Introduction
Epithelial ovarian cancer results in mortality more
frequently than any other gynecologic malignancy, as the majority
of patients present with advanced stage disease (1). Up-front primary cytoreductive surgery
followed by chemotherapy is able to improve overall survival, and
remains the standard treatment for the majority of patients with
resectable advanced ovarian cancer (2). Compared with other cancers, ovarian
cancer, and particularly clear cell carcinoma, is associated with a
high incidence of deep venous thrombosis (DVT), which may affect
surgical outcomes. The overall incidence of symptomatic DVT in
ovarian cancer is 9.7–16.6% (3,4). However,
the detection of DVT prior to the diagnosis of ovarian cancer is
rare, with an estimated incidence of 3.2% (3). Up-front primary cytoreductive surgery
remains a significant clinical challenge for patients with DVT.
Inferior vena cava (IVC) filters are typically
placed in the perioperative period of primary cytoreductive surgery
to reduce the risk of DVT-associated pulmonary embolism (PE)
(5–7).
Although IVC filters effectively prevent PE, they are do not
improve survival rates in patients with ovarian cancer undergoing
primary cytoreductive surgery, due to their significant associated
complications (8,9) and the high risk of hematogenous distant
metastasis in this population (10).
Therefore, the use of IVC filters in combination with up-front
primary cytoreductive surgery for ovarian cancer in patients with
DVT is controversial.
The current study presents the rare case of a
patient with DVT in the two lower extremities, identified prior to
the diagnosis of clear cell ovarian cancer. The patient underwent
optimal primary cytoreductive surgery within 1 month of
unsuccessful anticoagulant therapy, without placement of a
preoperative IVC filter. The patient's surgical outcome was good,
with resolution of lower limb swelling and without PE. The patient
was followed-up for >3 years, during which time serum tumor
marker assays and transvaginal sonography (TVS) identified no
evidence of tumor recurrence. The present case provides significant
information regarding the potential management of ovarian cancer in
patients with DVT. Other published case reports of ovarian cancer
associated with DVT in the literature were also evaluated.
Case report
Written consent from the patient for the use of
clinical materials for research purposes and approval from the
Institutional Ethics Board of the First Affiliated Hospital of Sun
Yat-Sen University (Guangzhou, China) were obtained.
A 49-year-old female [body mass index (BMI), 24.0
kg/m2] presented to the Vascular Surgery Department at
the First Affiliated Hospital, Sun Yat-Sen University with reddish
swelling and pain in the right leg, which had persisted for 3 days.
The difference in circumference between the patient's lower limbs
was 2.3 cm (left, 34.5 cm; right, 36.8 cm). Color Doppler flow
imaging of the right lower extremity identified multiple DVTs in
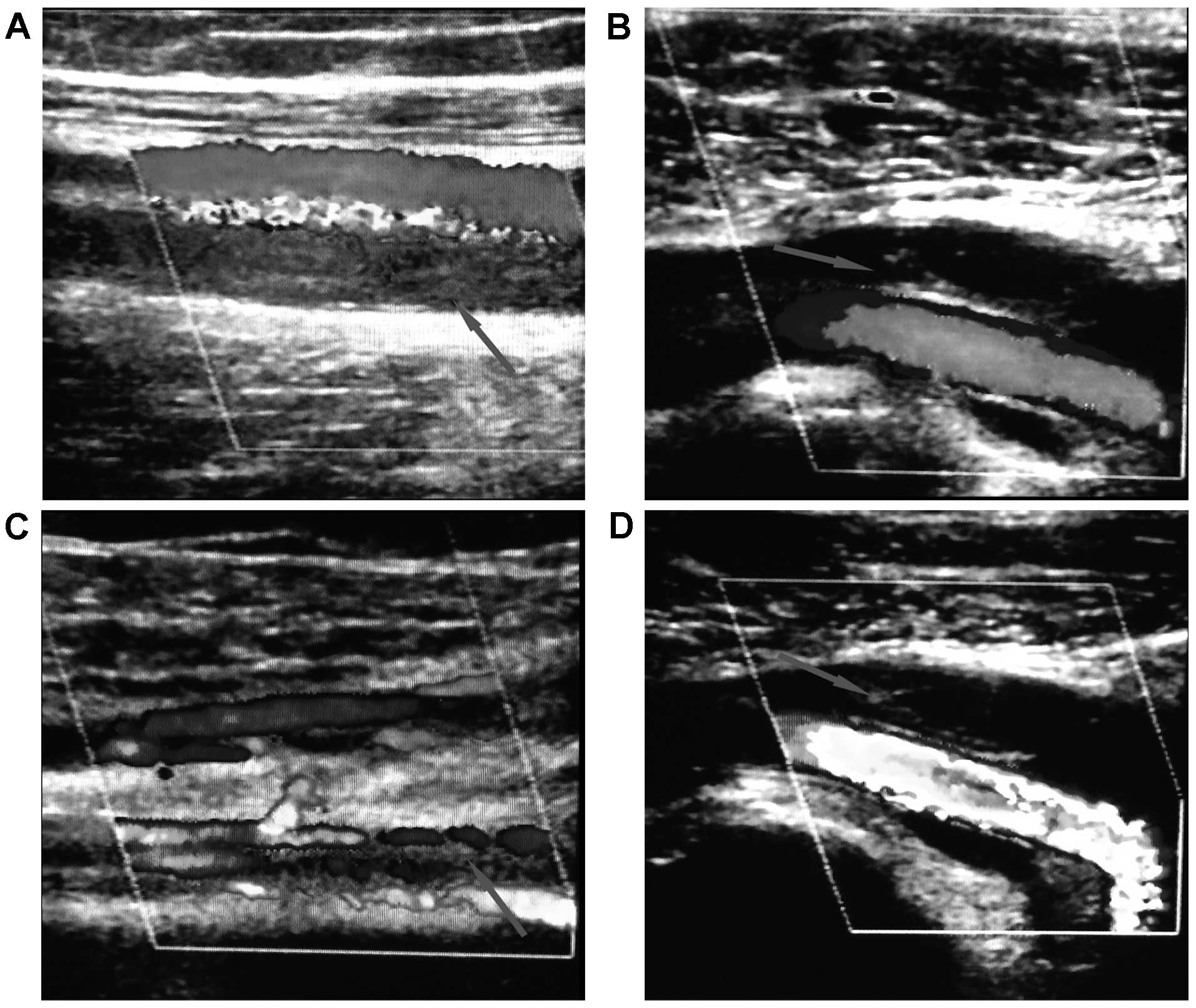
the superficial femoral, popliteal and fibular veins (Fig. 1A-C). Coagulation function tests were
performed, including platelet count (219×109/l), D-dimer
[18,190.00 µg/l, increased compared with normal values
(increased)], prothrombin time (17.8 sec, increased), activated
partial thromboplastin time (30.6 sec), thrombin time (17.2 sec),
fibrinogen (2.00 g/l) and international normalized ratio (1.6,
increased). The patient had no history of trauma, surgery, hormone
therapy or smoking, and was also single and without a sexual
history. The patient's family history was negative for clotting
disorders. The patient underwent low molecular weight heparin
anticoagulation therapy. However, the patient's symptoms did not
improve following 2 weeks of continuous therapy, and the popliteal
vein in the lower left extremity developed a thrombus with 80%
stenosis (Fig. 1D). Occult malignancy
was suspected and therefore, the expression of 10 serum tumor
markers was measured: Human epididymis protein (168.7 pmol/l,
increased), cancer antigen (CA) 153 (3,000 U/ml, increased), CA72-4
(15.09 U/ml, increased), CA125 (541.5 U/ml, increased), CA199
(111.4 U/ml, increased), carcinoembryonic antigen (0.619 ng/ml),
neuron-specific enolase (24.78 ng/ml, increased), human chorionic
gonadotropin-β (0.100 mIU/ml), squamous cell carcinoma antigen (0.7
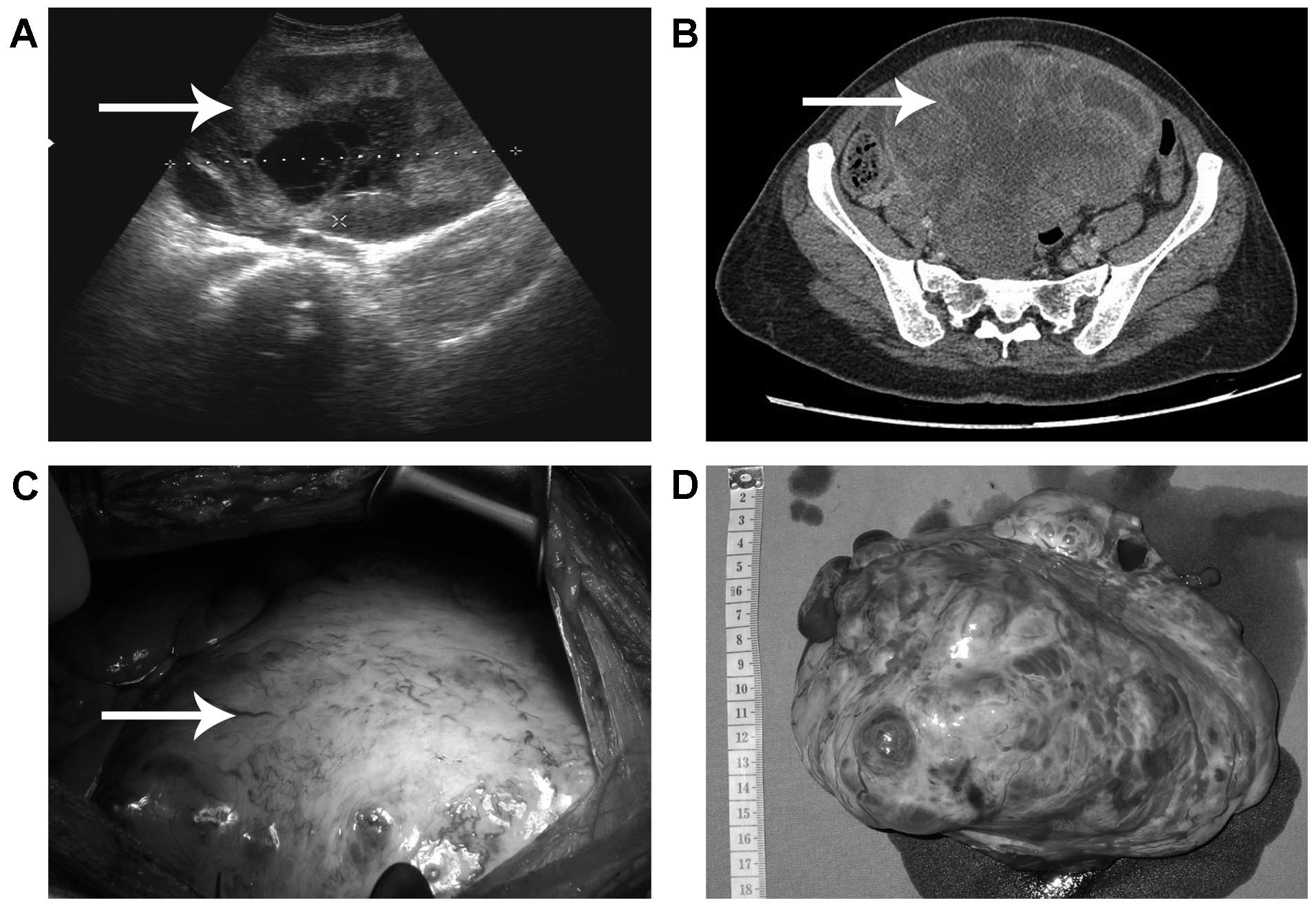
ng/ml) and α-fetoprotein (2.84 ng/ml). TVS revealed a cystic solid
mass measuring 16.0×12.8 cm in the pelvic cavity (Fig. 2A). The patient was admitted to the
Obstetrics and Gynecology Department for further treatment.
Computed tomography demonstrated right ovarian carcinoma in the
pelvic cavity, with cystic and solid portions (Fig. 2B). The patient required surgery, but
refused placement of a perioperative IVC filter due to insufficient
funds. Exploratory laparotomy confirmed the presence of a right
ovarian mass with a maximum diameter of 16.0 cm and 500 ml ascitic
fluid in the abdominal cavity (Fig. 2C
and D). A right oophorectomy was performed and an
intraoperative frozen section was obtained for the confirmation of
diagnosis. The solid and cystic mass exhibited an uneven surface
with excrescences, and the section was comprised of brittle tissue.
Following 30 min of evaluation, pathology confirmed ovarian
epithelial malignancy. Aggressive total hysterectomy, right
salpingectomy, left salpingo-oophorectomy, omentectomy, pelvic and
para-aortic lymph node dissection and appendectomy were performed.
The liver, pancreas, gall bladder, stomach, and small and large
bowel remained normal. No intraoperative peritoneal deposits or
areas suspicious for malignancy were found. Intraoperative bleeding
was 200 ml. Heparin anticoagulation therapy was stopped 12 h prior
to surgery, and resumed 24 h post surgery.
On postoperative day (POD) 1, the patient's DVT
symptoms were significantly relieved, with a decreased difference
in lower limb circumference (left, 30.5 cm; right, 31.5 cm). In
addition the plasma level of D-dimer had been reduced to 4,440.00
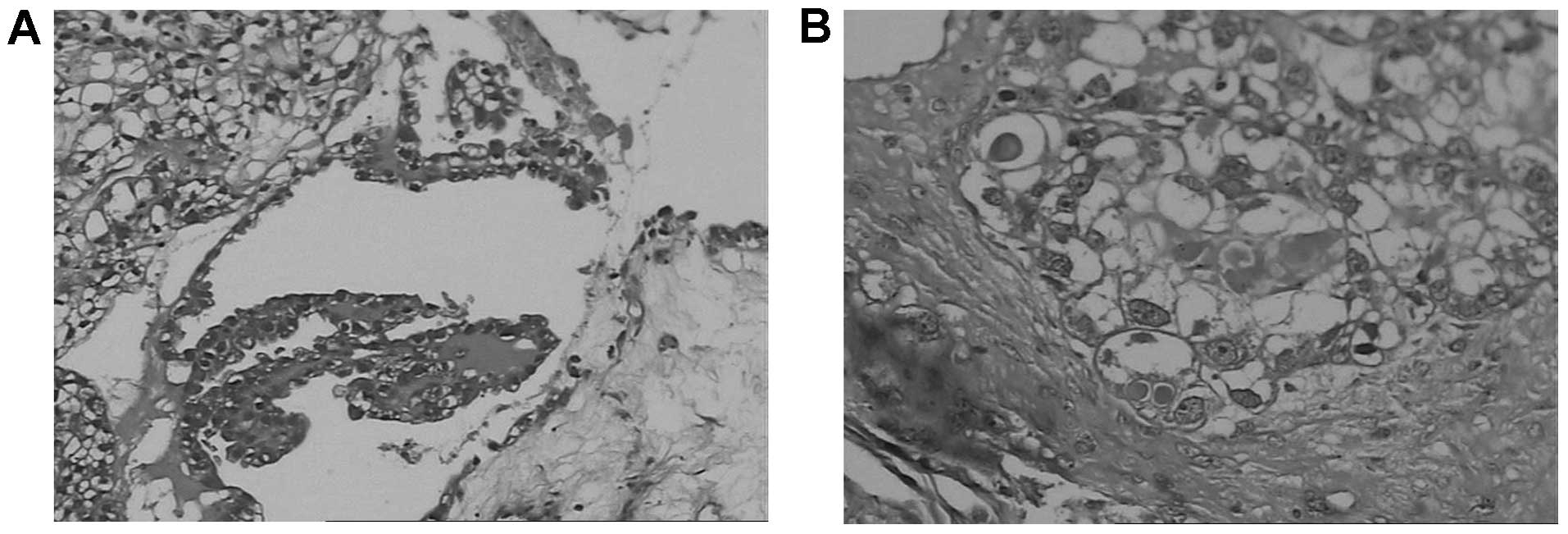
µg/l. Histology of the tumor confirmed ovarian clear cell
adenocarcinoma (Fig. 3A and B) with
left iliac and obturator lymph node metastasis. The patient's
uterus, right adnexa, and omentum majus were negative for
metastasis. The cancer stage was IIIC. The patient received six
cycles of carboplatin (AUC)=6 and docetaxel (175 mg/m2)
every 4 weeks following surgery. Serum tumor markers were measured
following the first cycle of chemotherapy. Serum CA153 had reduced
from 3,000 U/ml to 185.20 U/ml, while CA125 had decreased from
541.5 U/ml to 73.70 U/ml. CA199 and carcinoembryonic antigen levels
were normal. Warfarin oral anticoagulation was continued and the
international normalized ratio was maintained in the treatment
range of 2.0–3.0. All serum tumor marker levels and plasma D-dimer
levels returned to normal following the second cycle of
chemotherapy. The patient was followed-up for >3 years, during
which time serum tumor marker assays and TVS indicated no evidence
of tumor recurrence. The successful outcome of the present case
suggests that ovarian cancer with DVT may be treated with up-front
primary cytoreductive surgery within 1 month of anticoagulant
therapy, without placement of an IVC filter.
Discussion
Venous thromboembolism (VTE), including DVT and PE,
is increasingly recognized as a common complication amongst
patients with malignant disease, and is associated with increased
mortality, recurrence and compromised quality of life (11–13).
Numerous studies have confirmed this association between malignancy
and VTE (12,14,15). The
overall risk for VTE is seven-fold greater in patients with
malignancy, compared with that of individuals without malignancy,
particularly in the first few months following diagnosis, and in
the presence of distant metastases (12). Among solid tumors, ovarian cancer has
one of the highest incidence rates of VTE, an effect which
adversely impacts patient survival (16,17). The
overall incidence of symptomatic DVT among patients with ovarian
cancer is reported to be 9.7–16.6%, with 3.2% of cases detected
prior to the diagnosis of ovarian cancer (3,4). In the
present case, DVT was unresponsive to anticoagulant therapy,
suggesting the prescence of an underlying malignancy. Optimal
cytoreductive surgery without placement of a preoperative IVC
filter was performed, and ovarian cancer was confirmed. This case
suggests that clinicians should suspect underlying malignancy when
DVT is unresponsive to anticoagulant therapy.
Factors contributing to the risk of DVT in cancer
patients include clear cell subtype, high grade and stage of
cancer, high CA125 (>500 IU/ml), giant pelvic mass, history of
DVT, ongoing chemotherapy, lack of surgery, presence of residual
tumor and BMI ≥30 (4). Clear cell
carcinomas are associated with the highest DVT incidence (27.3%),
compared with that of 6.8% among patients with other types of
epithelial ovarian cancer (18). The
present patient exhibited several risk factors for DVT, including
high CA125 level, advanced stage, giant pelvic tumor and clear cell
adenocarcinoma subtype; although had no history of DVT and a normal
BMI. The symptoms of DVT were significantly relieved by POD 1, with
a decreased difference in circumference between the lower limbs,
resulting from decreased pelvic pressure. Tumor-associated
obstruction of venous flow may have a more prominant role in
gynecologic cancer patients than hypercoagulability activation by
tumor cells (19). Clinicians should
be aware of the risk factors for DVT so that appropriate
perioperative prophylactic measures, including anticoagulation
therapy, may be effectively used. Furthermore, in this case,
primary surgery was effective for a resectable giant pelvic mass
with DVT.
However, the management of ovarian cancer associated
with DVT remains challenging. There are currently three approaches
to the management of such cases: i) Up-front primary cytoreductive
surgery with placement of an IVC filter prior to surgery to prevent
PE (20); ii) neoadjuvant
chemotherapy followed by interval debulking surgery for huge tumors
that cannot be treated with optimal primary cytoreductive surgery
(20); and iii) initial less-invasive
diagnostic laparoscopy to remove cancer tissue, followed by three
cycles of chemotherapy and complete staging surgery, an approach
restricted to patients with small ovarian tumors (21). Up-front primary cytoreductive surgery
with preoperative IVC filter placement provides a histopathological
diagnosis, removes as much cancer tissue as possible, establishes
the International Federation of Gynecology and Obstetrics stage
(2), aids complete resection of
macroscopic disease (22) and
improves overall survival (20,23),
compared with the effects of neoadjuvant chemotherapy for
resectable advanced ovarian cancer. However, numerous complications
have been reported to be associated with IVC filters, including IVC
penetration, filter embolization and movement, filter fracture,
recurrent PE and DVT (8,9). Furthermore, perioperative placement of
an IVC filter in patients with ovarian cancer undergoing primary
cytoreductive surgery may significantly decrease survival time and
elevate the risk of DVT and hematogenous distant metastasis
(10). In addition, these patients
should be monitored closely and the filter requires removal once
anticoagulation is no longer contraindicated (24). The use of IVC filters prior to primary
cytoreductive surgery therefore remains controversial.
The present study describes the case of a huge
ovarian tumor with DVT, treated within 1 month of anticoagulant
therapy with optimal primary cytoreductive surgery without
placement of an IVC filter. A preoperative IVC filter was not
placed in this case as the patient did not suffer from clinically
evident PE and the chronic venous thrombi were adhered to the
vessel wall and did not involve the pelvic veins, lowering the risk
of PE (25). In addition, the patient
and family refused placement of an IVC filter due to a lack of
funds. Based on these circumstances, optimal cytoreductive surgery
was performed without placement of a preoperative IVC filter. This
case differed from those of previous studies (20,21). The
patient was followed up for >3 years, during which time serum
tumor marker assays and TVS scans identified no evidence of tumor
recurrence. Although no adverse events have previously been
reported following surgery without placement of an IVC, the number
of cases is too low to draw general conclusions. The present case
is therefore a useful contribution to enhancing understanding of
the treatment of ovarian cancer with DVT.
In conclusion, occult cancer should be suspected in
patients with DVT unresponsive to anticoagulant therapy, and
optimal cytoreductive surgery without placement of a preoperative
IVC filter is a feasible treatment strategy for advanced ovarian
cancer with DVT, when the thrombus strongly adheres to the vessel
wall organization.
Acknowledgements
The present study was supported by the Science and
Technology Development of Guangdong, China (nos. 2011B031800100 and
2011B031800025) and the Nature Science Committee of Guangdong,
China (nos. S2013010015599 and S2012010008270).
References
|
1
|
Jayson GC, Kohn EC, Kitchener HC and
Ledermann JA: Ovarian cancer. Lancet. 384:1376–1388. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
MorganRJ Jr, Alvarez RD, Armstrong DK,
Burger RA, Castells M, Chen LM, Copeland L, Crispens MA, Gershenson
D, Gray H, et al: National Comprehensive Cancer Network: Ovarian
cancer, version 3.2012. J Natl Compr Canc Netw. 10:1339–1349.
2012.PubMed/NCBI
|
|
3
|
Tateo S, Mereu L, Salamano S, Klersy C,
Barone M, Spyropoulos AC and Piovella F: Ovarian cancer and venous
thromboembolic risk. Gynecol Oncol. 99:119–125. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
AbuSaadeh F, Norris L, O'Toole S and
Gleeson N: Venous thromboembolism in ovarian cancer: Incidence,
risk factors and impact on survival. Eur J Obstet Gynecol Reprod
Biol. 170:214–218. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dewdney SB, Benn T, Rimel BJ, Gao F, Saad
N, Vedantham S, Mutch DG and Zighelboim I: Inferior vena cava
filter placement in the gynecologic oncology patient: A 15-year
institutional experience. Gynecol Oncol. 121:344–346. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sing RF and Fischer PE: Inferior vena cava
filters: Indications and management. Curr Opin Cardiol. 28:625–631.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Duffett LD, Gándara E, Cheung A, Bose G,
Forster AJ and Wells PS: Outcomes of patients requiring insertion
of an inferior vena cava filter: A retrospective observational
study. Blood Coagul Fibrinolysis. 25:266–271. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sella DM and Oldenburg WA: Complications
of inferior vena cava filters. Semin Vasc Surg. 26:23–28. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee JK, So YH, Choi YH, Park SS, Heo EY,
Kim DK and Chung HS: Clinical course and predictive factors for
complication of inferior vena cava filters. Thromb Res.
133:538–543. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Matsuo K, Carter CM, Ahn EH, Prather CP,
Eno ML, Im DD and Rosenshein NB: Inferior vena cava filter
placement and risk of hematogenous distant metastasis in ovarian
cancer. Am J Clin Oncol. 36:362–367. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Noble S and Pasi J: Epidemiology and
pathophysiology of cancer-associated thrombosis. Br J Cancer. 102
(Suppl 1):S2–S9. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Blom JW, Doggen CJM, Osanto S and
Rosendaal FR: Malignancies, prothrombotic mutations, and the risk
of venous thrombosis. JAMA. 293:715–722. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Arora M and Wun T: Adverse impact of
venous thromboembolism on patients with cancer. Semin Thromb
Hemost. 40:313–318. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bierry G, Holl N, Kellner F, Riehm S,
Roedlich MN, Greget M and Veillon F: Venous thromboembolism and
occult malignancy: Simultaneous detection during pulmonary CT
angiography with CT venography. AJR Am J Roentgenol. 191:885–9.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Murchison JT, Wylie L and Stockton DL:
Excess risk of cancer in patients with primary venous
thromboembolism: A national, population-based cohort study. Br J
Cancer. 91:92–95. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Metcalf RL, Fry DJ, Swindell R, McGurk A,
Clamp AR, Jayson GC and Hasan J: Thrombosis in ovarian cancer: A
case control study. Br J Cancer. 110:1118–1124. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gunderson CC, Thomas ED, Slaughter KN,
Farrell R, Ding K, Farris RE, Lauer JK, Perry LJ, McMeekin DS and
Moore KN: The survival detriment of venous thromboembolism with
epithelial ovarian cancer. Gynecol Oncol. 134:73–77. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Matsuura Y, Robertson G, Marsden DE, Kim
SN, Gebski V and Hacker NF: Thromboembolic complications in
patients with clear cell carcinoma of the ovary. Gynecol Oncol.
104:406–410. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
AbuSaadeh F, Norris L, O'Toole S, Mohamed
BM, Langhe R, O'Leary J and Gleeson N: Tumour expression of tissue
factor and tissue factor pathway inhibitor in ovarian cancer -
relationship with venous thrombosis risk. Thromb Res. 132:627–634.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hurtt CC, Cliby WA, Weaver AL, McGree M,
Martin J and Bakkum-Gamez JN: Management of epithelial ovarian
cancer in the setting of concomitant venous thromboembolism. Obstet
Gynecol. 123 (Suppl 1):183S–184S. 2014. View Article : Google Scholar
|
|
21
|
Ha JE, Lee YS, Lee HN and Park EK:
Diagnostic laparoscopy of patient with deep vein thrombosis before
diagnosis of ovarian cancer: A case report. Cancer Res Treat.
42:48–52. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Vergote I, Tropé CG, Amant F, Kristensen
GB, Ehlen T, Johnson N, Verheijen RH, van der Burg ME, Lacave AJ,
Panici PB, et al: European Organization for Research and Treatment
of Cancer-Gynaecological Cancer Group; NCIC Clinical Trials Group:
Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV
ovarian cancer. N Engl J Med. 363:943–953. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
vanMeurs HS, Tajik P, Hof MH, Vergote I,
Kenter GG, Mol BW, Buist MR and Bossuyt PM: Which patients benefit
most from primary surgery or neoadjuvant chemotherapy in stage IIIC
or IV ovarian cancer? An exploratory analysis of the European
Organisation for Research and Treatment of Cancer 55971 randomised
trial. Eur J Cancer. 49:3191–3201. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
AlHakim R, Kee ST, Olinger K, Lee EW,
Moriarty JM, McWilliams JP and AI-Hakim R: Inferior vena cava
filter retrieval: Effectiveness and complications of routine and
advanced techniques. J Vasc Interv Radiol. 25:933–939. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Köhn H, König B and Mostbeck A: Incidence
and clinical feature of pulmonary embolism in patients with deep
vein thrombosis: A prospective study. Eur J Nucl Med. 13
(Suppl):S11–S15. 1987. View Article : Google Scholar : PubMed/NCBI
|