Introduction
Alveolar adenoma is an extremely rare pulmonary
neoplasm with specific characteristics, identified upon gross and
microscopic analysis (1,2). Grossly, alveolar adenoma presents a
rounded configuration that is well-circumscribed with a spongy
gray-white multilocular cut surface (1). Microscopically, this tumor comprises a
number of cystic spaces of variable sizes, which are lined by type
2 alveolar epithelial cells (1–3). These
tumors are often discovered incidentally on chest X-rays and
predominantly occur in the lung periphery (4). The radiological images typically reveal
a solitary, well-delineated, non-calcified nodule or mass with
homogeneous density. In certain cases, the nodules have a central
apparent cavity (5,6). These pulmonary lesions are considered to
be benign tumors and primarily occur in middle-aged woman who have
no history of smoking. The size of these lesions usually varies,
typically ranging between 0.2 and 10 cm (7,8).
In the present study, the case of a 47-year-old
female with an alveolar adenoma coexisting with intracranial
vascular malformations is reported and a literature review was
conducted, providing novel insights into the pathophysiology of
this disease.
Case report
A 47-year-old female with no history of smoking
underwent a routine medical examination prior to a
hysteromyomectomy at the First Affiliated Hospital of Zhejiang
University (Hangzhou, China) in November, 2010. A chest X-ray
revealed a dense pulmonary nodule on the right side of the chest.
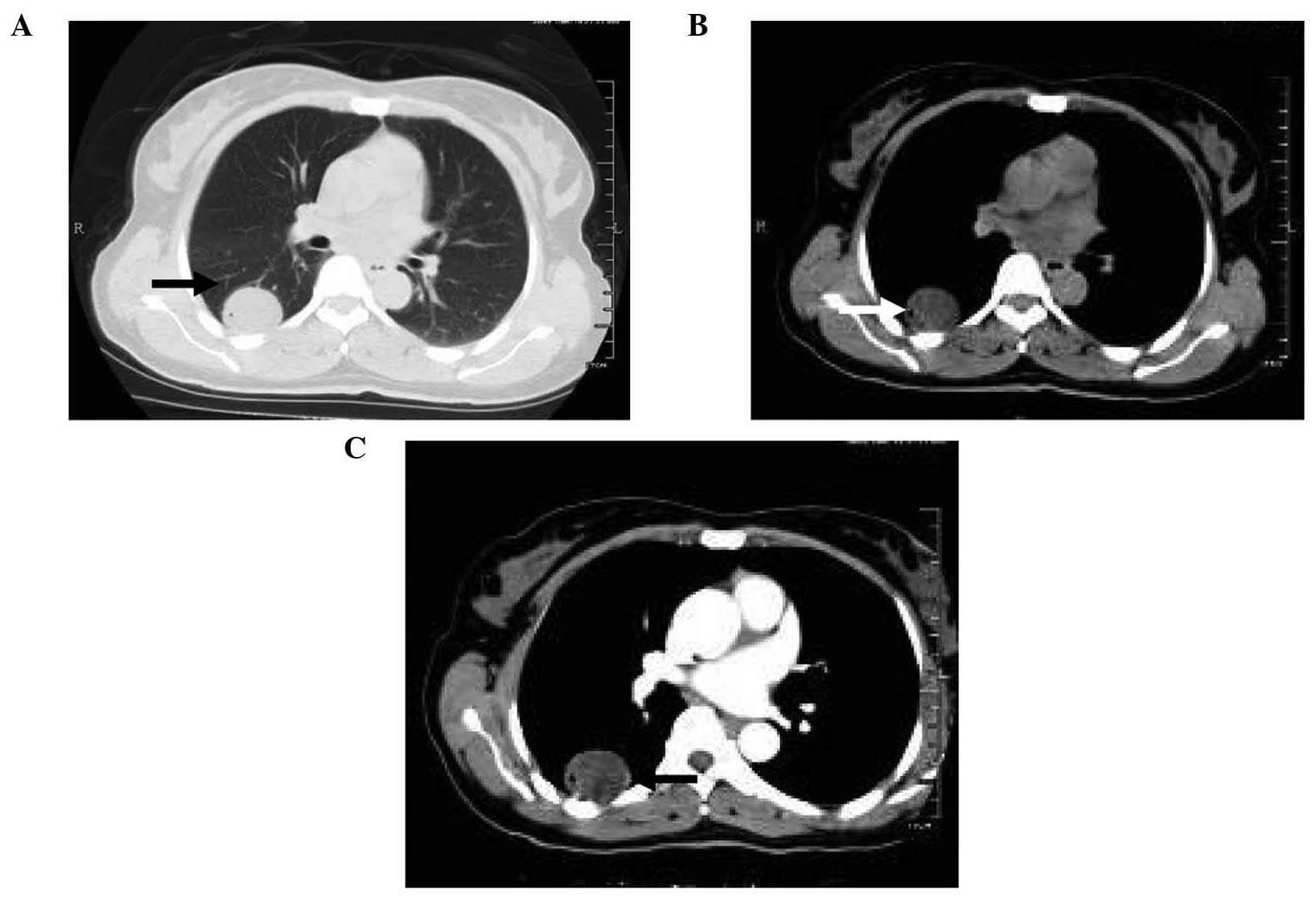
Further examination using a computed tomography (CT) scan detected
a 4-cm, low-density mass with air inclusions on the right lower
lobe of the lung (Fig. 1A and B). A
contrast-enhanced scan was produced with the attenuation of the
postcontrast CT scan set to 20 Hounsfield units greater than the
precontrast CT scan. The resulting image displayed a thin-rim of
enhancement in the cyst wall, without internal enhancement
(Fig. 1C). The initial diagnosis
established by a radiologist was a pulmonary abscess; however, the
patient did not present with any symptoms of infection, such as
night sweats, weight loss, coughing or dyspnea. No abnormalities
were detected in clinical and serological examinations, while
pulmonary function was also normal.
In December 2010, a thoracoscopic segmentectomy was
performed due to the possibility of low-grade malignancy of the
pulmonary lesion. Gross examination of the resected lung tissues
revealed a globular, pleural-based tumor, 4×4 cm in size, which was
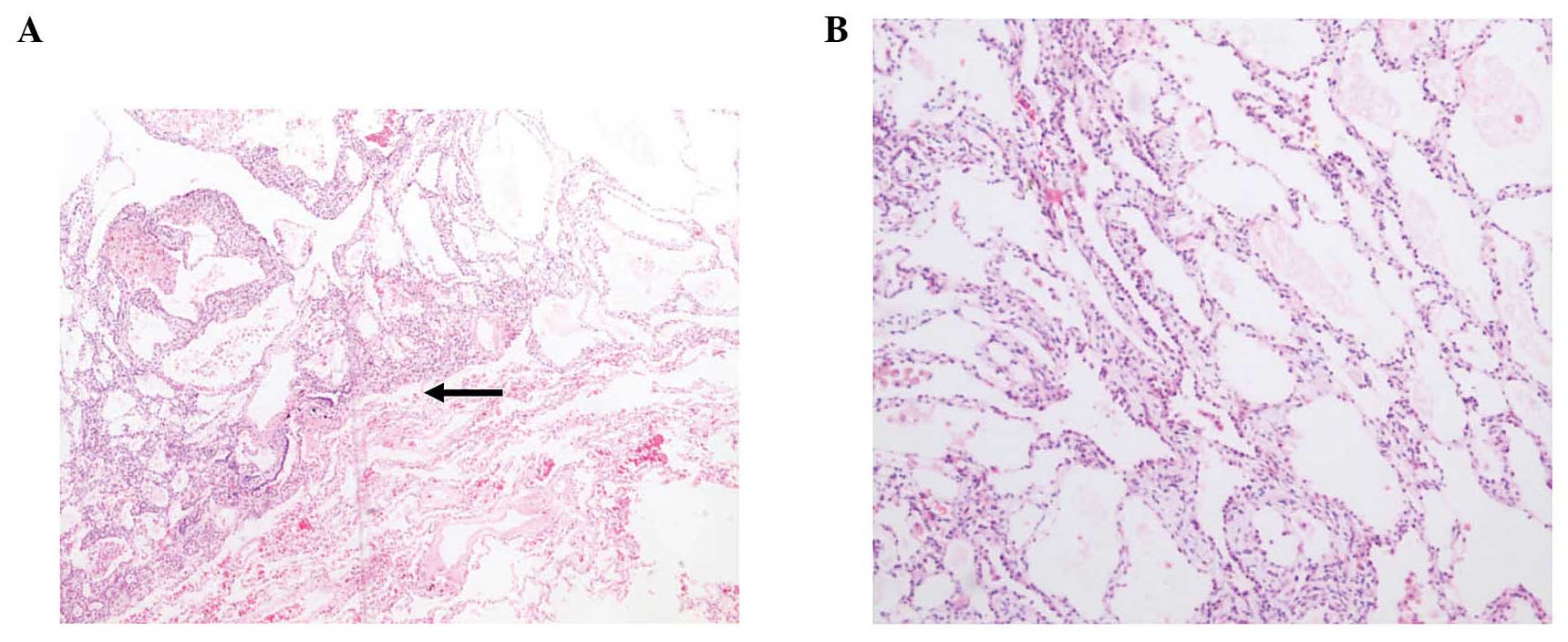
soft and pale grey. Microscopic analysis of the frozen resected
tissue indicated that the tumor was a well-demarcated,
non-invasive, multicystic mass (Fig.
2A) with spaces filled with eosinophilic granular material and
histiocytes (Fig. 2B). The cystic
spaces were lined by different types of epithelial cells, including
flat, cuboidal and ‘hobnail’ cells. The alveolar lumina contained a
small number of histiocytes with minimal cellular atypia, no
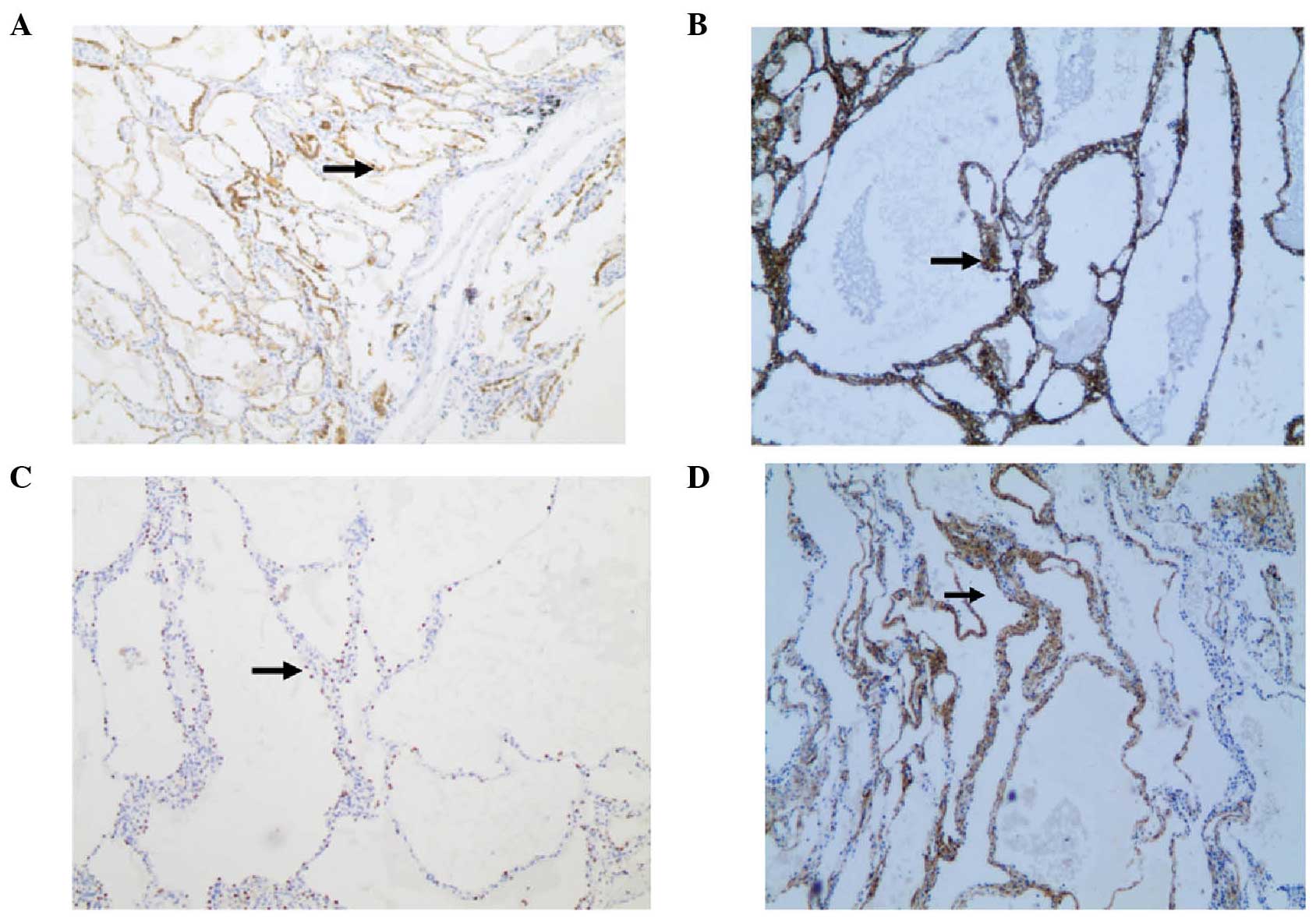
mitosis and no invasive growth. Immunohistochemical analysis
revealed the flat and cuboidal epithelia were positive for
pan-cytokeratin (CK), CK7, CD10 and thyroid transcription factor 1
(TTF1; Fig. 3A–C), but negative for
vimentin, calretinin and CD31. In addition, the mesenchyme was
reactive for smooth muscle antigen (Fig.
3D). The stroma contained spindle cells mixed with inflammatory
cells, histiocytes, lymphocytes, erythrocytes and plasma cells. No
Clara cells, mucous cells and APUD cells were identified. These
findings indicated that the tumor was an alveolar adenoma.
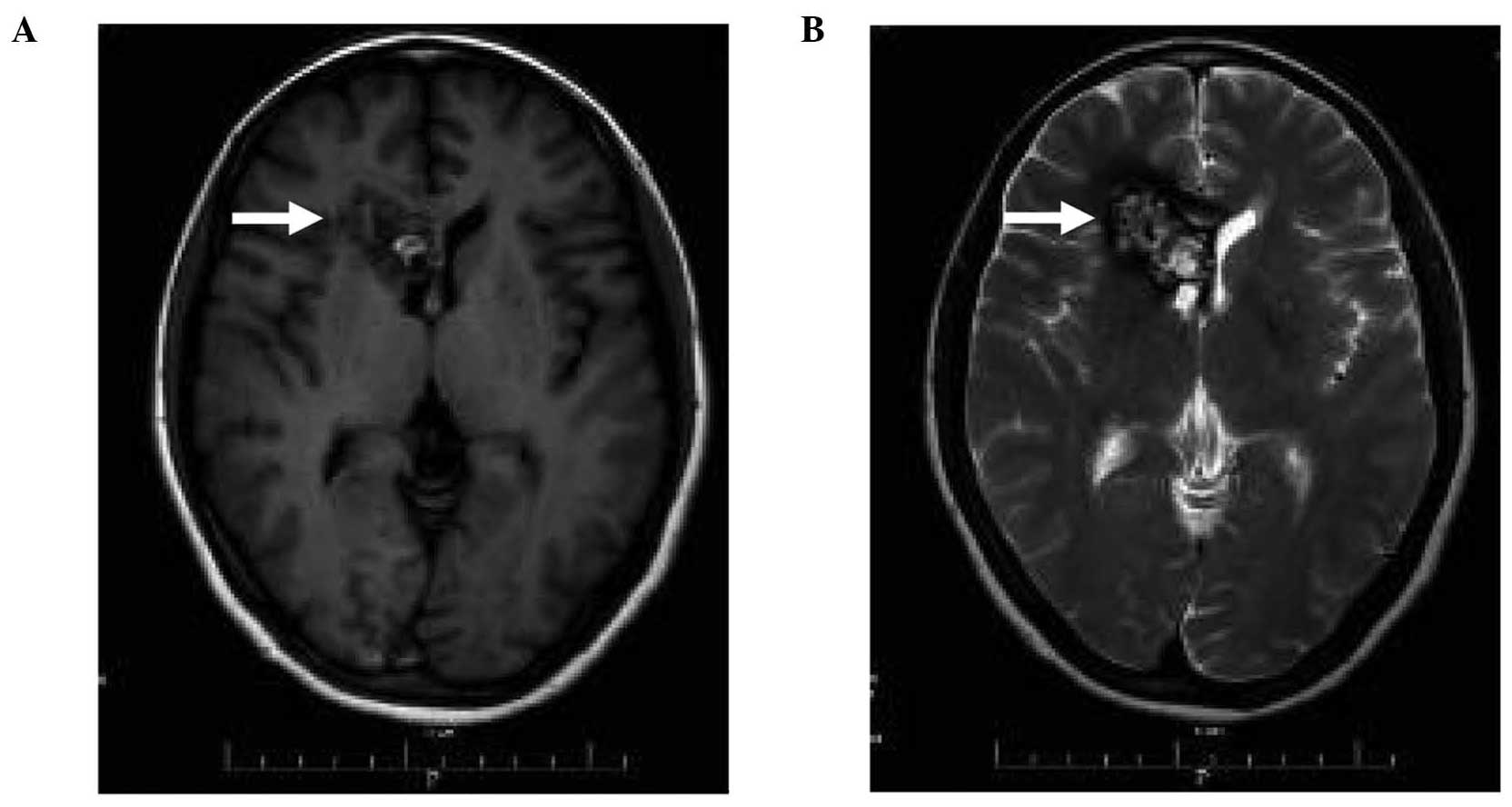
A routine CT scan of the head demonstrated the
presence of a lesion next to the right lateral ventricle. However,
the patient displayed no adverse symptoms, including headache,
nausea, blurred vision or impairment of limb movement. In addition,
the patient had no previous history of seizures or hypertension. A
magnetic resonance imaging scan of the head revealed a 3.5×1.7-cm
lesion with mixed signals next to the anterior horn of the right
lateral ventricle. A T1-weighted image demonstrated a
heterogeneous, punctate pattern with a combination of high and low
signal intensity areas; however, no edema or mass effect was noted
(Fig. 4A). A T2-weighted image
displayed the presence of honeycomb-like structures (Fig. 4B). The intracranial lesion was
diagnosed as an arteriovenous malformation with hemorrhage.
Following consultation with a neurologist in the
Department of Neurological Surgery (First Affiliated Hospital,
Zhejiang University), a digital subtraction angiography (DSA) was
performed. No apparent cerebrovascular malformation was observed on
the DSA. Considering the benign nature of the intracranial lesion,
as detected by DSA, and the potential risks associated with surgery
and radiotherapy, the patient selected to undergo follow-up with
observation only. No exacerbation of the intracranial lesion was
noted during the 4-year follow-up period. Similarly, the
postoperative course of the alveolar adenoma was uneventful, and
there was no sign of recurrence 52 months after surgery. The study
was approved by the ethics committee of the First Affiliated
Hospital of Zhejiang University, and written informed consent was
obtained from the patient prior to publication of the study.
Discussion
Alveolar adenoma of the lung is an extremely rare
primary benign epithelial lesion involving the lung parenchyma,
which can have an alveolar or papillary cellular architecture
(1,3,4).
Determining of the exact number of alveolar adenoma cases is
difficult, since these tumors are often confused with other rare
benign lung tumors. The first alveolar adenoma case was reported by
Yousem and Hochholzer in 1986 (2). To
the best of our knowledge, the present study is the first report of
the coexistence of alveolar adenoma with intracranial arteriovenous
malformations.
Alveolar adenoma seldom causes symptoms. In a
limited number of cases, patients have presented with chest pain or
chronic cough (9–11). Only one previous study reported the
admission of an alveolar adenoma patient to the hospital with
severe dyspnea (12). Most alveolar
adenoma patients are 40–60 years old, with a slight female
predominance (1,2,8). The
youngest patient ever reported, to the best of our knowledge, was a
24-year-old male, who presented an 18×17-mm nodule on the lower
lobe of the left lung (13). Although
patients usually present with a single lesion, a previous study
described a case with three nodules on the two sides of the lung
(1).
Alveolar adenomas typically grow slowly; however, a
number of studies reported a sudden increase in size similar to
malignant tumor growth (5,8). Although alveolar adenomas have no
distinct imaging features, the contrast-enhanced CT scan performed
in the present study displayed enhancement around a thin-rim of the
nodule. Similar features have been identified in tuberculoma
patients (14), as well as a
previously-reported alveolar adenoma case (1).
From a diagnostic standpoint, a ‘lung mass’ is
defined as an abnormal spot in the lungs with a size of >3 cm.
The mass is considered to be a bronchogenic carcinoma until proven
otherwise (15). In the present case,
the pulmonary lesion identified on the CT scan was 4 cm in diameter
and, therefore, larger than the prognostic threshold of 3 cm. For
this reason, the lesion was removed by surgical lobectomy for
diagnostic and therapeutic purposes.
Structurally, alveolar adenoma is comprised of
epithelial and mesenchymal tissues, which can be identified by
histological analysis (3–5). Upon examination using light microscopy,
alveolar adenoma appears to be sharply demarcated from the
surrounding tissue, but with lack of encapsulation, similar to the
microcystic-like spaces that predominate the lesion. The cystic
spaces contain a clear cellular fluid, as well as histiocytes,
erythrocytes and foamy macrophages (4). In the current case, these cystic spaces
were lined with a single layer of epithelial cells, which were
mostly cuboidal or ‘hobnail’ in appearance.
Previous immunohistochemical studies have
demonstrated that alveolar adenoma epithelia are positive for
markers including pan-CK, epithelial membrane antigen and TTF-1
(16). Additionally, epithelia are
positive for type II pneumocyte markers, indicating that the
epithelial layer is derived from type II pneumocytes (16). In cases where the epithelial layer is
flattened in shape and resembles the endothelium, the absence of
immunostaining for CD31 or CD34 vascular markers may help to
distinguish alveolar adenoma from other pulmonary lesions (17,18).
The standard diagnosis of thoracic diseases is
challenged by varied pathological findings in patients. Using
clinical and histological findings, the current World Health
Organization Classification of Tumors (19) states that benign adenomas of the lung
include mucous gland, mucinous cyst, pleomorphic, alveolar and
papillary adenomas. Known histological markers must be used for the
differential diagnosis of benign alveolar tumors from malignant
tumors, including pulmonary adenoma, sclerosing hemangioma,
lymphangioma, atypical adenomatous hyperplasia and bronchoalveolar
carcinoma. For instance, positive immunostaining for CK in the
peripheral epithelial cells and negative immunostaining for
vascular markers can distinguish alveolar adenomas from
lymphangiomas (4).
However, diagnostic discrimination between alveolar
adenoma and bronchioloalveolar adenocarcinoma has been proven to be
difficult, since the two tumors exhibit positive immunoreactivity
for TTF-1, surfactant and epithelial markers (4,11).
Therefore, for an unambiguous diagnosis of alveolar adenoma, the
findings of immunohistochemical staining and gross structural
analysis are also required. The well-circumscribed growth pattern,
lack of lepidic growth and cellular atypia of alveolar adenoma
distinguishes it from the other carcinomas. Considering that
alveolar adenoma has a characteristic multicystic histology and
often resembles the normal lung parenchyma, pathological analysis
of the entire tumor resection is required for a clear-cut diagnosis
(5,10,20).
Intracranial arteriovenous malformations are
congenital vascular lesions usually identified in patients with an
age of 20–40 years (21). The typical
clinical presentation includes hemorrhage, seizures, progressive
neurological deficit or headaches (21). In the present study, the patient
experienced no neurological symptoms and no apparent
cerebrovascular malformations were detected by DSA. A neurologist
diagnosed the intracranial lesion as an occult arteriovenous
malformation based on previously-reported features (22). Although surgery is the recommended
treatment modality (23), the patient
selected to undergo long-term follow-up with clinical observation
only, considering the risks associated with surgery and
radiotherapy. During the 3-year follow-up period, no exacerbation
of the intracranial lesion was observed.
In conclusion, alveolar adenoma is an extremely rare
disease, which requires careful diagnosis and differentiation from
a solitary pulmonary lesion. Surgical resection remains the best
solution for the majority of patients. To the best of our
knowledge, no recurrence of alveolar adenoma has ever been reported
(1–6,8–11,20,24). The
present study is the first to report a case of incidental
identification of alveolar adenoma with intracranial vascular
malformations. The accurate diagnosis and appropriate treatment
provided the patient with an improved prognosis following surgical
lobectomy. Finally, the present study provides new insight into the
diagnosis of alveolar adenoma.
Acknowledgements
This study was supported by a grant from the
Zhejiang Provincial Education Department, China (no.
Y200804939).
References
|
1
|
Fujimoto K, Muller NL, Sadohara J, Harada
H, Hayashi A and Hayabuchi N: Alveolar adenoma of the lung:
computed tomography and magnetic resonance imaging findings. J
Thorac Imaging. 17:163–166. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yousem SA and Hochholzer L: Alveolar
adenoma. Hum Pathol. 17:1066–1071. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sak SD, Koseoglu RD, Demirag F, Akbulut H
and Gungor A: Alveolar adenoma of the lung. Immunohistochemical and
flow cytometric characteristics of two new cases and a review of
the literature. Apmis. 115:1443–1449. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Burke LM, Rush WI, Khoor A, et al:
Alveolar adenoma: a histochemical, immunohistochemical and
ultrastructural analysis of 17 cases. Hum Pathol. 30:158–167. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kondo N, Torii I, Hashimoto M, et al:
Alveolar adenoma of the lung: a case report. Ann Thorac Cardiovasc
Surg. 17:71–73. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Saito EH, de Aaraujo LR, Carneiro LH, de
Oliveira Neto AA, Correa JC and Teixeira LS: Alveolar adenoma. J
Bras Pneumol. 32:267–269. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bhavsar T, Uppal G, Travaline JM, Gaughan
C, Huang Y and Khurana JS: An unusual case of a microscopic
alveolar adenoma coexisting with lung carcinoma: a case report and
review of the literature. J Med Case Rep. 5:1872011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wang X, Li WQ, Yan HZ, et al: Alveolar
adenoma combined with multifocal cysts: case report and literature
review. J Int Med Res. 41:895–906. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cakan A, Samancilar O, Nart D and Cagirici
U: Alveolar adenoma: an unusual lung tumor. Interact Cardiovasc
Thorac Surg. 2:345–347. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nosotti M, Mendogni P, Rosso L, et al:
Alveolar adenoma of the lung: unusual diagnosis of a lesion
positive on PET scan. A case report. J Cardiothorac Surg. 7:12012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hartman MS, Epstein DM, Geyer SJ and
Keenan RJ: Alveolar adenoma. Ann Thorac Surg. 78:1842–1843. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Petrella F, Rizzo S, Pelosi G, Borri A,
Galetta D, et al: Giant alveolar adenoma causing severe dyspnoea. J
Thorac Oncol. 5:1088–1090. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
De Rosa N, Maiorino A, De Rosa I, Curcio
C, Sellitto C and Amore D: CD34 expression in the stromal cells of
alveolar adenoma. Case Rep Med. 2012:9135172012.PubMed/NCBI
|
|
14
|
Sakai F, Sone S, Maruyama A, et al:
Thin-rim enhancement in Gd-DTPA-enhanced magnetic resonance images
of tuberculoma: a new finding of potential differential diagnostic
importance. J Thorac Imaging. 7:64–69. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gould MK, Fletcher J, Iannettoni MD, et
al: Evaluation of patients with pulmonary nodules: when is it lung
cancer?: ACCP evidence-based clinical practice guidelines (2nd
edition). Chest. 132 (Suppl):108–130. 2007. View Article : Google Scholar
|
|
16
|
Halldorsson A, Dissanaike S and Kaye KS:
Alveolar adenoma of the lung: a clinicopathological description of
a case of this very unusual tumour. J Clin Pathol. 58:1211–1214.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cagle PT, Allen TC and Fraire AE: Alveolar
adenoma. Atlas of Neoplastic Pulmonary Disease. 19–21. 2010.
|
|
18
|
Limmer S, Krokowski M and Kujath P:
Pulmonary lymphangioma. Ann Thorac Surg. 85:336–339. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Travis WD, Brambilla E, Müller-Hermlink HK
and Harris CC: Pathology and genetics. Tumours of the lung, pleura,
thymus and heartWorld Health Organization Classification of
Tumours. IARC Press; Lyon: 2004
|
|
20
|
Hamid Kazerouni A and Chetty R: Alveolar
adenoma of the lung. Diagnostic Histopathology. 19:311–313. 2013.
View Article : Google Scholar
|
|
21
|
Fleetwood IG and Steinberg GK:
Arteriovenous malformations. Lancet. 359:863–873. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lobato RD, Perez C, Rivas JJ and Cordobes
F: Clinical, radiological and pathological spectrum of
angiographically occult intracranial vascular malformations.
Analysis of 21 cases and review of the literature. J Neurosurg.
68:518–531. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mossa-Basha M, Chen J and Gandhi D:
Imaging of cerebral arteriovenous malformations and dural
arteriovenous fistulas. Neurosurg Clin N Am. 23:27–42. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nakamura H, Adachi Y, Arai T, et al: A
small alveolar adenoma resected by thoracoscopic surgery. Ann
Thorac Surg. 87:956–957. 2009. View Article : Google Scholar : PubMed/NCBI
|