Introduction
Cerebellar liponeurocytoma is a rare tumor of the
central never system. Since it was first reported in 1978 (1), several names had been applied, such as
lipomatous medulloblastoma, medullocytoma, neurolipocytoma,
lipomatous glioneurocytoma and lipidized mature neuroectodermal
tumor of the cerebellum (1). In 2000,
The World Health Organization (WHO) classified this rare tumor as a
distinctive entity, prior to characterizing it as a grade II tumor
in 2007 (2). Cerebellar
liponeurocytoma is most commonly found in adults, without gender
predominance (2–4). Patel et al (4) revealed that 42 cases of cerebellar
liponeurocytoma were reported in the English literature between
1978 and 2009, with a male to female ratio of 22:20. Clinical
symptoms include the symptoms of the cerebellar dysfunction, such
as gait disturbance and uncoordinated movements, which are slowly
progressive and generally not detected in the early stages of the
disease. Vomiting and progressive visual symptoms begin to present,
as a result of increased cranial pressure in the later stages of
the disease (5). Preclinical
diagnosis is difficult as to date, no typical imaging features have
been identified, however, Aker et al (3) reported that the lesion exhibited
heterogeneous enhancement on T1-weighted images (3). Pathologically, the tumor is
characterized by the focal accumulation of adiposities in an
otherwise typical small cell tumor, similar to central neurocytoma,
with cerebella and supratentorial locations (2–3). The
current preferred treatment strategy is radical surgery, and
adjuvant radiotherapy is recommended in cases of residual tumor. As
the tumor has potentially long-term malignant characteristics,
close follow-up is recommended (2–4). However,
the clinical characteristics and optimal treatment strategy of the
cerebellar liponeurocytoma remain unclear. The present study
reports a case located in the foramen magnum region, and also
provides a review of the literature.
Case report
A 45-year-old female was referred to the Department
of Neurosurgery of Beijing Tiantan Hospital (Capital Medical
University, Beijing, China) in September 2011 complaining of
occipital headaches that had persisted for ~18 months. Paresthesia
of the left hand was exhibited prior to slow progression to the
other limb, which was associated with debilitation and
breathlessness for ~6 months. The patient had a history of
hypertension for ~3 years, which was controlled with a dietary
regimen, exercise therapy and blood pressure monitoring. Upon
clinical examination, the patient presented with a hoarse voice,
occasional deglutition, diminished pinprick sensations in the right
arm and leg, and acroaesthesia of the left side. Muscle strength
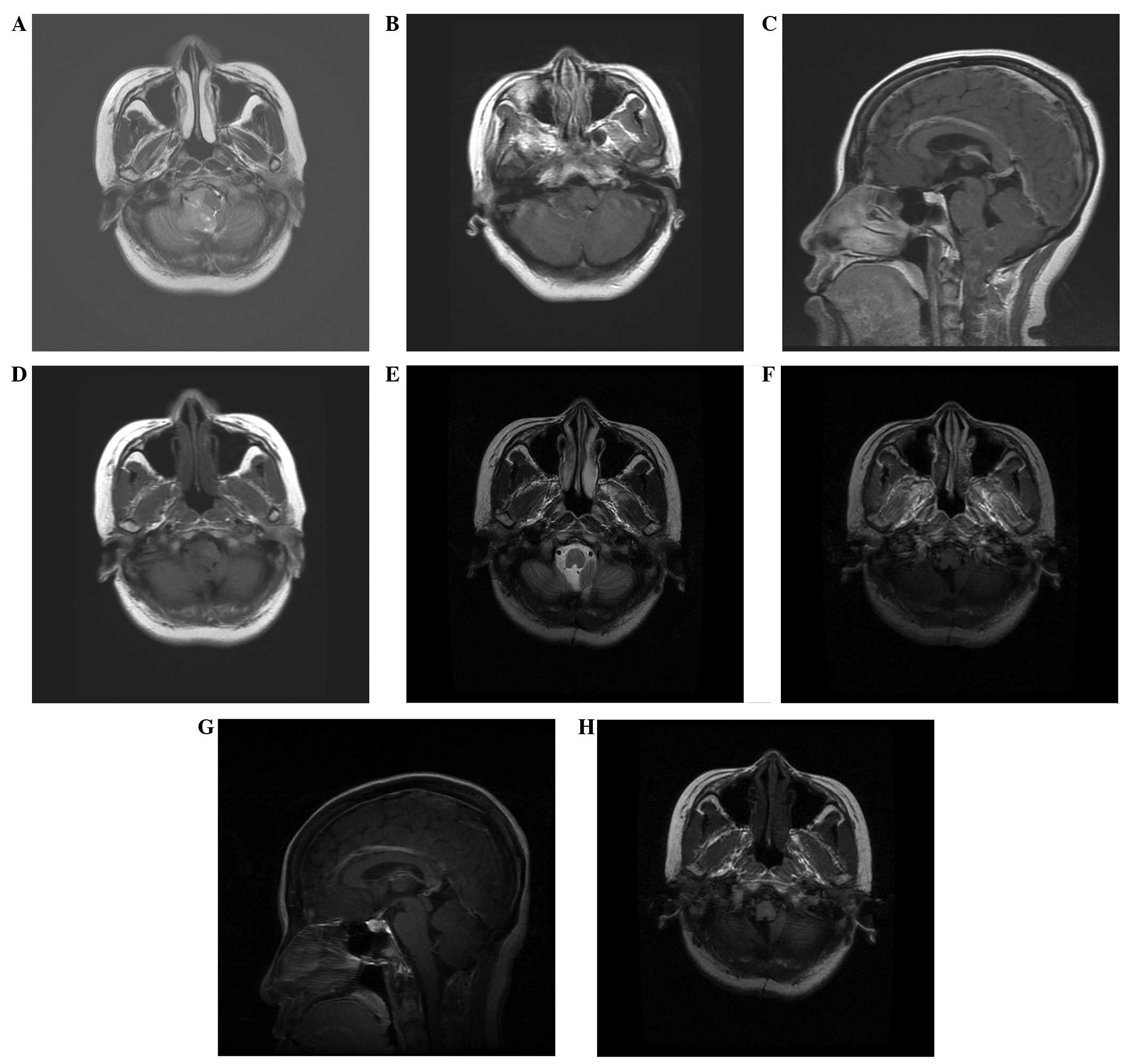
was normal, however, a broad-based gait was noted. Magnetic
resonance imaging (MRI) revealed an isointense lesion with a sparse
hypointense signal on T1-weighted imaging (WI) and slightly
heterogeneous enhancement on enhanced T1WI. On T2WI, the lesion was
slightly hyperintense compared with the cortex (Fig. 1A–D). The lesion was ~4.5×2.5×2.0 cm in
size, occupying the right hemisphere of the cerebellum and the
inferior vermis, compressing the medulla oblongata from the right
side, and extending through the foramen magnum to the C2 level. The
lesion was well-marginated, as shown by the T2WI, without apparent
edema, and no signs of obstructive hydrocephalus were found.
The patient underwent a total resection of the tumor
through the midline suboccipital approach, which extended downward
to the C2 level. During the surgery, the gross appearance of the
tumor was noted to be soft and moderately vascularized, with a
yellowish color. The tumor was derived from the right cupula region
of the fourth ventricle, well demarcated from the surrounding
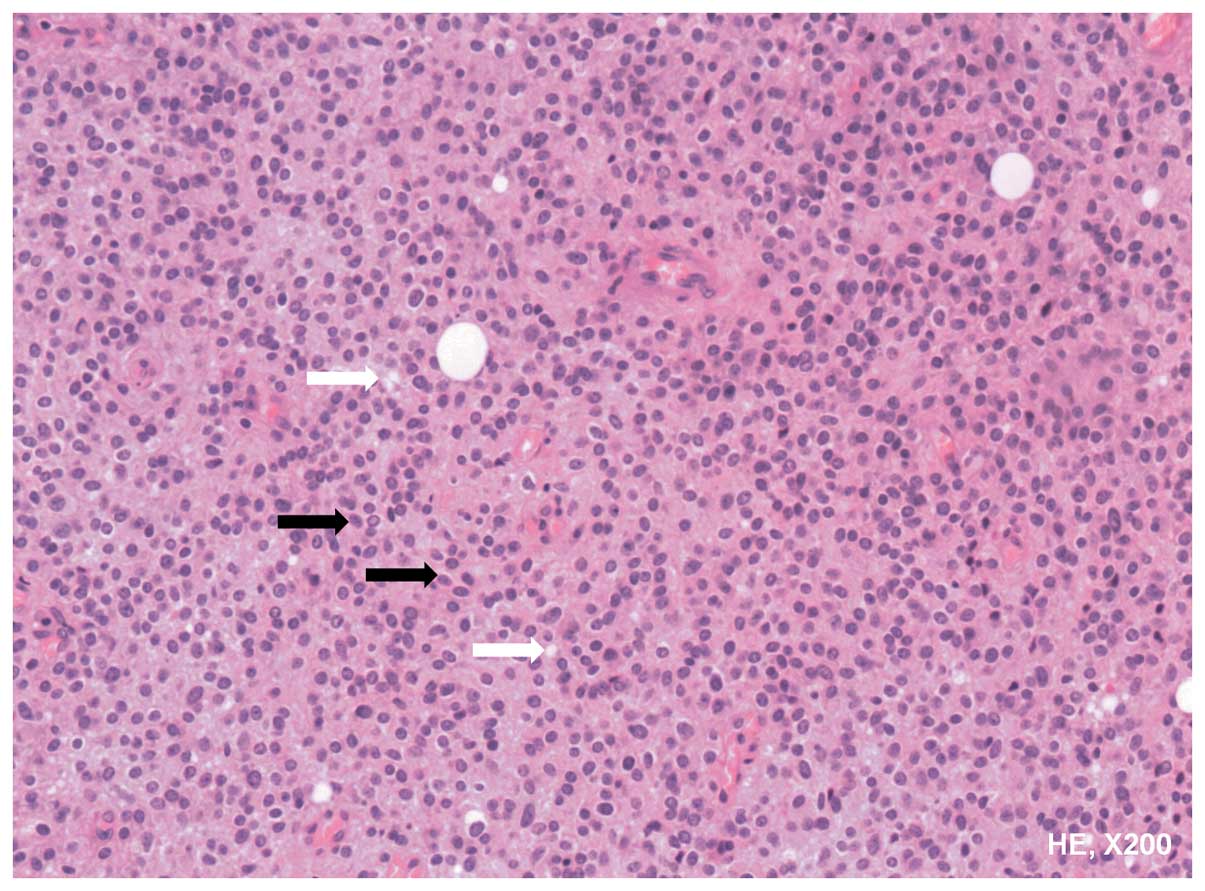
parenchyma, without close adherence to the parenchyma. Microscopic
examination showed monotonous small round cells with slightly
eosinophilic cytoplasm. The lipomatous cells were localized focally
(Fig. 2). Immunohistochemistry was
positive for synaptophysin, S-100 and neuronal nuclear antigen,
partially positive for Olig-2, and negative for glial fibrillary
acidic protein and epithelial membrane antigen. The Ki-67 index was
low (<5%). The post-operative period was uneventful, with
notable improvement of the main symptoms; however, the hoarse voice
remained unchanged. Following the total resection of the tumor,
radiation therapy was not recommended, and at the 6-month
follow-up, there was no evidence of tumor recurrence. In the latest
follow-up at 3 years post-surgery, the patient's hoarse voice was
significantly recovered and no signs of tumor recurrence were found
(Fig. 1E–H).
Discussion
Little is known with regard to cerebellar
liponeurocytoma due to its rarity. As its name implies, cerebellar
liponeurocytoma often occurs in the cerebellum, occupying the
cerebellar hemisphere, with repletion of the fourth ventricle,
causing the clinical symptoms of cranial hypertension and
cerebellar symptoms (2,3). The mean age at diagnosis is ~49 years,
and the majority of patients are >30 years (4). According to the study by Patel et
al, in which 42 cases of liponeurocytoma from the literature
were reviewed in 2009, there is no gender predominance (4). The WHO classified cerebellar
liponeurocytoma as a grade II tumor, with a tendency to recur in
the follow-up period (2).
There has been controversy with regard to the
location of cerebellar liponeurocytoma, partly due to its rarity.
At first, this tumor appeared to be specifically located to the
cerebellum. However, there have been 11 cases reported in an
extracerebellar location (5,6). Kuchelmeister et al reported a
case located in the lateral ventricle, and confirmed that the
liponeurocytoma was not an exclusively cerebellar neoplasm
(7). The most notable points with
regard to liponeurocytomas of the supratentorial intraventricular
region is that there is an absence of calcification and a lack of
lipid components when compared with the cerebellar compartment
(7). Although the majority of cases
in the literature have been located in the cerebellar area,
recently, certain studies have suggested that the tumor may be
located supratentorially and subtentorially, and should be renamed
as solely liponeurocytoma (5–7).
The tumor has a recurrent nature, although this
occurs in the long term, with a mean time until recurrence of ~8.5
years (2). Limaiem et al
reported a recurrent cerebellar liponeurocytoma with supratentorial
extension, and upon reviewing all 9 recurrent cases presented in
the literature, the study suggested that the tumor may recur due to
mitoses present in the lesion and >10% Ki-67-positive cells
(2). However, one confusing element
was that, even when treated with total resection, recurrence
appeared unavoidable, showing that the cerebellar liponeurocytoma
was similar to a malignant lesion (3). To a certain extent, the recurrent tumors
were more malignant than the primary lesions, as indicated by the
proliferation index and the recurrence period following the second
surgery. Anghileri et al reported a case in which a complete
resection was performed, and where recurrence was experienced at 8
years and metastasis at 11 years post-surgery, respectively
(8). This suggested that the
liponeurocytoma was a lesion of uncertain malignant potential.
Châtillon et al analyzed 20 cases, and
reported a high recurrence rate in the group treated by gross total
resection alone and in the group treated by subtotal resection
(9). Although there is no such
comparison for the surgery and radiation, there is a trend showing
that post-operative radiotherapy benefits the outcome, as suggested
by Jackson et al (10). Genc
et al reported 2 cases of cerebellar liponeurocytoma with
post-surgery γ-knife therapy, and observed that the tumors
diminished in size after a follow-up time of 12 and 53 months,
respectively (11). However, certain
studies believe that since the recurrence of the tumor occurs in
the long term, adjuvant radiation is too aggressive following the
initial gross total resection (2–4,9). Considering that there is no evidence to
support the use of adjuvant radiation in the prevention of
recurrence and due to the side-effects of radiation, the majority
of studies in the literature recommended a gross total resection,
with a focus on quality of life, and a long-term follow-up plan
(7–9).
When recurrence was observed, repeat surgery and adjuvant radiation
was recommended, as the pathology of the recurrence was always more
aggressive than the primary tumor (10–12).
The treatment strategy for the present patient was
surgery and close follow-up, since a total resection was achieved,
as confirmed intraoperatively and by post-operative MRI, and
secondly, since the Ki-67 was low. Radiation therapy was not
recommended and close observation was maintained during the
follow-up for the subsequent 3 years; no signs of recurrence were
found. This treatment strategy was in accordance with those in the
literature (7–9), and is recommended for primary tumors
with complete resection, in order to avoid aimless radiation and
protect the brain.
In summary, the present study reported a case of
cerebellar liponeurocytoma that was successfully treated by total
resection. A review of the literature showed that cerebellar
liponeurocytoma is rare and may located supratentorially or
subtentorially. The optimal treatment strategy appears to be a
total resection and close follow-up, while radiation is recommended
when there is residual tumor, recurrence or a high Ki-67. However,
due to the rarity of the tumor and limited data available,
long-term follow-up is required.
Acknowledgements
This study was supported, in part, by the Research
Special Fund For Public Welfare Industry of Health, China (grant
no. 201402008 to Junting Zhang) and the Capital Characteristic
Clinic Project, China (grant no. Z131107002213179 to Zhen Wu).
References
|
1
|
Bechtel JT, Patton JM and Takei Y: Mixed
mesenchymal and neuroectodermal tumor of the cerebellum. Acta
Neuropathol. 41:261–263. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Limaiem F, Bellil S, Chelly I, Bellil K,
Mekni A, Jemel H, Haouet S, Zitouna M and Kchir N: Recurrent
cerebellar liponeurocytoma with supratentorial extension. Can J
Neurol Sci. 36:662–665. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aker FV, Ozkara S, Eren P, Peker O,
Armağan S and Hakan T: Cerebellar liponeurocytoma/lipodized
medulloblastoma. J Neurooncol. 71:53–59. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Patel N, Fallah A, Provias J and Jha NK:
Cerebellar liponeurocytoma. Can J Surg. 52:E117–E119.
2009.PubMed/NCBI
|
|
5
|
Pankaj R, Jindal A and Banerjee AK:
Liponeurocytoma of lateral ventricle. Neurol India. 58:805–806.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Karabagli P, Sav A and Pamir N: Does
‘cerebellar liponeurocytoma’ always reflect an expected site? An
unusual case with a review of the literature. Folia Neuropathol.
52:101–105. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kuchelmeister K, Nestler U, Siekmann R and
Schachenmayr W: Liponeurocytoma of the left lateral ventricle -
case report and review of the literature. Clin Neuropathol.
25:86–94. 2006.PubMed/NCBI
|
|
8
|
Anghileri E, Eoli M, Paterra R, Ferroli P,
Pollo B, Cuccarini V, Maderna E, Tringali G, Saini M, Salsano E and
Finocchiaro G: FABP4 is a candidate marker of cerebellar
liponeurocytomas. J Neurooncol. 108:513–519. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Châtillon CE, Guiot MC, Roberge D and
Leblanc R: Cerebellar liponeurocytoma with high proliferation
index, Treatment options. Can J Neurol Sci. 36:658–661. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jackson TR, Regine WF, Wilson D and Davis
DG: Cerebellar liponeurocytoma. Histopathology. J Neurosurg.
95:700–703. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Genc A, Bozkurt SU, Karabagli P, Seker A,
Bayri Y, Konya D and Kilic T: Gamma knife radiosurgery for cranial
neurocytomas. J Neurooncol. 105:647–657. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chung SB, Suh YL and Lee JI: Cerebellar
liponeurocytoma with an unusually aggressive histopathology, Case
report and review of the literature. J Korean Neurosurg Soc.
52:250–253. 2012. View Article : Google Scholar : PubMed/NCBI
|