Introduction
Paraganglioma, which is also referred to as
extra-adrenal pheochromocytoma, is an uncommon type of
neuroendocrine neoplasm with an estimated incidence rate of 3 per
million population; in addition, paragangliomas have been observed
in patients of all age-groups (1).
Paragangliomas are known to occur at the base of the skull base and
neck as well as within the mediastinum and periaortic region. It is
estimated that ~10% of all paragangliomas are malignant and
metastasize at sites where chromaffin tissue is rarely observed
(2,3).
In the genitourinary tract, the urinary bladder is the primary site
for paragangliomas (79.2%), followed by the urethra (12.7%), pelvis
(4.9%) and ureter (3.2%) (3,4). In addition, urinary bladder
paragangliomas account for 0.06% of all bladder tumors and 6% of
extra-adrenal pheochromocytomas (5).
Paragangliomas of the bladder present with the
clinical symptoms of pheochromocytoma, which include headaches,
palpitations and fainting as a result of the induction of
catecholamine release from functional bladder paragangliomas when
urinating (6). A proportion of
patients present with the clinical symptoms of bladder tumors, such
as hematuria. Out of these urinary bladder paragangliomas, 10–15%
are non-functioning and a further 10% have hormonal activities that
do not manifest clinically. Therefore, these paragangliomas are
occasionally diagnosed incorrectly; thus, surgeons are unprepared
and the surgery to remove paragangliomas may result in an
intraoperative hypertensive crisis and increase the mortality rate
(7).
Several reviews have been published on
paragangliomas of the urinary bladder (8,9); however,
non-functioning paragangliomas of the urinary bladder have rarely
been reported (10). The present
study reports the case of an asymptomatic patient with
non-functioning paraganglioma of the bladder, which was detected as
a mass on urinary ultrasonography scans.
Case report
Written informed consent was obtained from the
patient prior to the publication of this case report and any
accompanying images.
The bladder mass of a 61-year-old male patient was
observed in January 2014 using urinary ultrasonography during a
medical examination at the West China Hospital of Sichuan
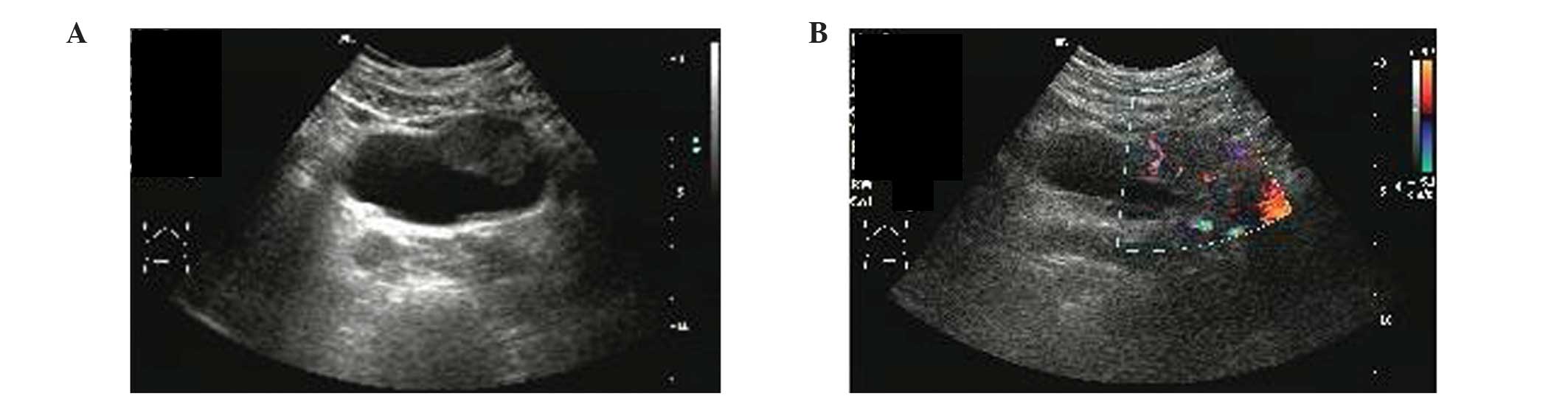
University (Chengdu, China). The ultrasound study (EPIQ 5, Philips
Diagnostic Ultrasound System and Transducers, Bothell, WA, USA)
revealed a mass (3.7×2.5×3.7 cm) on the left anterior wall of the
bladder; in addition, color Doppler sonography indicated that the
mass had predominantly arterial vascularization (Fig. 1). The patient was then admitted. The
patient had a 10-year history of hypertensive disease (the highest
blood pressure recorded was 168/100 mmHg); however, the patient's
blood pressure had been controlled to 120/80 mmHg through treatment
with diovan (80 mg, once-a-day) and norvasc (5 mg, once-a-day). The
patient had no history of hematuria, headaches, palpitations or
dizziness associated with micturition or postural changes. Routine
blood and urine tests demonstrated no abnormalities.
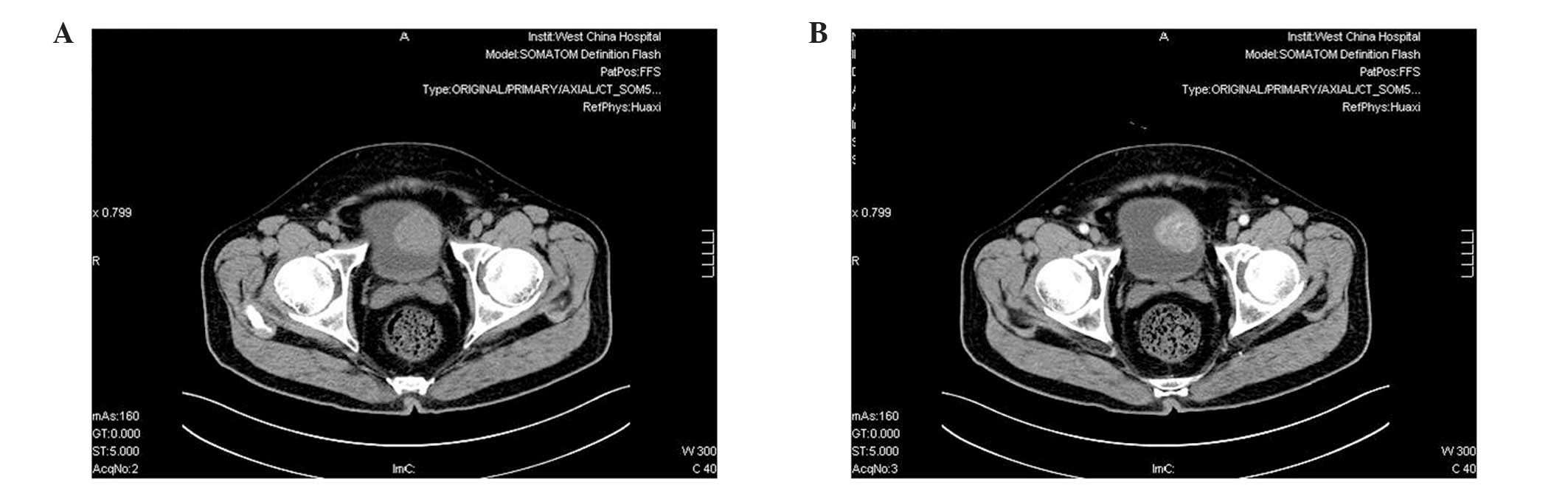
A computed tomography (CT) scan (SOMATOM Sensation64
MSCT, Siemens AG, Berlin, Germany) of the patient's abdomen and
pelvis revealed a 3.9×3.6 cm mass on the left anterior aspect of
the bladder, which protruded into the bladder cavity; the mass had
well-defined borders and there was no thickening of the bladder
wall surrounding the mass. On the plain CT images, it appeared that
the mass had a homogeneous iso-density (Fig. 2A); however, contrast-enhanced CT
images demonstrated that the degree of enhancement of the tumor was
markedly increased compared with that of the bladder wall (Fig. 2B). Metastatic disease of the other
abdominal organ systems was not observed on ultrasound examination
or CT scans. The solitary submucosal mass on the left anterior
aspect of the bladder with normal mucosal covering was confirmed by
cystoscopy (Olympus Cystoscope A4620, Olympus Corporation, Tokyo,
Japan).
On the basis of these examinations, the patient was
diagnosed with a bladder tumor and underwent a partial cystectomy.
The entire tumor was resected and during the intervention, no
hypertensive crisis occurred.
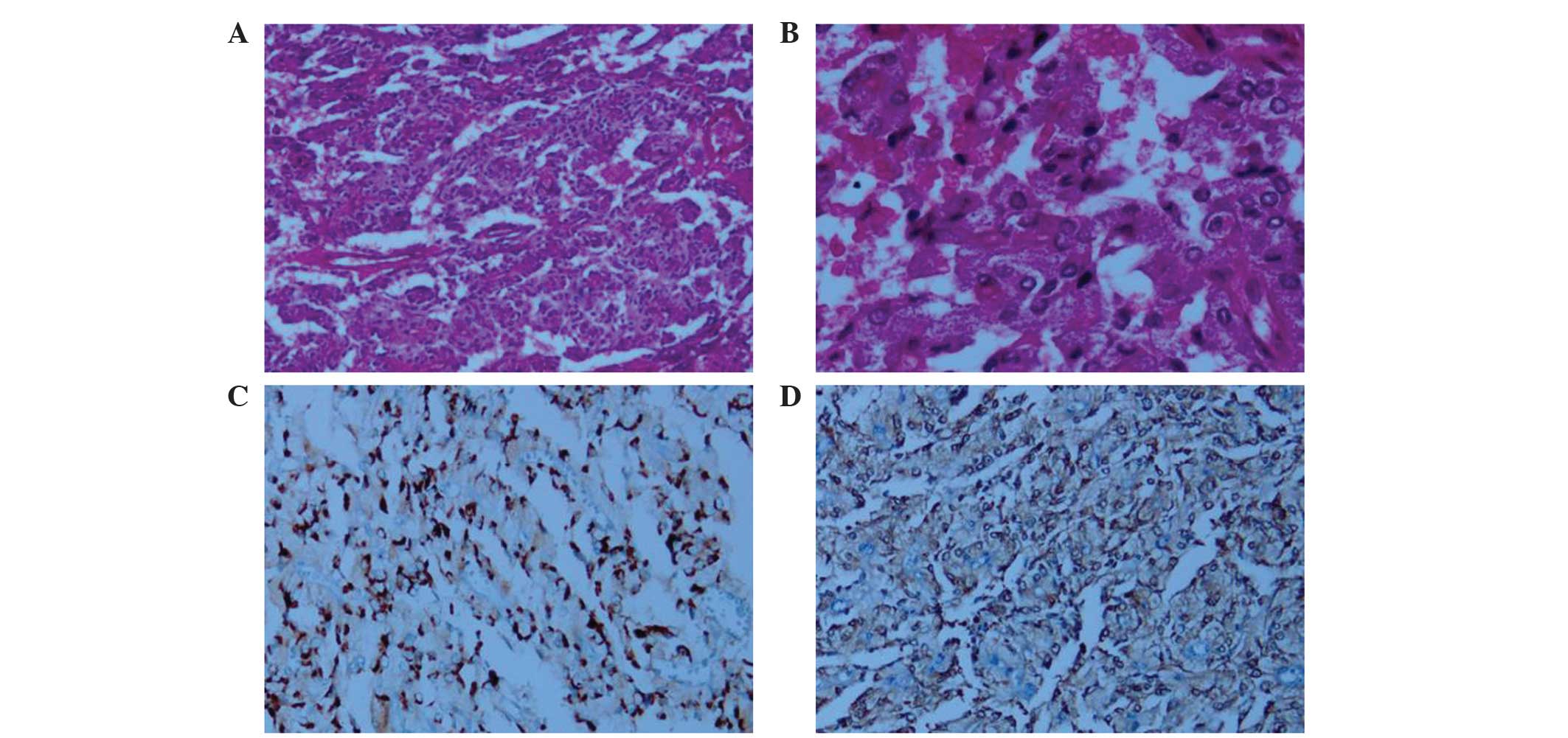
Pathological analysis demonstrated that the mass on
the left anterior aspect of the bladder was a paraganglioma. It was
confirmed using positive immunohistochemical stains for
neuron-specific enolase (mouse anti-human monoclonal NSE; cat. no.
M0873; Dako, Glostrup, Denmark; dilution, 1:100; incubation, 1 h at
37°C) and chromagranin (mouse anti-human monoclonal chromagranin;
cat. no. ZM-0076; ZSGB-BIO, Beijing, China; dilution, 1:150;
incubation, 1 h at 37°C) as well as negative immunoreactions for
muscle-specific actin (MSA) (mouse anti-human monoclonal MSA; cat.
no. 0032; Fuzhou Maixin Biotechnology Development Co., Ltd.,
Fuzhou, China; 1:60, incubation, 1 h at 37°C), desmin (mouse
anti-human monoclonal desmin; cat. no. M0760; Dako; dilution,
1:100; incubation, 1 h at 37°C), pan cytokeratin (mouse anti-human
monoclonal PCK; cat. no. ZA-0573; ZSGB-BIO; dilution, 1:100;
incubation, 1 h at 37°C) and epithelial membrane antigen (mouse
anti-human monoclonal EMA; cat. no. M0613; Dako; dilution, 1:100;
incubation, 1 h at 37°C) were negative. The Ki-67 labeling index
was ~5% (Fig. 3).
The patient demonstrated good postoperative recovery
and at 3 months follow-up the patient felt well, with no signs of
recurrence. The patient's blood pressure was not affected by the
operation; however, continuation of diovan and norvasc treatment is
required to control the hypertension to within a normal range.
Discussion
Paragangliomas account for ~10% of pheochromocytoma
and 800 cases are diagnosed annually in the USA (2). Paragangliomas are observed in patients
of all ages; however, they have been found to occur more frequently
during the 2nd decade of life and the ratio of female to male
patients is 3:2 (11–13). The most common site for paragangliomas
is the organ of Zuckerkandl at the distal aorta or aortic
bifurcation and less commonly, they are observed in the head, neck,
thorax and bladder (14). The first
case of a paraganglioma of the bladder was described by Zimmerman
et al (15) in 1953.
Pheochromocytomas and paragangliomas may secrete catecholamines and
these substances are responsible for symptoms, including headache,
palpitations and fainting. Hypertensive crises may be triggered by
inducing the release of catecholamine during urination if the
bladder paraganglioma is functional. Therefore endocrine tests,
including those for metanephrines, vanillylmandelic acid,
epinephrine, norepinephrine and dopamine in a 24-h urine and serum
sample, must be performed when a case of urinary bladder
paraganglioma is suspected. However, 10–15% of such tumors are
non-functioning and a further 10% have hormonal activities that do
not manifest clinically (11). This
type of tumor does not have produce typical test results from blood
or urine samples collected at the occurrence of typical symptoms.
If the surgeons are unprepared for the resection of paragangliomas
during pheochromocytoma surgery, it may result in intraoperative
hypertensive crises and increase the risk of mortality. Therefore,
when a paraganglioma of the bladder is suspected and the basal
catecholamine levels appear normal, it may be beneficial for
diagnosis to measure the plasma catecholamine concentrations prior
to, during and following micturition (16).
Imaging examinations are essential for preoperative
localization and qualitative analysis. The sensitivities of the
localizing examination for ultrasound, CT scan, magnetic resonance
imaging and 131I-metaiodobenzylguanidine are 89, 64–100,
88–100 and 62–88%, respectively (11,17,18).
Positron emission tomography (PET) has an increased accuracy
compared with MIBG scans for the localization of paragangliomas due
to the higher spatial resolution of PET scanning (19).
Bladder paragangliomas are frequently treated
surgically. The surgical options include radical cystectomy,
partial cystectomy and transurethral resection. It was estimated
that ~3% of patients treated by the above therapies succumbed to
their cancer. However, it is important to note that ≥20% of
patients had recurrence or metastases at the last known follow-up
(20,21). The present case report may be helpful
to standardize the reporting guidelines of paraganglioma cases in
order to better understand its natural progression and
outcomes.
The current study presented the case of a
61-year-old male with urinary bladder paraganglioma. Notably, the
patient did not exhibit any of the typical symptoms associated with
bladder paraganglioma, such as headache, palpitations and postural
changes, and thus initially a diagnosis of paraganglioma was not
considered. For patients who are suspected to have paraganglioma,
it is necessary to stabilize hypertension prior to surgical
treatment with α-blocking agents. In the present case, partial
cystectomy was performed without the pre-operative adminstration of
α-blocking agents and fortunately, no hypertensive crisis or
bleeding occurred during surgery.
It is extremely difficult to pre-operatively
diagnose asymptomatic bladder paraganglioma. Based on the present
case and previous studies, if CT or cystoscopy reveals a mass with
well-defined borders that is located in the submucosa with an
intact surface, a diagnosis of bladder paraganglioma must be
considered and subsequent preoperative preparations must be
performed to reduce the risk of intraoperative hypertensive
crisis.
References
|
1
|
Tischler AS: Pheochromocytoma and
extra-adrenal paraganglioma: Updates. Arch Pathol Lab Med.
132:1272–1284. 2008.PubMed/NCBI
|
|
2
|
Elder EE, Elder G and Larsson C:
Pheochromocytoma and functional paraganglioma syndrome: No longer
the 10% tumor. J Surg Oncol. 89:193–201. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dahm P and Gschwend JE: Malignant
non-urothelial neoplasms of the urinary bladder: A review. Eur
Urol. 44:672–681. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hanji AM, Rohan VS, Patel JJ and Tankshali
RA: Pheochromocytoma of the urinary bladder: A rare cause of severe
hypertension. Saudi J Kidney Dis Transpl. 23:813–816. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pastor-Guzmán JM, López-García S,
Giménez-Bachs JM, et al: Paraganglioma of the bladder: Controversy
regarding treatment. Urol Int. 73:270–275. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sheps SG, Jiang NS, Klee GG and van
Heerden JA: Recent developments in the diagnosis and treatment of
pheochromocytoma. Mayo Clin Proc. 65:88–95. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Messerli FH, Finn M and MacPhee AA:
Pheochromocytoma of the urinary bladder. Systemic hemodynamics and
circulating catecholamine levels. JAMA. 247:1863–1864. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Feng N, Li X, Gao HD, Liu ZL, Shi LJ and
Liu WZ: Urinary bladder malignant paraganglioma with vertebral
metastasis: A case report with literature review. Chin J Cancer.
32:624–628. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Beilan J, Lawton A, Hajdenberg J and
Rosser CJ: Locally advanced paraganglioma of the urinary bladder: A
case report. BMC Res Notes. 6:1562013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li S, Lui S, Li F, Yue Q, Huang X and Gong
Q: Unsuspected paraganglioma of the urinary bladder with
intraoperative hypertensive crises: A case report. Exp Ther Med.
6:1067–1069. 2013.PubMed/NCBI
|
|
11
|
Lucon AM, Pereira MA, Mendonça BB, Halpern
A, Wajchenbeg BL and Arap S: Pheochromocytoma: Study of 50 cases. J
Urol. 157:1208–1212. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bolli V, Cerioni M, Martino A, et al:
Unusual benign mass of the bladder in children: Report of 2 cases.
Radiol Med. 92:154–156. 1996.(In Italian). PubMed/NCBI
|
|
13
|
Kouame BD, Lardy H, Michalak S, Lacombe A,
Mercier C and Robert M: Bladder paraganglioma (pheochromocytoma): A
rare tumor in children. Apropos of a case. Ann Urol (Paris).
32:363–366. 1998.(In French). PubMed/NCBI
|
|
14
|
Lee KY, Oh YW, Noh HJ, et al: Extraadrenal
paragangliomas of the body: Imaging features. AJR Am J Roentgenol.
187:492–504. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zimmerman IJ, Biron RE and MacMahon HE:
Pheochromocytoma of the urinary bladder. N Engl J Med. 249:25–26.
1953. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lecube A, Peña A, Hernández C and Simó R:
Bladder pheochromocytoma: A variation in the plasma catecholamines
during micturition. Med Clin (Barc). 112:477–478. 1999.(In
Spanish). PubMed/NCBI
|
|
17
|
Bravo EL: Evolving concepts in the
pathophysiology, diagnosis and treatment of pheochromocytoma.
Endocr Rev. 15:356–368. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jalil ND, Pattou FN, Combemale F, et al:
Effectiveness and limits of preoperative imaging studies for the
localisation of pheochromocytomas and paragangliomas: A review of
282 cases. French Association of Surgery (AFC), and The French
Association of Endocrine Surgeons (AFCE). Eur J Surg. 164:23–28.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pacak K, Eisenhofer G and Goldstein DS:
Functional imaging of endocrine tumors: Role of positron emission
tomography. Endocr Rev. 25:568–580. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jansen R and Zaslau S: Paraganglioma of
the bladder. Clin Adv Hematol Oncol. 10:839–841. 2012.PubMed/NCBI
|
|
21
|
Tsai CC, Wu WJ, Chueh KS, et al:
Paraganglioma of the urinary bladder first presented by bladder
bloody tamponade: Two case reports and review of the literatures.
Kaohsiung J Med Sci. 27:108–113. 2011. View Article : Google Scholar : PubMed/NCBI
|