Introduction
Tumors of the spine are defined as an abnormal mass
of tissue within or surrounding the spinal cord or spinal column
(1). Spine tumors may be
characterized according to the location in which they occur, such
as the lumbar and sacral regions. The majority of spinal tumors
have an unknown cause, however, exposure to cancer-causing agents
may be involved (2). The most
frequent symptom of spinal tumors is non-mechanical back pain,
particularly in the middle or lower back (2). Usually a combination of radiological and
medical examinations, which focus on back pain and neurological
deficits, are used to diagnose tumors of the spine (3). At present, both surgical and nonsurgical
treatments are used for the treatment of spinal tumors, however,
treatment outcome is dependent on various factors, such as patient
age, overall health of the patient and whether the tumor is benign
or malignant and primary or metastatic (3). The majority of spinal tumors are
metastatic, and are usually treated with palliative therapy,
including radiotherapy, chemotherapy and selective artery embolism.
However, chemotherapy and radiotherapy have extremely limited
effects in the treatment of spine tumors (4). Selective embolization may be used to
control tumor size and reduce bleeding during surgery (5). Approximately 5% of spine tumors are
primary tumors (6) and surgical
treatment can be used to completely cure such tumors in certain
cases. It has also been reported that surgery may be used to
relieve pain in 80–90% of patients with malignant spinal tumors, as
well as improving spinal function in 75% of patients (4).
Spondylectomy for the treatment of spinal neoplasms
was first reported by Stener in 1971 (7) and further used by Roy-Camille et
al (8) and Fidler (9). In the 1990s, Tomita et al
(10) developed and popularized the
surgical procedure known as total en bloc spondylectomy
(TES) to resect the diseased vertebrae. The TES procedure has been
increasingly gaining recognition and is now widely accepted by
spinal tumor surgeons due to its favorable outcomes (11,12).
Generally there are two surgical steps to the TES
procedure (10,13,14): Step
one is a total-laminectomy, which involves the excision of the
posterior of the vertebrae, and step two is the resection of the
total front of the vertebral body. The present study reports 10
cases of total spondylectomy and spine reconstruction through
posterior or combined anterior-posterior approaches for thoracic
lumbar and sacral vertebral tumors.
Patients and methods
Patient data
Between December 2009 and May 2012, 10 cases of
patients with primary malignant tumors of the spine treated by TES
in the Second Affiliated Hospital of Xi'an Jiaotong University
Medical School (Xi'an, China) were retrospectively analyzed
(Table I). The average age of the
patients at the time of surgery was 50.5 years (range, 23–65
years), with an average follow-up time of 50.2 months (range,
28.1–68.7 months). The study group consisted of three females and
seven males.
 | Table I.Data on patients with primary
malignant tumors of the spine. |
Table I.
Data on patients with primary
malignant tumors of the spine.
| Patient no. | Diagnosis | Age, years | Levels | Surgical duration,
h | Intraoperative blood
loss, ml | Status | Follow-up,
months |
|---|
| 1 | Giant cell tumor | 23 | L5-S2 | 11 | 4000 | NED | 24 |
| 2 | Giant cell tumor | 44 | L3–4 | 7 | 3200 | NED | 22 |
| 3 | Malignant fibrous
histiocytoma | 36 | T6 | 5 | 2300 | DOD | 8 |
| 4 | Chordoma | 66 | S3 or below | 3 | 1500 | NED | 28 |
| 5 | Chordoma | 59 | S3 or below | 4 | 1800 | DOC | 18 |
| 6 | Chordoma | 65 | S3 or below | 3 | 1600 | NED | 30 |
| 7 | Plasma cell
myeloma | 59 | T8 | 5 | 2800 | NED | 36 |
| 8 | Plasma cell
myeloma | 62 | T7 | 6 | 2400 | NED | 18 |
| 9 | Giant cell
tumors | 22 | L3 | 8 | 10000 | NED | 33 |
| 10 | Chondrosarcoma | 46 | T7 | 5 | 1800 | NED | 36 |
All 10 cases were of primary tumors, with three
chordomas, three giant cell tumors of the bone, two plasma cell
myelomas, one chondrosarcoma and one malignant fibrous
histiocytoma. Affected segments were T6, T8 and L3 in one case
each, T7 in two cases, L3–4 in one case, L5 and S1–2 in one case
each, and S3 or below in three cases. According to Tomita's grading
system (15), there were four type IV
cases, four type V cases and two type VI cases. Using the Frankel
classification of pre-operative spinal cord function (16), one case was grade A, two cases were
grade C, two cases were grade D and five cases were grade E. Seven
cases required a partial spondylectomy and three required a total
spondylectomy. According to the recorded data for the height,
weight and body mass index of the patients, the average body mass
index was 25.7 kg/m2 (range, 22.2–39.5
kg/m2). Written informed consent was obtained from all
patients and this study was approved by the ethics committee of the
Second Affiliated Hospital of Xi'an Jiaotong University Medical
School.
TES procedure
The TES procedure generally consists of two steps:
Step one is a total-laminectomy, which involves the excision of the
posterior of the vertebrae, and step two is the resection of the
total front of the vertebral body. In step one, the surgical area
is focused on the lesion centrum and the extension for one centrum.
When the transverse of the lesion centrum is fully exposed, the
bilateral pedicle is cut off. The T-saw guide is carefully inserted
into the middle of the lamina and vertebral pedicle surface, and
removed from the neural tube, to completely resect the bilateral
pedicle and avoid nerve root damage. The guide is removed following
the introduction of a special wire saw, which is used to cut off
the vertebral pedicle. To reduce bleeding and contamination by
tumor cells, the cut off vertebral pedicle is wrapped with gauze.
The posterior spine is fixed by temporary equipment to maintain
spinal stability following resection. The bilateral segmental
artery is carefully identified and protected prior to step two. The
thoracic vertebra nerve root is cut off in the intervertebral
foramen. The segmental artery branch along the nerve root is also
cut off. Next, a blunt dissection is performed between the pleura
(or iliopsoas) and the centrum. The aorta is separated from the
anterior centrum using a curette and fingers. The intervertebral
disc is cut carefully using the wire saw. The dura mater is then
separated from the venous plexus and ligaments in the surrounding
spinal canal by nerve dissection. Finally, the anterior and
posterior of the centrum are removed.
Surgical approach
According to the affected segments, the extent of
lesion involvement and the specific pathology results, different
surgical indications and approaches were selected. A one-stage
posterior or combined anterior-posterior total spondylectomy and
reconstruction was used for the treatment of complicated thoracic
lumbar and sacral vertebral malignant and invasive benign tumors.
Titanium mesh autologous bone grafts were used for intervertebral
fusion. The indications for a total spondylectomy were nerve
function defects, an inability to withstand back pain medication
due to spinal instability, or pain that could not be reduced by
injections.
For the affected segments located at the thoracic
level and L3 or above (not including L3 spine), as the tumor did
not invade into the main blood vessels, a one-stage posterior
partial spondylectomy and titanium cage bone graft was used,
together with a posterior screw rod system reconstruction. For S3
or below, a one-stage posterior partial spondylectomy without
reconstruction was used. For L3–5, a one-stage anterior/posterior
partial spondylectomy, spinal canal decompression, a posterior
screw rod system and a titanium cage bone graft reconstruction were
applied. Lastly, for L5-S2, a one-stage anterior/posterior partial
spondylectomy, spinal canal decompression, a posterior screw rod
system and a bilateral autologous fibula reconstruction were
applied.
Data collection
All patients were followed-up on months 1, 3, 6 and
12 post-surgery, and then once a year thereafter. The follow-up
evaluation was performed using medical imageology analysis by spine
specialists who had not been involved in treating the patients. The
frontal and lateral X-rays and computed tomography (CT) were
reviewed prior to or following the surgery. X-ray analysis,
including the measurement of body weight and segmental angle, the
collapsed or displaced vertebral plate grid, and any spinal column
instability or misalignment. CT scan was used to detect the
vertebral plate grid of the graft bone, and at least two or more
sagittal section images were included with adjacent vertebral graft
bone bridge plates.
Results
Surgical and patient data
The average surgical duration was 6.8 h (range,
4.8–12 h) with an average level of blood loss of 3,200 ml (range,
1,500–10,000 ml). All patients were followed-up for an average of
15 months (range, 3–29 mouths). Two patients succumbed and one
patient experienced tumor recurrence at follow-up. One-stage
posterior total spondylectomy for lesions in the thoracic vertebrae
or L3 and above showed thorough removal of the lesional focus and
immediate stability of the spine without fixation, break or evident
complication.
At six months post-operatively, the spinal cord
function for all patients recovered to Frankel classification grade
E. One patient with a lesion in S3 or below showed recurrence, with
urination and defecation function disturbance. One patient with a
L3–5 lesion treated with combined posteroanterior total
spondylectomy showed decreased bilateral quadriceps muscle strength
from level 4 to level 2, complicated by radiating pain in the hip.
However, X-rays and magnetic resonance examination showed thorough
decompression, good spinal stability and no internal fixation
loosening or fracture during the follow-up. One patient with a
L5-S2 lesion showed partial paralysis of the lower limbs, and
spinal cord function decreased from grade D to B. Following one
year of follow-up, bone graft healing without tumor recurrence was
observed, but the posterior screw-rod was broken.
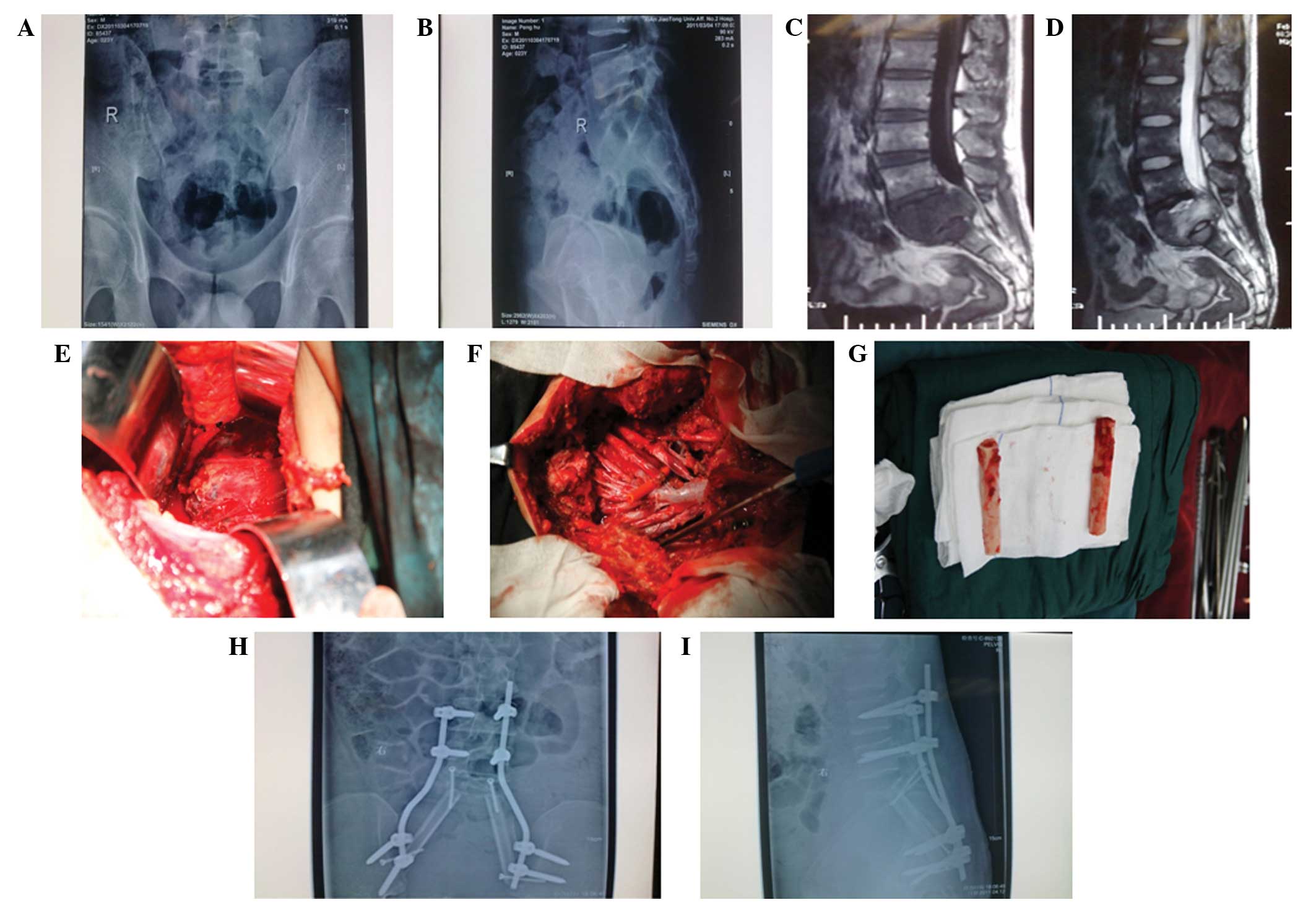
Sample case
One of the patients treated was a 23-year-old male
with a giant cell tumor (case 1 in Table
I). The tumor expanded into the spinal canal and outside of the
vertebral body (Fig. 1). Bilateral
posterior reconstruction with an autologous fibula was used.
Post-operative radiographs and CT scans of the lumbar spine
suggested that the reconstructed spine was well maintained
(Fig. 1).
Discussion
Total spondylectomy is one of the most difficult
surgeries to perform for the treatment of upper thoracic vertebral
tumors with the advantage of the complete removal of tumors
(17). One-stage posterior total
spondylectomy and spine reconstruction can be used to treat primary
malignant tumors in the spine, including chordoma, osteosarcoma and
chondrosarcoma. In addition, benign upper thoracic vertebra tumors
with the potential for invasion or a higher recurrence rate, such
as giant cell tumors, can also be treated by TES (18). Other tumors that lead to nerve
dysfunction and compression fractures, as well as those metastatic
tumors in a single vertebra also require TES. The Second Affiliated
Hospital of Xi'an Jiaotong University Medical School has
successfully treated a number of cases of total spondylectomy with
satisfactory results.
Different techniques for en bloc resection have
previously been described (8–10,19–21). To
achieve a total spondylectomy and reconstruction, a combined
anterior-posterior surgical approach has usually been used.
However, this approach can lead to more serious injury, a longer
surgical duration and greater blood loss, as well as increasing the
psychological and economic burden on the patient. The frontal
thoracotomy approach requires greater patient tolerance and may
lead to the injury of the visceral pleura or large blood vessels
during surgery. The approach has increased risks of atelectasis and
pulmonary infection, as well as an increased risk of respiratory
failure post-operatively for elderly patients with poor lung
function and lung diseases, or in those with pleural adhesion or
who underwent open heart surgery (22).
By contrast, surgery using the posterior approach
could avoid intraoperative injury and the corresponding risk of
complications (23). This approach
does not require a thoracotomy, and is therefore suitable for more
patients as it requires a lower level of tolerance, reduces the
surgical trauma, shortens the surgical duration, lowers the level
of intraoperative blood loss, relieves the patients' pain, reduces
medical costs and shorten the hospital stay. However, the posterior
approach also requires doctors with higher surgical skills, due to
the narrow filed of vision, limited surgical space and easily
damaged spinal cord.
Therefore, we believe that the indications for a
posterior thoracic vertebra total spondylectomy and reconstruction
are as follows: Primary malignant spinal tumors and aggressive
benign tumors; tumors without front internal organ invasion; tumors
without adhesion to the inferior vena cava and aorta; no multiple
metastases; less than 3 vertebral body lesions; and an isolated
vertebral metastatic tumor, without primary lesion, or a primary
tumor lesion under control. The present results showed that
survival time can be extended to between three months and half a
year with the surgery, and the quality of life can be significantly
improved.
Overall, the following conclusions can be made from
this study: Firstly, if the lesion location is above L3 without
main venous invasion, the posterior approach only gives a better
result. Secondly, to treat tumors with main venous invasion or
serious segmental blood vessel adhesion, the anterior approach
should be used first, followed by a posterior total spondylectomy
and reconstruction. Lastly, for those lesions located at L3-S2,
where the surgical field may be covered by the ala ossis ilii, and
affected by the existence of abdominal aortic bifurcation and psoas
major, the use of a combined anterior and posterior approach would
result in a better prognosis.
References
|
1
|
Dahlin DC: Bone Tumors; General Aspects
and Data on 3,987 cases (2nd). Springfield, IL: C. C. Thomas.
2851967.
|
|
2
|
Van Goethem JW, van den Hauwe L, Ozsarlak
O, De Schepper AM and Parizel PM: Spinal tumors. Eur J Radiol.
50:159–176. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bilsky MH, Lis E, Raizer J, Lee H and
Boland P: The diagnosis and treatment of metastatic spinal tumor.
Oncologist. 4:459–469. 1999.PubMed/NCBI
|
|
4
|
Frymoyer JW and Wiesel SW: The Adult and
Pediatric Spine (3rd). Philadelphia, PA: Lippincott Williams &
Wilkins. 2004.
|
|
5
|
Simmons ED and Zheng Y: Vertebral tumors:
Surgical versus nonsurgical treatment. Clin Orthop Relat Res.
443:233–247. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Munoz-Bendix C, Slotty PJ, Ahmadi SA,
Bostelmann R, Steiger HJ and Cornelius JF: Primary bone tumors of
the spine revisited: A 10-year single-center experience of the
management and outcome in a neurosurgical department. J
Craniovertebr Junction Spine. 6:21–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Stener B: Total spondylectomy in
chondrosarcoma arising from the seventh thoracic vertebra. J Bone
Joint Surg Br. 53:288–295. 1971.PubMed/NCBI
|
|
8
|
Roy-Camille R, Saillant G, Mazel CH and
Monpierre H: Total vertebrectomy as treatment of malignant tumors
of the spine. La Chir Organi Mov. 75(1 Suppl): 94–96.
1990.PubMed/NCBI
|
|
9
|
Fidler MW: Radical resection of vertebral
body tumours. A surgical technique used in ten cases. J Bone Joint
Surg Br. 76:765–772. 1994.PubMed/NCBI
|
|
10
|
Tomita K, Kawahara N, Baba H, Tsuchiya H,
Fujita T and Toribatake Y: Total en bloc spondylectomy. A new
surgical technique for primary malignant vertebral tumors. Spine
(Phila Pa 1976). 22:324–333. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kato S, Murakami H, Demura S, et al: More
than 10-year follow-up after total en bloc spondylectomy for spinal
tumors. Ann Surg Oncol. 21:1330–1336. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tomita K, Kawahara N, Murakami H and
Demura S: Total en bloc spondylectomy for spinal tumors:
improvement of the technique and its associated basic background. J
Orthop Sci. 11:3–12. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kawahara N, Tomita K, Murakami H, Demura
S, Yoshioka K and Kato S: Total en bloc spondylectomy of the lower
lumbar spine: a surgical techniques of combined posterior-anterior
approach. Spine (Phila Pa 1976). 36:74–82. 2011.PubMed/NCBI
|
|
14
|
Demura S, Kawahara N, Murakami H, et al:
Total en bloc spondylectomy for spinal metastases in thyroid
carcinoma. J Neurosurg Spine. 14:172–176. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tomita K, Kawahara N, Kobayashi T, et al:
Surgical strategy for spinal metastases. Spine (Phila Pa 1976).
26:298–306. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ditunno JF Jr, Young W, Donovan WH and
Creasey G: The international standards booklet for neurological and
functional classification of spinal cord injury. American Spinal
Injury Association. Paraplegia. 32:70–80. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Guo C, Yan Z, Zhang J, et al: Modified
total en bloc spondylectomy in thoracic vertebra tumour. Eur Spine
J. 20:655–660. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chung JY, Kim SK, Jung ST and Lee KB: New
posterior column reconstruction using titanium lamina mesh after
total en bloc spondylectomy of spinal tumour. Int Orthop.
37:469–476. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Boriani S, Biagini R, De Iure F, et al: En
bloc resections of bone tumors of the thoracolumbar spine. A
preliminary report on 29 patients. Spine (Phila Pa 1976).
21:1927–1931. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Krepler P, Windhager R, Bretschneider W,
Toma CD and Kotz R: Total vertebrectomy for primary malignant
tumours of the spine. J Bone Joint Surg Br. 84:712–715. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mazel C, Grunenwald D, Laudrin P and
Marmorat JL: Radical excision in the management of thoracic and
cervicothoracic tumors involving the spine: results in a series of
36 cases. Spine (Phila Pa 1976). 28:782–792. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yang Q, Li JM, Yang ZP, Li X, Li ZF and
Yan J: Treatment of thoracolumbar tumors with total en bloc
spondylectomy and the results of spinal stability reconstruction.
Zhonghua Zhong Liu Za Zhi. 35:225–230. 2013.(In Chinese).
PubMed/NCBI
|
|
23
|
Matsumoto M, Tsuji T, Iwanami A, et al:
Total en bloc spondylectomy for spinal metastasis of differentiated
thyroid cancers: a long-term follow-up. J Spinal Disord Tech.
26:E137–E142. 2013. View Article : Google Scholar : PubMed/NCBI
|