Introduction
Follicular dendritic cells (FDCs), localized to
primary and secondary B cell follicles, are unique immune cells
participating in the regulation of humoral immune responses. The
cells facilitate the activation of B cells, as they trap and retain
antigens in the form of highly immunogenic immune complexes
(1). A tumor arising from these FDCs
is termed a FDC sarcoma (FDCS), and since Monda et al
(2) first described FDCS in 1986,
~200 cases have been reported in the English literature. In the
majority of cases, FDCS presents as a painless, slow-growing
well-circumscribed mass, with no constitutional symptoms, such as
fever, night sweats, and weight loss (3). The diagnosis of FDCS depends on an array
of morphological, histological, electron microscopic and, most
importantly, immunohistochemical studies. Surgical resection
remains the cornerstone of treatment. The efficacy of adjuvant
therapy (chemotherapy or radiation) is yet unclear (4,5). Cervical
and intraabdominal lymph nodes are the most frequently affected
nodal sites. In addition, various extranodal sites can also be
involved, particularly in the liver, lungs and tonsils (6). The current study presents the second
published case of FDCS with extensive lymph node involvement, as to
the best of our knowledge, only one case has been reported
previously (7). Written informed
consent was obtained from the patient's family for the publication
of this case report.
Case report
Patient presentation
A 65-year-old male presented to the Xiangya Second
Hospital (Central South University, Changsha, Hunan, China) in July
2013 with a recurrent fever, abdominal distension and mild edema of
the lower limbs that had persisted for 2 weeks. There was no
significant past medical history. The physical examination revealed
rebound tenderness in the abdomen, a palpable enlarged liver and
shifting dullness. The laboratory test results of note were as
follows: A white blood cell count of 6,200/µl (normal,
4000–10000/µl), a blood neutrophil percentage of 78.30 (normal,
50–70%), an erythrocyte sedimentation rate of 40 mm/h (normal,
<20 mm/h), a C-reactive protein level of 96.80 mg/l (normal,
<10 mg/l) and a procalcitonin level of 0.25 ng/ml (normal,
<0.5 ng/ml). Mycotic spores were found in a stool sample.
Routine biochemical analysis revealed a marked increase in
γ-glutamyl transpeptidase and alkaline phosphatase levels 134.2 U/l
(normal, 9.0–39.0 U/l) and 217.4 U/l (normal, 42.0–141.0 U/l)
respectively. The patient underwent an ultrasound of the abdomen,
which revealed multiple gallbladder stones, cholecystitis,
enlargement of the liver and spleen, multiple cysts on the kidneys
and small amounts of ascites. The first clinical impression that
was formed to account for the ascites and recurrent fever was one
of infection, and empirical clinical treatment using the antibiotic
moxifloxacin (400 mg/day for 7 days) combined with diuretic
treatment [frusemide (20 mg/day) and aldactone, (60 mg/day) for 10
days] was initiated prior to the outcome of a bacterial culture.
Meanwhile, the patient received a computed tomography (CT) scan to
further identify possible reasons for the recurrent fever, as well
as the enlargement of the liver and spleen. The CT scan detected
extensive enlargement of the lymph nodes in the mediastinal,
retroperitoneal and mesenteric areas (Fig. 1). Color Doppler ultrasonography of the
neck revealed multiple enlarged cervical lymph nodes, while a bone
marrow specimen showed no malignancy. An excisional biopsy of a
cervical lymph node was immediately performed, which revealed the
existence of a poorly-differentiated malignant tumor.
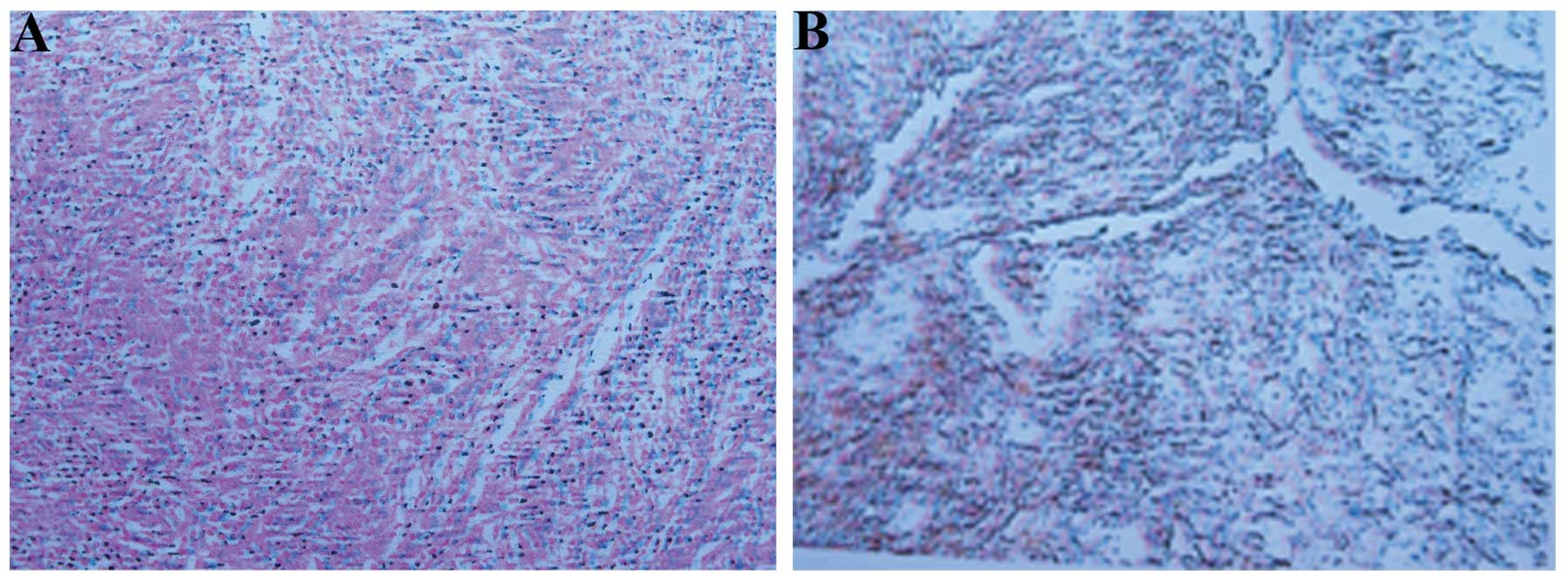
Histological findings
Macroscopically, the cervical lymph node was
1×0.3×0.8 cm in size. On immunohistochemical (IHC) staining, the
diagnostic antibodies used included antibodies against cluster of
differentiation (CD) 23(++) (Fig. 2),
CD21(++), S-100(–), D1a(–), CD3(+), CD31(–), CD45RO(+), CK(–),
CD79a (+) and CD20(+). The intensity of the dye color was graded as
0 (no color), 1 (light yellow), 2 (light brown) or 3 (brown), and
the number of positive cells was graded as 0 (<5%), 1 (5–25%), 2
(25–50%), 3 (51–75%) or 4 (>75%). The two grades were added
together and specimens were assigned one of four staining levels
based on this score: 0–1 (–), 2 (+), 3–4 (++) and >5 (+++).
Given that FDCS is specifically immunopositive to CD21, CD35,
and/or CD23, a diagnosis of FDCS was determined based on the
immunohistochemical staining result.
Treatment and outcome
Following one cycle of cyclophosphamide [0.1 g
intravenously, day 1], epirubicin (110 mg intravenous infusion, day
1), vincristine (2 mg intravenously, day 1) and prednisone (100 mg
orally, days 1–5) (CHOP) chemotherapy, the patient improved and
symptoms of recurrent fever and abdominal distension disappeared.
The patient will continue to receive consolidation chemotherapy (a
further cycle of CHOP) and undergo regular follow-up
examinations.
Discussion
FDCS is a rare low- to intermediate-grade malignant
tumor arising from germinal centers. The etiology and pathogenesis
of FDCS are unclear. Among the reported cases of patients with
FDCS, a small subset of cases are believed to be associated with
Epstein-Barr virus, with the majority of these cases involving the
liver or spleen and presenting with an inflammatory
pseudotumor-like morphology (8,9).
Additionally, patients with a background of hyaline-vascular
Castleman disease have been reported be at greater risk of FDCS,
although the exact association between the conditions remains
unknown (10,11).
As a whole, FDCS involves the lymph nodes in
one-half to two-thirds of cases, with the cervical nodes being the
most common site (6). In the present
case, the lymph nodes in the neck and the mediastinal,
retroperitoneal and mesenteric areas were extensively affected. In
past decades, a wide variety of extranodal sites have been
reported, including the tonsils, liver, spleen, oral cavity,
gastrointestinal tract, bones, soft tissues, skin and breasts
(6).
The diagnosis of FDCS remains challenging, and a
definitive diagnosis of this uncommon tumor depends on the
distinctive histological morphology and IHC profile. The
traditional diagnostic markers of FDCS mainly include CD21, CD23,
CD35 and clusterin. However, it should be noted that the markers of
FDC are not routinely used in IHC studies.
Among the published cases, surgery was used as the
mainstay of treatment for early FDCS (3). Adjuvant chemotherapy or radiotherapy
were reported to be used for the late disease management in several
cases, with therapies consisting of the CHOP regimen, the
ifosfamide, carboplatin and etoposide regimen, and the Adriamycin,
bleomycin, vincristine and dacarbazine regimen (12).
In the present case, the fundamental cause of the
enlargement of the liver and spleen remains in question. It is
uncertain whether the enlargement of the liver and spleen was
associated with the FDCS. Choi et al (7) described a case of
FDCS with extensive lymph nodes being affected. In that case, the
CT scan also revealed mild splenomegaly. However, there was no
mention of the turnover of the mild splenomegaly following two
cycles of CHOP, therefore a conclusion cannot be drawn from this
data. As a result, detailed follow-up records will be maintained in
the present case.
Follicular dendritic cell sarcoma is extremely rare.
From a diagnostic perspective, the pathologist should increase
awareness regarding these tumors and further develop means for
their molecular characterization. From a therapeutic perspective,
although surgery is the primary treatment, when feasible, a
multimodal approach and personalized treatment should be
considered. Due to the rarity of this tumor, its optimal treatment
yet to be defined, and multicenter cooperation and enrollment of
patients in well-designed clinical studies are necessary to
establish this.
References
|
1
|
Park CS and Choi YS: How do follicular
dendritic cells interact intimately with B cells in the germinal
centre. Immunology. 114:2–10. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Monda L, Warnke R and Rosai J: A primary
lymph node malignancy with features suggestive of dendritic
reticulum cell differentiation. A report of 4 cases. Am J Pathol.
122:562–572. 1986.PubMed/NCBI
|
|
3
|
Dalia S, Shao H, Sagatys E, et al:
Dendritic cell and histiocytic neoplasms: Biology, diagnosis, and
treatment. Cancer Control. 21:290–300. 2014.PubMed/NCBI
|
|
4
|
Karligkiotis A, Contis D, Bella M, et al:
Pediatric follicular dendritic cell sarcoma of the head and neck: A
case report and review of the literature. Int J Pediatr
Otorhinolaryngol. 77:1059–1064. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hu T, Wang X, Yu C, et al: Follicular
dendritic cell sarcoma of the pharyngeal region. Oncol Lett.
5:1467–1476. 2013.PubMed/NCBI
|
|
6
|
Saygin C, Uzunaslan D, Ozguroglu M,
Senocak M and Tuzuner N: Dendritic cell sarcoma: A pooled analysis
including 462 cases with presentation of our case series. Crit Rev
Oncol Hematol. 88:253–271. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Choi BS, Baek JH, Shin YM, et al:
Follicular dendritic cell sarcoma: A case report and review of the
literature. Cancer Res Treat. 42:121–124. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shek TW, Ho FC, Ng IO, Chan AC, Ma L and
Srivastava G: Follicular dendritic cell tumor of the liver.
Evidence for an Epstein-Barr virus-related clonal proliferation of
follicular dendritic cells. Am J Surg Pathol. 20:313–324. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Arber DA, Kamel OW, van de Rijn M, et al:
Frequent presence of the Epstein-Barr virus in inflammatory
pseudotumor. Hum Pathol. 26:1093–1098. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Meijs M, Mekkes J, van Noesel C, et al:
Paraneoplastic pemphigus associated with follicular dendritic cell
sarcoma without Castleman's disease; treatment with rituximab. Int
J Dermatol. 47:632–634. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yamamoto K, Yoshida M, Yamamoto M, et al:
An abdominal follicular dendritic cell tumor in Castleman's
disease. Rinsho Ketsueki. 45:1033–1038, (In Japanese). PubMed/NCBI
|
|
12
|
Kairouz S, Hashash J, Kabbara W, et al:
Dendritic cell neoplasms: An overview. Am J Hematol. 82:924–928.
2007. View Article : Google Scholar : PubMed/NCBI
|