Introduction
Due to its versatility, the pedicled pectoralis
major myocutaneous (PMMC) flap is extensively used for the
treatment of surgical defects resulting from oral and maxillofacial
cancer ablation (1). Despite the fact
that microvascularized free-tissue transfer is increasingly
becoming the main flap method for oral, head and neck cancer
reconstruction, this method cannot be used effectively in certain
situations, including recurrence following reconstruction
(salvage), in the presence of poor systemic or local conditions,
following full-dose radiotherapy, in patients with arteriosclerosis
or in the elderly (1,2).
Numerous clinicians have criticized the PMMC flap
due to its relatively high rate of fistula formation, bulkiness of
the muscle pedicle and adipose layer, disfiguring donor-site
morbidity, and relatively high potential (15–32%) for distal or
marginal flap necrosis with partial flap loss, as a result of
vascular insufficiency (1,3). In addition, the limited arc of rotation
results in reduced flexibility following oral and maxillofacial, or
head and neck reconstruction, compared with free-tissue transfer
methods (2,3). The PMMC flap was initially described by
Ariyan (4) in 1979, and has since
been used for salvage and advanced primary reconstruction, with
numerous technical modifications based on 3-dimensional blood
circulation (2,5).
Kiyokawa et al (5) and Rikimaru et al (6) improved the restricted range of the PMMC
flap rotation arc by developing a novel method of flap elevation
and transfer, in order to extend its range and degree of
flexibility whilst maintaining stable blood circulation in the skin
paddle. This was achieved by moving the flap to the reconstruction
site via the subclavian route, which provides a high degree of
flexibility with a greater rotation arc and ~8 cm extension,
compared with the original method described by Ariyan (4).
A further drawback of the PMMC flap is vascular
insufficiency due to unstable blood supply, which may result in the
partial loss of the distal and marginal parts of the flap. This is
particularly a problem when the flap is harvested from the caudal
vascular territory (far caudal from the fourth costal cartilage to
the seventh) through the choke vessels of communicating vessels in
an axial pattern based on the angiosome concept (2,3,6). As a result, unreasonable tension in the
skin paddle may lead to partial distal or marginal necrosis
(5). Kiyokawa et al (5) and Rikimaru et al (6) partially resolved this problem by
designing a skin paddle that included a large number of perforating
branches, which is suitable regardless of the size of the flap.
Studies of 3-dimensional blood circulation and cadaver anatomy have
demonstrated that preservation of the lateral thoracic artery, in
addition to the conventional technique for head and neck
reconstruction, stabilizes the blood supply to the distal (caudal)
part of the flap without compromising pedicle length (2,6).
In the present study, a simple modification of the
conventional PMMC flap harvesting method, which is able to overcome
the weaknesses of the flap, is reported. In the modified method,
the blood supply is secured by preserving the lateral thoracic
vessels and using the subclavian route. In addition, the rotation
arc is increased for oral and maxillofacial reconstruction.
Case report
Study approval
The present study was approved by the Ethical
Committee of Shimane University Faculty of Medicine (Izumo,
Shimane, Japan) (study no. 1522). Written informed consent for
publication of the clinical images was provided by the patient.
Patient presentation
The patient, a 57-year-old Japanese female affected
by oral cancer, was admitted to the Department of Oral and
Maxillofacial Surgery of Shimane University Hospital (Izumo, Japan)
on December 19th 2013, and subjected to PMMC flap
reconstruction.
Surgical technique
When harvesting the PMMC flap, the pectoralis major
muscle was elevated from the chest wall and moved upward, as in the
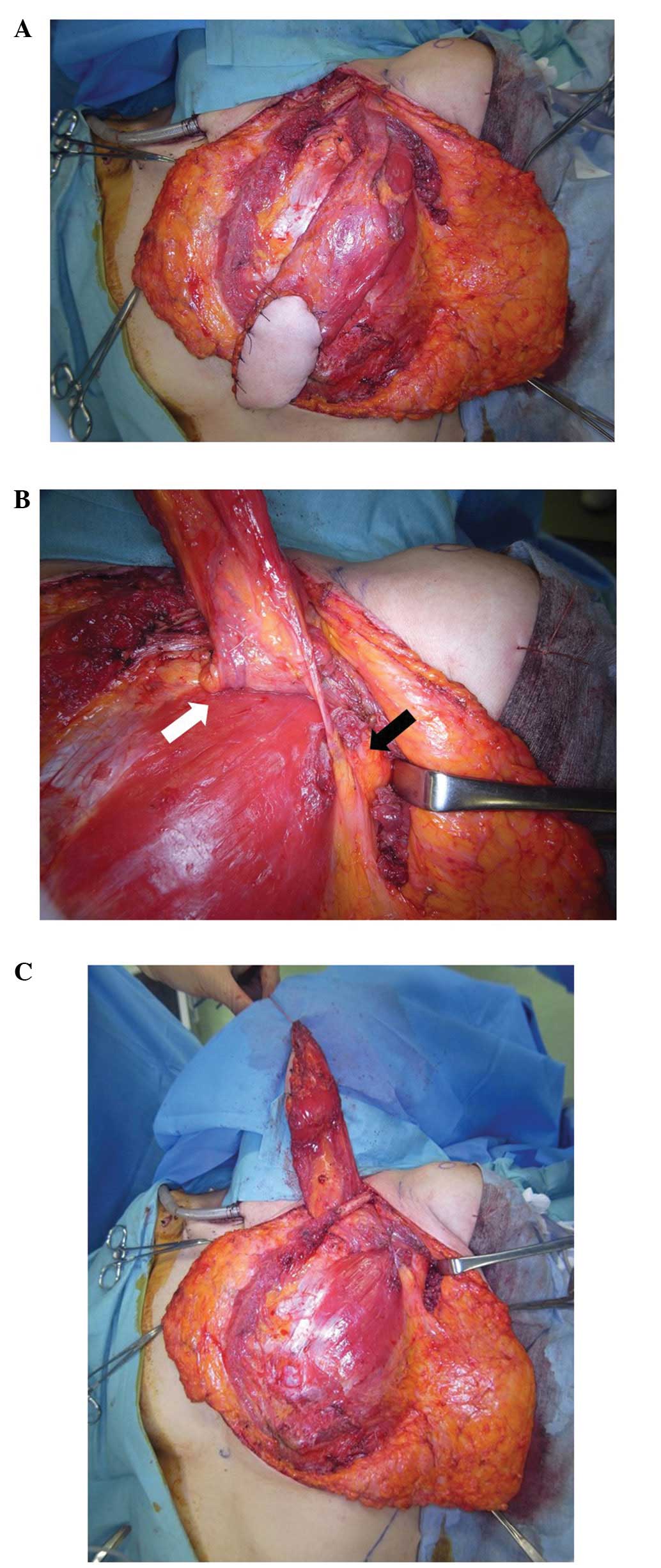
conventional surgical technique (Fig.
1A). The lateral thoracic vessels were identified beneath the
lateral border of the pectoralis major muscle in the region of the
axilla. The pectoral part of the pectoralis major muscle was
divided lateral to the lateral thoracic artery, and medial to the
pectoral branch of the thoracoacromial artery up to the clavicular
part of the muscle. The clavicular part of the pectoralis major
muscle overlying the pectoral branch of the thoracoacromial artery
was then divided up to the clavicle using the true-island PMMC flap
technique described by Wei et al (7). In the conventional flap preparation
technique, the lateral thoracic artery, which runs upward beneath
the lateral border of the pectoralis minor muscle, is sacrificed at
this stage, since it limits the length of the flap pedicle. The
pectoralis minor muscle may be divided around the lateral thoracic
vessels to release them, as depicted in Fig. 1B. Subsequently, the clavicular
periosteum around the pectoral branches of the thoracoacromial
vessels was excised from the cervical and thoracic sides, and the
periosteum on the inferior surface of the clavicle was detached and
reflected in order to drop downward, as described by Kiyokawa et
al (5). This procedure enables
the safe transfer of the PMMC flap and its rotation toward the oral
and maxillofacial region under the clavicle without damaging the
subclavian vessels (Fig. 1C).
Furthermore, it enables the PMMC flap to safely reach the entire
oral cavity, including the infraorbital region, palate, middle
pterygopalatine fossa and nasopharynx, with no distal vascular
insufficiency.
This modified surgical approach has been performed
on 7 patients at the Department of Oral and Maxillofacial Surgery
of Shimane University Hospital, and no post-surgery complications
have been observed thus far. Regarding the surgical procedure, the
double-pedicled PMMC flap reconstruction with transfer via a
subclavian route was routinely followed by tracheostomy, radical
neck dissection for metastatic lymph nodes and en bloc
complete margin-free cancer ablation surgery, as in the present
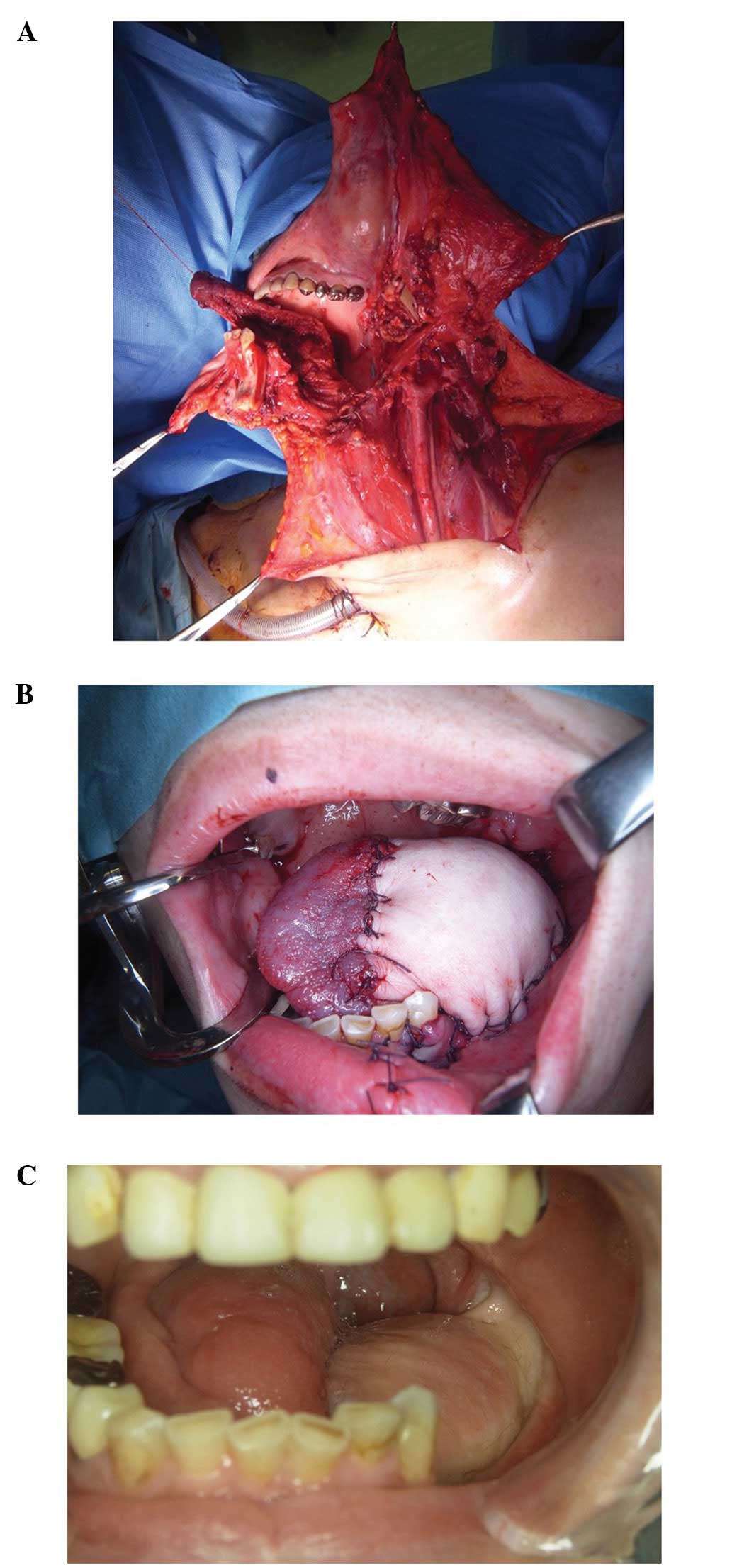
case (Fig. 2A and B). The
postoperative adjuvant treatments were performed according to the
current National Comprehensive Cancer Network Guidelines (8). The patients were subjected to regular
postoperative clinical follow-up with functional assessment. In the
present case, good functional tongue mobility with no fistulas was
observed 6 months after surgery (Fig.
2C). However, the patient succumbed to distant metastases 9
months after undergoing surgery.
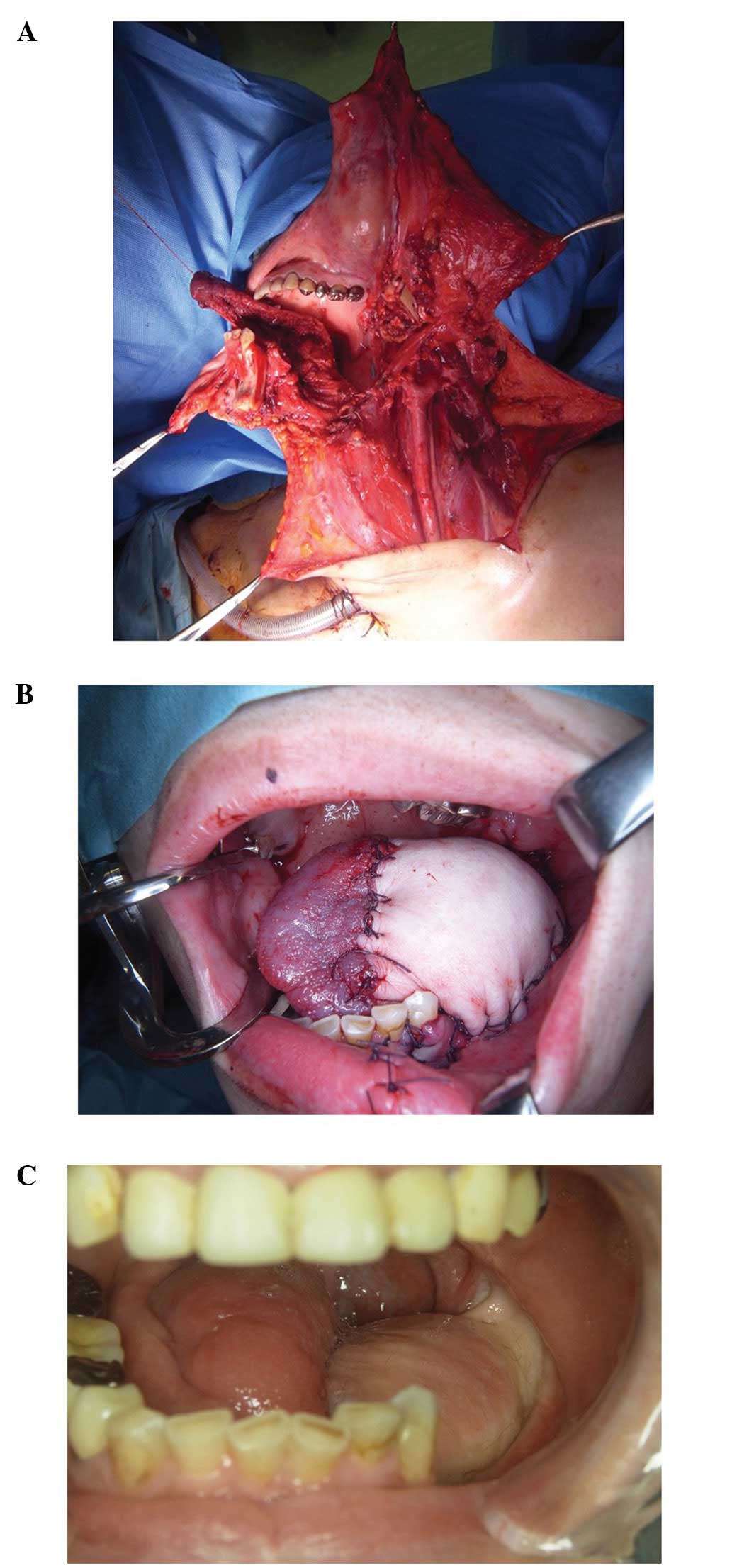 | Figure 2.(A) Patient with two advanced types of
cancer (tongue squamous cell carcinoma with multiple ipsilateral
cervical LNMs, cT4aN2bM0, stage IVa; and rectum adenocarcinoma with
LNM, cT3N2M0, stage IIIb) was subjected to pedicled PMMC flap
reconstruction with a temporary mandibular reconstruction plate,
followed by tracheostomy, radical neck dissection for multiple LNMs
(levels I–V), en bloc complete margin-free cancer ablation
surgery (comprising a subtotal glossectomy and segmental resection
of the mandible) and surgical treatment of the rectum
adenocarcinoma. (B) Elevated PMMC flap was transferred to the
reconstruction site via a subclavian route, and water-tight closure
was performed. (C) Intraoral image at 6 months post-surgery,
indicating good functional tongue mobility with no fistulas. LNM,
lymph node metastasis; PMMC, pectoralis major myocutaneous. |
Discussion
Despite the wide clinical application of the PMMC
flap in oral, head and neck reconstructive surgery, numerous PMMC
flaps have been observed to develop partial distal necrosis and
display limited flexibility (1,3). Although
the restricted range of rotation reported in the original technique
was resolved with the development of the subclavian route, the
blood supply to the distal (caudal) portion of the PMMC flap
remained problematic (1,5). Anatomical studies have aided to improve
PMMC flap preparation (6). In
particular, Yang et al (9) and
Elazab and Nabil (10) demonstrated
that the pectoral branches of the thoracoacromial trunk vessels
arising from the first and second parts of the axillary artery
provide the main blood supply to the skin paddle island and the
overlying upper part of the pectoralis major muscle. Although the
anterior intercostal branches of the internal mammary artery supply
blood to ~43% of the skin territory overlying the medial and lower
parts of the PMMC flap, the lateral thoracic artery is often the
main blood supply to the lateral and lower parts of the pectoralis
major muscle, overlying the paddle skin in ~6.6% of PMMC flaps
(3,9,10).
Previous studies have demonstrated that the distal
segment of the pectoralis major muscle is supplied by the pectoral
branch of the thoracoacromial, axillary and lateral thoracic artery
in 90, 67 and 40% of cases, respectively (3,9,10). Po-Wing Yuen (3) reported a simple technique for preserving
the lateral thoracic artery during PMMC flap harvesting. In this
technique, the lateral thoracic artery is identified and elevated
subsequent to dividing the overlying pectoralis minor muscle, and
the lateral thoracic artery and pectoralis branch of the
thoracoacromial artery that is part of the double pedicled flap are
then rotated upward through the supraclavian root via a
subcutaneous tunnel (3). Makiguchi
et al (11) developed the
‘supercharged PMMC flap’ technique, which preserves the lateral
thoracic artery by tracing the lateral thoracic vessels upward near
the bifurcation of the subclavian vessels. At this location, the
vessels are sectioned and anastomosed to the cervical vessels to
create a conventionally prepared PMMC flap nourished by the
dominant thoracoacromial vessels. In addition, the vessels are also
rotated upward through the supraclavian root via a subcutaneous
tunnel, similar to that described in the modified method of Po-Wing
Yuen (3). Therefore, preserving the
lateral thoracic artery during PMMC flap harvesting to improve the
distal blood supply is reasonable. The Department of Oral and
Maxillofacial Surgery of Shimane University Hospital has been using
this modified technique over the conventional microvascularized
free flap reconstruction technique since 2013. To date, seven
patients with advanced or recurrent oral cancer, a number of whom
were elderly, have been treated with this modified technique, and
no flap problems or necrosis have been observed. Since the
technique described in the present study involves dividing the
branches of the internal mammary and axillary arteries, the
potential risks of partial distal flap necrosis have not been
completely overcome. However, preservation of the lateral thoracic
vessels, which may be major contributors of blood supply to the
distal and lateral parts of the PMMC flap and skin paddle, is
advantageous.
In conclusion, the modification of the PMMC flap
technique described in the present study has been demonstrated to
preserve the lateral thoracic vessels without limiting the rotation
arc of the flap, due to the use of the subclavian route.
Furthermore, this modified technique is simpler and safer than
those that divide the pectoralis minor muscle, or section and
anastomose the lateral thoracic vessels.
Acknowledgements
The authors of the present study would like to thank
all of the participants. The present study was in part supported by
Grant-in-Aid for Scientific Research (KAKENHI) and Young Scientists
(B; grant no. 25870452 to Dr Takahiro Kanno).
References
|
1
|
Jena A, Patnayak R, Sharan R, Reddy SK,
Manilal B and Rao LM: Outcomes of pectoralis major myocutaneous
flap in female patients for oral cavity defect reconstruction. J
Oral Maxillofac Surg. 72:222–231. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rikimaru H, Kiyokawa K, Watanabe K, Koga
N, Nishi Y and Sakamoto A: New method of preparing a pectoralis
major myocutaneous flap with a skin paddle that includes the third
intercostal perforating branch of the internal thoracic artery.
Plast Reconstr Surg. 123:1220–1228. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yuen Po-Wing A: Preservation of lateral
thoracic artery to improve vascular supply of distal skin without
compromising pedicle length in harvesting pectoralis major
myocutaneous flap. J Plast Reconstr Aesthet Surg. 59:1433–1435.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ariyan S: The pectoralis major
myocutaneous flap. A versatile flap for reconstruction in the head
and neck. Plast Reconstr Surg. 63:73–81. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kiyokawa K, Tai Y, Tanabe HY, Inoue Y,
Yamauchi T, Rikimaru H, Mori K and Nakashima T: A method that
preserves circulation during preparation of the pectoralis major
myocutaneous flap in head and neck reconstruction. Plast Reconstr
Surg. 102:2336–2345. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rikimaru H, Kiyokawa K, Inoue Y and Tai Y:
Three-dimensional anatomical vascular distribution in the
pectoralis major myocutaneous flap. Plast Reconstr Surg.
115:1342–1354. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wei WI, Lam KH and Wong J: The true
pectoralis major myocutaneous island flap: An anatomical study. Br
J Plast Surg. 37:568–573. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
National Comprehensive Cancer Network
(NCCN) Clinical Practice Guidelines in Oncology: Head and Neck
Cancers. Version 2. NCCN (Fort Washington, USA). 16–20. 2013.
|
|
9
|
Yang D, Marshall G and Morris SF:
Variability in the vascularity of the pectoralis major muscle. J
Otolaryngol. 32:12–15. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Elazab EEB and Nabil NM: Pectoralis major
muscle: Anatomical features of its arterial supply. Eur J Plast
Surg. 35:9–18. 2012. View Article : Google Scholar
|
|
11
|
Makiguchi T, Yokoo S, Miyazaki H, Takayama
Y, Ogawa M, Hashikawa K and Terashi H: Supercharged pectoralis
major musculocutaneous flap. J Craniofac Surg. 24:e179–e182. 2013.
View Article : Google Scholar : PubMed/NCBI
|