7±4.8 one month
later (P=0.004). Intraluminal brachytherapy with 125I
radioactive seed implantation has a longer therapeutic effect,
which may be an explanation for the comparatively long duration of
the improvement in KPS.
In the present study, the long-term survival of lung
cancer was the ultimate treatment goal. The median survival was
15.6 and the survival rate was 86.7% at 6 months subsequent to the
procedure, 66.7% at 12 months and 13.3% at 24 months. The two-year
survival rate was lower in the current study compared with certain
studies of HDR intraluminal brachytherapy (5,24). This
difference may be a result of patient selection or additional
therapy, as numerous intraluminal brachytherapy procedures were
combined with external radiation treatment. In the present study,
eight patients presented with stage IV disease. Therefore, a
two-year survival rate of 13.3% is a favorable outcome. However,
the present study also demonstrated certain limitations. Firstly,
accurate measurement of the dosimetry of the irradiation was not
possible due to the lack of sophisticated measuring techniques
dedicated to this condition. Therefore, no quantitative data
associated with radiation therapy could be provided. Secondly,
pulmonary atelectasis is occasionally challenging to differentiate
from the tumor, so the present study cannot supply accurate data
for local tumor control. Thirdly the current study was not a
randomized trial and, as a pilot study, only 15 patients were
approved to receive the therapy.
Management of malignant tumor complicated with
pulmonary atelectasis is a challenging issue. Interventional
bronchoscopy with a multimodality approach may improve symptom
control and survival. This study demonstrated that
trans-bronchoscopy with 125I radioactive seed
implantation is a feasible procedure that demonstrates good symptom
control, minimal complications and improvement in survival and QOL.
Physicians treating such patients should recognize the limitation
of single modality therapy and become skilled in utilizing
alternative complementary treatment approaches in order to achieve
optimal outcome.
Acknowledgements
This study was supported by the Provincial &
Ministry of Education Research Project of Guangdong (grant no.,
2012B091100458), Major Project of Science and Technology of
Guangzhou (grant no., 132400027) and National Natural Science
Foundation of China (grant no., 81371654). The authors thank Dr.
Marcin Bednarz and Dr. Zou Fang for their kind help with the
English language.
References
|
1
|
Jemal A, Bray F, Center MM, et al: Global
cancer statistics. CA Cancer J Clin. 61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Au WW, Su D and Yuan J: Cigarette smoking
in China: Public health, science, and policy. Rev Environ Health.
27:43–49. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cavaliere S, Venuta F, Foccoli P, et al:
Endoscopic treatment of malignant airway obstructions in 2,008
patients. Chest. 110:1536–1542. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Niemoeller OM, Pöllinger B, Niyazi M, et
al: Mature results of a randomized trial comparing two
fractionation schedules of high dose rate endoluminal brachytherapy
for the treatment of endobronchial tumors. Radiat Oncol. 8:82013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aumont-le Guilcher M, Prevost B, Sunyach
MP, et al: High-dose-rate brachytherapy for non-small-cell lung
carcinoma: A retrospective study of 226 patients. Int J Radiat
Oncol Biol Phys. 79:1112–1116. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Taira AV, Merrick GS, Galbreath RW, et al:
Long-term outcomes of prostate cancer patients with Gleason pattern
5 treated with combined brachytherapy and external beam
radiotherapy. Brachytherapy. 12:408–414. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Guo JH, Teng GJ, Zhu GY, et al:
Self-expandable esophageal stent loaded with 125I seeds:
Initial experience in patients with advanced esophageal cancer.
Radiology. 247:574–581. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
British Thoracic Society Bronchoscopy
Guidelines Committee, a Subcommittee of Standards of Care Committee
of British Thoracic Society, . British Thoracic Society guidelines
on flexible bronchoscopy. Thorax. 56:(Suppl 1). i1–i21. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
World Medical Association, . World Medical
Association Declaration of Helsinki: Ethical principles for medical
research involving human subjects. JAMA. 310:2191–2194. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Novello S and Le Chevalier T: Chemotherapy
for non-small-cell lung cancer. Part 1: Early-stage disease.
Oncology (Williston Park). 17:357–364. 2003.PubMed/NCBI
|
|
11
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Schiller JH, Harrington D, Belani CP, et
al: Eastern Cooperative Oncology Group: Comparison of four
chemotherapy regimens for advanced non-small-cell lung cancer. N
Engl J Med. 346:92–98. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tishelman C, Petersson LM, Degner LF and
Sprangers MA: Symptom prevalence, intensity, and distress in
patients with inoperable lung cancer in relation to time of death.
J Clin Oncol. 25:5381–5389. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gorden JA and Ernst A: Endoscopic
management of central airway obstruction. Semin Thorac Cardiovasc
Surg. 21:263–273. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mallick I, Sharma SC and Behera D:
Endobronchial brachytherapy for symptom palliation in non-small
cell lung cancer - analysis of symptom response, endoscopic
improvement and quality of life. Lung Cancer. 55:313–318. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Escobar-Sacristán JA, Granda-Orive JI,
Gutiérrez Jiménez T, et al: Endobronchial brachytherapy in the
treatment of malignant lung tumours. Eur Respir J. 24:348–352.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Niu L, Zhou L, Xu K and Mu F: Combination
of cryosurgery and Iodine-125 seeds brachytherapy for lung cancer.
J Thorac Dis. 4:504–507. 2012.PubMed/NCBI
|
|
18
|
Zhang S, Zheng Y, Yu P, et al: The
combined treatment of CT-guided percutaneous 125I seed
implantation and chemotherapy for non-small-cell lung cancer. J
Cancer Res Clin Oncol. 137:1813–1822. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang ZM, Lu J, Liu T, et al: CT-guided
interstitial brachytherapy of inoperable non-small cell lung
cancer. Lung Cancer. 74:253–257. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kubaszewska M, Skowronek J, Chicheł A and
Kanikowski M: The use of high dose rate endobronchial brachytherapy
to palliate symptomatic recurrence of previously irriadiated lung
cancer. Neoplasma. 55:239–245. 2008.PubMed/NCBI
|
|
21
|
Ozkok S, Karakoyun-Celik O, Goksel T, et
al: High dose rate endobronchial brachytherapy in the management of
lung cancer: response and toxicity evaluation in 158 patients. Lung
Cancer. 62:326–333. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang J, Wang J, Liao A, et al: The direct
biologic effects of radioactive 125I seeds on pancreatic
cancer cells PANC-1, at continuous low-dose rates. Cancer Biother
Radiopharm. 24:409–416. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Liao A, Wang J, Wang J, et al: Relative
biological effectiveness and cell-killing efficacy of continuous
low-dose-rate 125I seeds on prostate carcinoma cells in
vitro. Integr Cancer Ther. 9:59–65. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hennequin C, Bleichner O, Trédaniel J,
Quero L, Sergent G, Zalcman G and Maylin C: Long-term results of
endobronchial brachytherapy: A curative treatment? Int J Radiat
Oncol Biol Phys. 67:425–430. 2007. View Article : Google Scholar : PubMed/NCBI
|