Introduction
Mesothelioma is a rare type of cancer originating
from the surface linings of serous cavities; these membranes
include the pleura, peritoneum and pericardium (1,2). Malignant
peritoneal mesothelioma (MPM) is highly aggressive, accounting for
~25% of all mesothelioma cases (3),
and is the second most common mesothelioma subtype after pleural
mesothelioma. Mesothelioma exhibits a predilection for males with a
history of work-related asbestos exposure (2).
The four main cellular subtypes of mesothelioma are
epithelioid, sarcomatoid, biphasic and desmoplastic (4,5). Of these
subtypes, epithelioid mesothelioma is the most common. Cells of
epithelioid mesothelioma tumors are usually epithelial-like and may
be cuboidal, tubular or flattened. In rare cases, tumors may
exhibit deciduoid, pleomorphic, signet-ring or clear cell features
(6). Clear cell-type mesothelioma is
extremely rare, with only a few individual case reports published
previously (1,6–8). In the
present study, a rare case of clear cell MPM is reported in a
60-year-old female with no history of asbestos exposure.
Case report
On August 21, 2012, a 60-year-old female was
admitted to The First Hospital of Jilin University (Changchun,
China) with intestinal fistula, incisional hernia and abdominal
infection. The patient had undergone a cesarean section and
appendectomy 30 years previously, and the resultant abdominal
incision had healed well. In August 2008, the patient presented to
a local hospital (Central Hospital of Siping, Siping, China) with
an incisional hernia located at the cesarean section incision.
Incisional hernia repair surgery was subsequently performed, and
the section of the small bowel in the incisional sac was returned
to the abdominal cavity. In April 2011, the patient presented again
with an incisional hernia with a protruded abdominal mass. During a
laparotomy, a massive cystic cavity with purulence outside of the
peritoneum in the lower abdomen was found. The purulent cyst was
removed, the patient's general condition improved and the abdominal
mass disappeared.
In August 2012, the patient was admitted to a local
hospital for the third time due to the recurrence of the incisional
hernia with an abdominal mass, which exuded yellowish fluid. A
secondary laparotomy was performed with the same findings as in
2011. Following aspiration of the purulent fluid, a drainage tube
was inserted into the incisional hernia lesion. At 3 days
post-surgery, fecal-like materials passed through the drainage
tube, and the patient was transferred to The First Hospital of
Jilin University for further management. The patient had no history
of smoking or alcohol consumption, and no history of asbestos
exposure.
A physical examination revealed abdominal distension
with ascites, but no abdominal pain, stiffness or rebound
tenderness. Laboratory blood examinations revealed a marginal
increase in platelet number (381×109 cells/l; normal
range, 100–300×109 cells/l). Red and white blood cell
count and liver and kidney functions were normal. Chest and plain
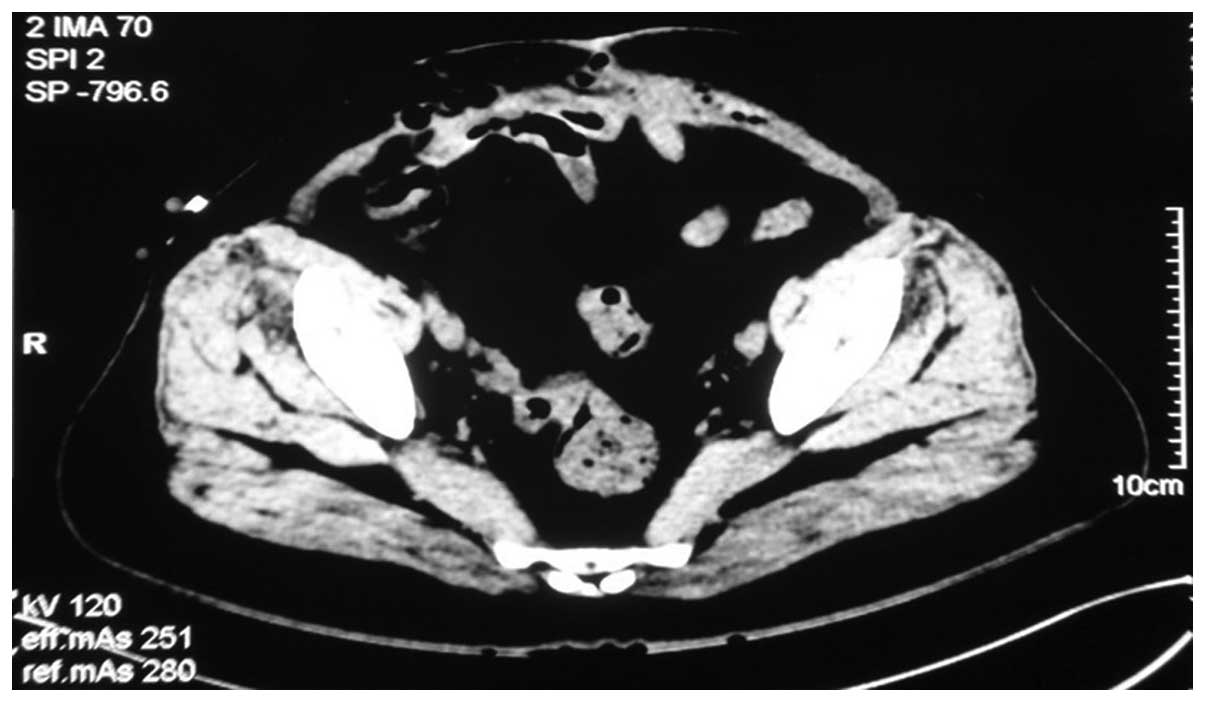
abdominal radiographs were normal. Extensive small bowel adhesion
and massive peritoneal effusion were observed on the abdominal
computed tomography scans (Fig. 1).
The patient was admitted for further management of the intestinal
fistula, incisional hernia and abdominal infection.
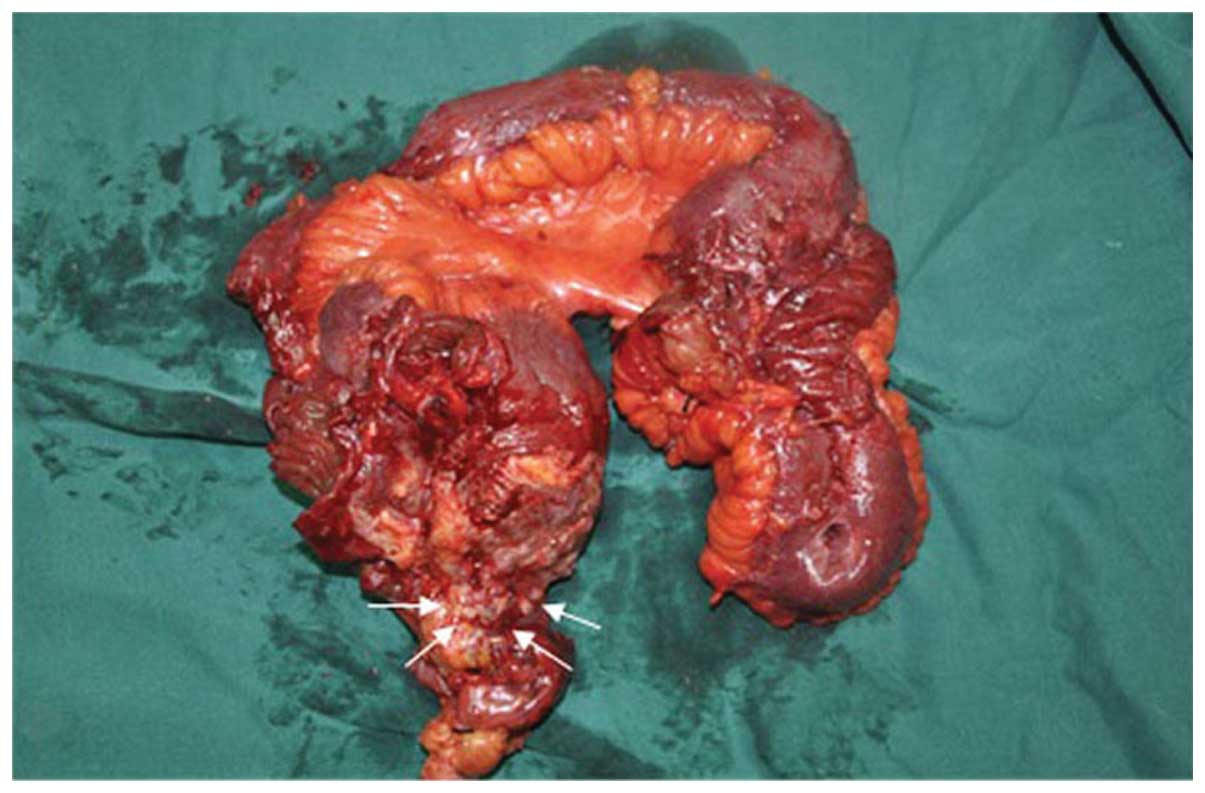
A laparotomy was performed on August 27, 2012. A
massive purulent cavity (15×12×3 cm) was identified outside the
peritoneum in the lower abdomen. Multiple white nodules of variable
size (1–5 mm) were found in the peritoneum. Extensive bowel
adhesions were also observed. No significant enlargement of the
lymph nodes was identified, and no lesions were found in the liver,
pancreas, spleen, kidneys or ovaries. The adhesive bowels were
separated. An intestinal fistula was identified ~80 cm from the
distal end of the jejunum suspensory ligament, closely connected to
the cranial end of the purulent cavity. The necrotic intestinal
fistula was resected and multiple white tumor-like nodules were
observed on the surface (Fig. 2).
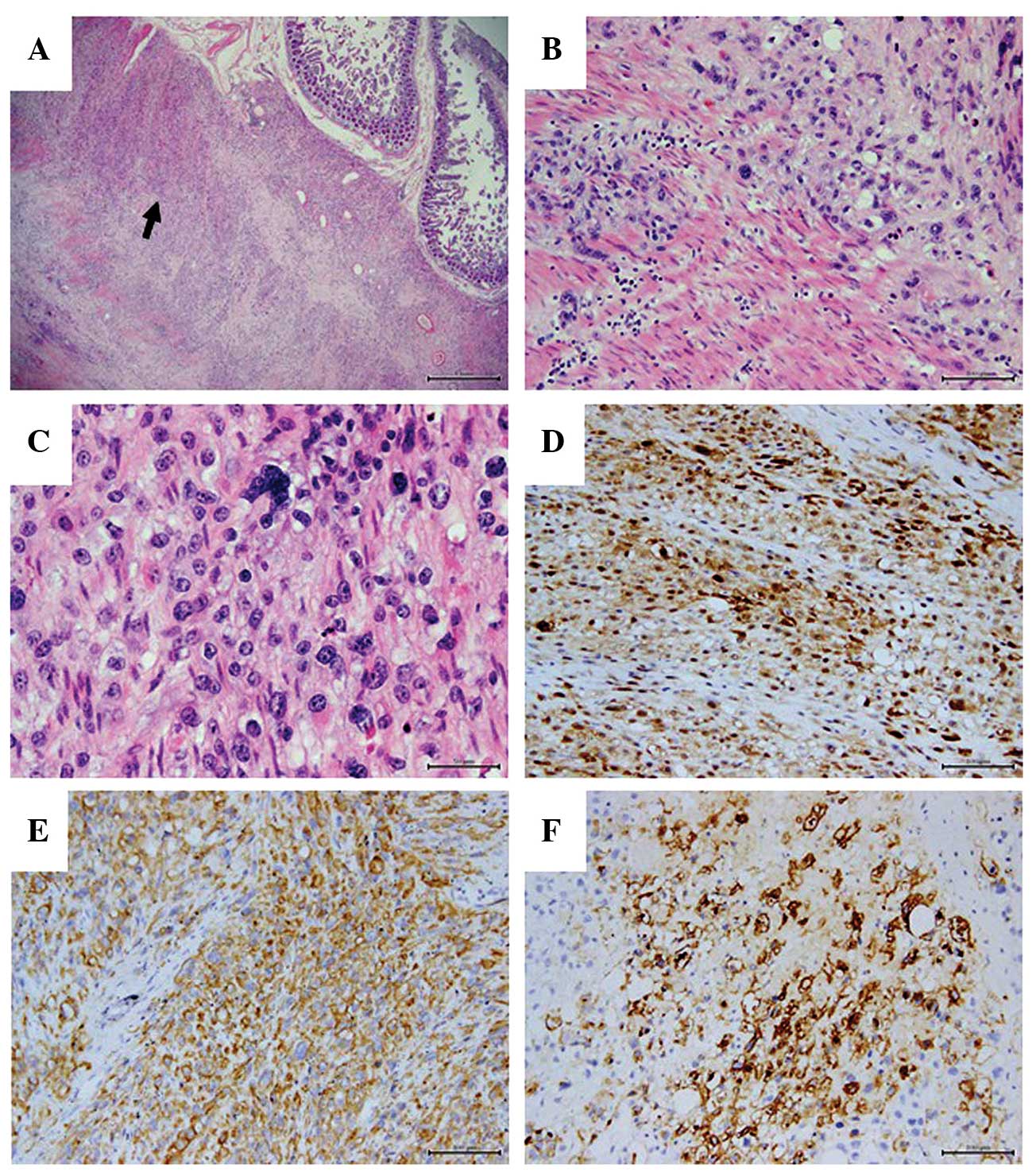
Histological examination of the intestinal fistula
biopsy specimens indicated the presence of MPM, with invasion to
the intestinal submucosa and mesenterium (Fig. 3). Positive immunoreactivity was
observed for calretinin (Fig. 3D),
pan-cytokeratin (Fig. 3E),
cytokeratin 7, cytokeratin 14, cytokeratin 19, epithelial membrane
antigen (EMA; Fig. 3F), cluster of
differentiation (CD)99, caldesmon and Ki-67. Negative expression of
calponin, S-100, vimentin, CD34, HMB-45, smooth muscle actin,
desmin, CD117 and DOG1 proteins was also observed. A fistula of the
anastomotic lesion occurred 1 week post-operatively. Local flushing
and dressing of the lesions was performed. No further medical
treatment was administered. Follow-up examination 1 year after
surgery revealed that the patient was in generally good health, and
at the time of writing, the patient remained alive with no signs of
recurrence.
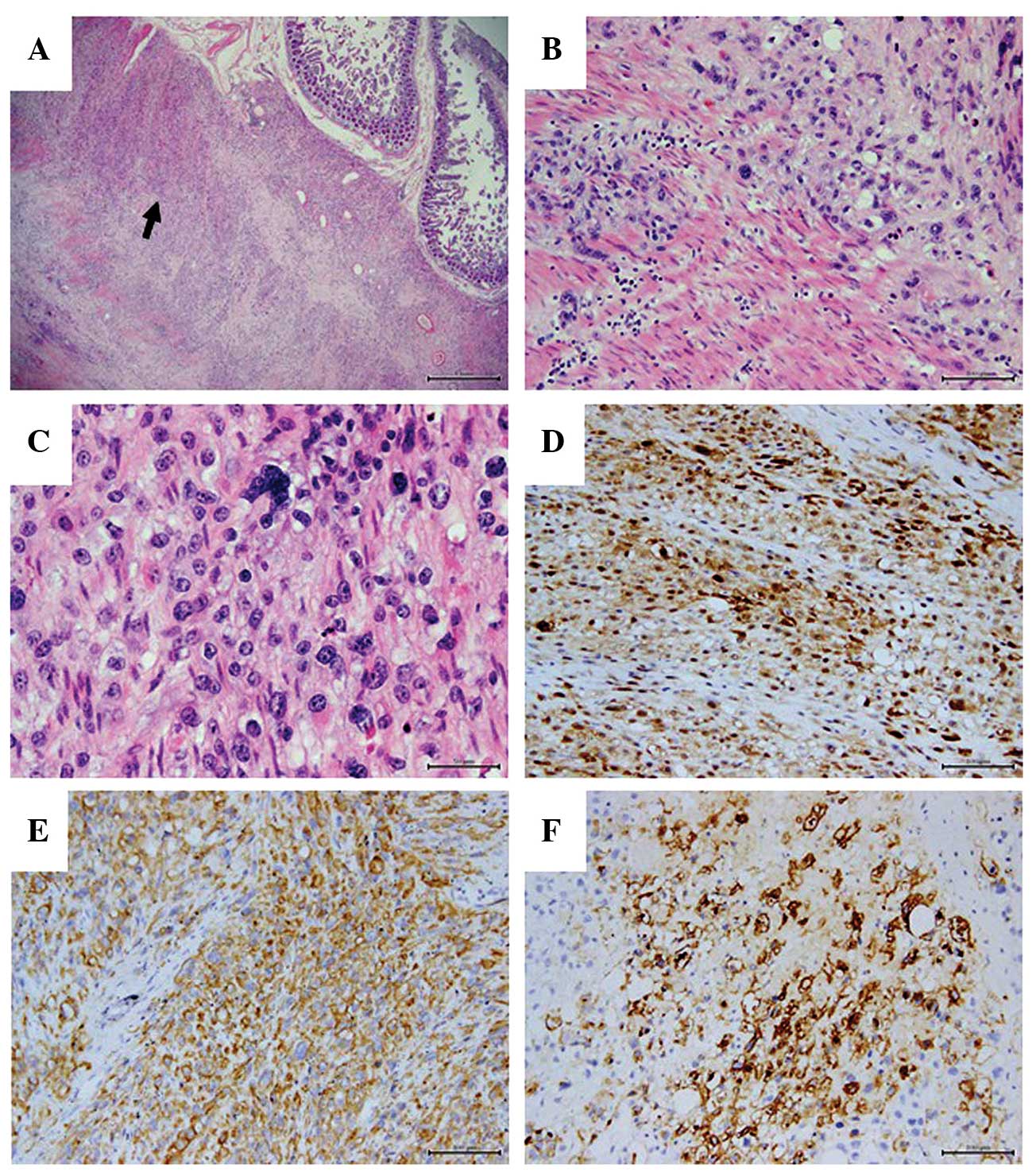 | Figure 3.Histopathological and immunoreactive
features of malignant peritoneal mesothelioma. (A) Mesothelioma
with epithelial-like cells (indicated by the black arrow) and
intestinal mucosa (stain, H&E; scale bar, 1 mm). (B) Micrograph
of mesothelioma with epithelial-like cells and clear cells (stain,
H&E; scale bar, 100 µm). (C) Clear cells with prominent nuclei
and clear cytoplasm in tumor cells (stain, H&E; scale bar, 50
µm). (D) Diffuse positive immunoreactivity for calretinin in nuclei
and cytoplasm (scale, 100 µm). (E) The majority of the tumor was
pan-cytokeratin-positive (scale bar, 100 µm). (F) The majority of
cellular membranes were epithelial membrane antigen-positive (scale
bar, 100 µm). H&E, hematoxylin and eosin. |
Discussion
MPM is a rare disease with varied and non-specific
clinical presentations, and thus its diagnosis is often overlooked
by surgeons and pathologists (2). The
patient in the present report underwent three laparotomies as a
result of incisional hernia and abdominal infection. However, only
after the last pathological analysis was the presence of MPM
diagnosed. Increased awareness and caution with regard to this
disease is therefore required.
A history of asbestos exposure is closely associated
with the susceptibility to MPM (9).
The incidence of MPM is higher in males than females, which may be
related to their higher risk of occupational exposure to asbestos
(10). The proportion of patients
with mesothelioma reporting histories of asbestos exposure ranged
from 5–83% (9). However, the absence
of a history of asbestos exposure does not exclude the possibility
of malignant mesothelioma. Other risk factors of peritoneal
mesothelioma include recurrent peritonitis (11), radiation therapy (12), mica exposure (13), and thorium dioxide administration for
cholangiography (14). Notably, the
patient in the present report had no history of asbestos
exposure.
Clinical presentations of MPM are non-specific.
Abdominal distention and the identification of an abdominal mass
are the most common primary presentations (1). Approximately 70% of patients exhibit
serous ascetic fluid, which is produced by tumor nodules (3). Thrombocytosis is another common symptom
observed in MPM patients (15),
occurring in 40–80% of cases (9,16). In the
present case, routine blood tests revealed a marginal increase in
platelet count (381×109 cells/l), which may have been
due to the presence of tumor cells. However, the exact pathogenesis
of thrombocytosis remains to be elucidated.
The most specific manifestation of MPM identified
during laparoscopy or laparotomy is the presence of diffuse whitish
tumor nodules on the peritoneum (2,3).
Aggregation of these nodules to form masses or plaques may occur.
The MPM patient in the current report presented with an intestinal
fistula, incisional hernia and abdominal infection, which to the
best of our knowledge, has not been reported previously in the
literature. However, the coexistence of inguinal and umbilical
hernia and MPM is more common (4,9,17,18).
Munkholm-Larsen et al (3)
reported that 13% of MPM patients exhibit a newly developed
abdominal wall hernia. The development of a hernia in MPM patients
may be due to the accumulation of intra-abdominal pressure from
ascites. However, the presence of MPM in the hernial sac may be the
result of chronic inflammation (9).
Recurrent or chronic infection as a main presentation of the
disease is not that common in MPM patients, although certain
patients may exhibit symptoms of inflammatory bowel disease
(19,20). Peritoneal mesothelioma complicated
with a fistula is rare, with only a few cases reported previously;
Govender et al reported the occurrence of a colojejunal
fistula and a long sigmoid stricture in a 53-year-old male with
peritoneal mesothelioma (21), and
McCaffrey et al (22) reported
an unusual case of benign peritoneal mesothelioma in a 59-year-old
female with colovesical fistula and bilateral hydronephrosis
formation. We hypothesize that the occurrence of fistulae may be
due to tissue necrosis, chronic stimulation of local inflammation
and a lack of blood supply to the intestinal tract.
The diagnosis of MPM is difficult to establish
pre-operatively. Usually, the diagnosis is based on pathological
hematoxylin-eosin staining and immunohistochemical staining from
biopsy samples collected during laparoscopy and laparotomy
(3). Due to the high prevalence of
ascites in MPM patients, the cytological examination of ascetic
fluid is often required. However, the results of ascites cytology
are often non-specific (23).
Cytological examination was not performed in the present study.
Microscopic examination of the intestinal fistula biopsy specimen
revealed the presence of undifferentiated malignant neoplastic
nodules with infiltration of the intestinal submucosa and
mesenterium (Fig. 3A). These
epithelial-like cells were diverse in size and shape, with a number
of clear cells exhibiting prominent nuclei and clear cytoplasm
(Fig. 3B and C). Malignant
mesothelioma commonly exhibit positive immunoreactivity for
calretinin, EMA, Wilms' tumor 1 antigen, serum mesothelin-related
protein, podoplanin, cytokeratin (CK)5/6, D2-40 antibodies, CA12-5,
CA15-3, hyaluronic acid, osteopontin and pan-CK, and exhibit
negative immunoreactivity for calponin, S-100, vimentin, HMB-45,
CD117, DOG1, Ber-EP4, MOC-31, TAG72, CA19-9, CD15, monoclonal
carcinoembryonic antigen and BG-8 antibodies (24).
The differential diagnosis of MPM is quite broad,
and also depends on histological analyses (25). The main diagnostic difficulty is
differentiating MPM from adenocarcinoma (2). Among the aforementioned markers,
calretinin, a vitamin D-dependent calcium-binding protein, is the
most definitive in differentiating mesothelioma from adenocarcinoma
(26); calretinin is largely present
in mesothelioma, but absent in adenocarcinoma. Renal cell carcinoma
may also complicate the diagnosis of MPM; calretinin and
cytokeratin are positively expressed in epithelioid mesothelioma,
but not in renal cell carcinoma (8).
Strong EMA expression and negative desmin expression also indicate
malignant mesothelioma, and may be used as reliable markers to
distinguish malignant mesothelioma from benign reactive mesothelial
proliferation (2,25,27). The
positive immunostaining of cytokeratin also aids to distinguish
malignant mesothelioma from melanoma and sarcoma, and also confirms
tumor invasion (1). In the present
case, the macroscopic observations during laparotomy, the
microscopic morphologies, and the positive immunoreactivity of
several markers indicated the diagnosis of MPM.
At present, no optimal treatment strategy for MPM
has been established. Due to the rarity of this tumor, few previous
studies have investigated possible treatment regimens. Eltabbakh
et al (28) demonstrated that
cytoreduction surgery combined with chemotherapy (paclitaxel and
cisplatin) may provide a benefit for female patients. Sugarbaker
et al (29) also confirmed
that a combined regimen of cytoreduction surgery and
intraperitoneal chemotherapy prolonged survival and completely
resolved ascetic fluid in the majority of patients. However, the
distribution of tumor nodules is not limited to the peritoneal
surface, and may also extend to the small bowel and mesentery,
which complicates cytoreduction surgery, preventing completion of
the procedure in certain cases.
The prognosis of patients with MPM is relatively
poor, with a reported survival time of ~1 year following the
diagnosis (2,28). In one study, the median survival time
of diffuse MPM patients improved to 92 months, with a 5-year
survival rate of 59%, following combined treatment with
cytoreductive surgery and intraperitoneal chemotherapy (30). However, the patient in the present
case refused all chemotherapy. Despite this, the patient survived,
was in generally good health at the follow-up examination performed
at 1 year post-surgery and remains alive at the time of writing
this study.
MPM is a rare disease, and thus information
regarding this type of cancer remains limited. The present case
study highlights that a diagnosis of MPM should be considered in
patients with intractable intestinal fistula, incisional hernia and
abdominal infection. Stimulation due to recurrent inflammation may
facilitate tumor progression and compromise the healing of an
incisional hernia. Furthermore, presentations of incisional hernia
with intestinal fistula accompanied by peritoneal infection may
obscure recognition of malignant mesothelioma, and make an accurate
diagnosis of MPM difficult.
References
|
1
|
Dessy E, Falleni M, Braidotti P, Del Curto
B, Panigalli T and Pietra GG: Unusual clear cell variant of
epithelioid mesothelioma. Arch Pathol Lab Med. 125:1588–1590.
2001.PubMed/NCBI
|
|
2
|
Robinson BW and Lake RA: Advances in
malignant mesothelioma. N Engl J Med. 353:1591–1603. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Munkholm-Larsen S, Cao CQ and Yan TD:
Malignant peritoneal mesothelioma. World J Gastrointest Surg.
1:38–48. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
D'Ambrosio V: Mesothelioma as primary
tumor of the peritoneum. A case report. J Med Soc N J. 70:637–639.
1973.PubMed/NCBI
|
|
5
|
Hammar SP: Macroscopic, histologic,
histochemical, immunohistochemical, and ultrastructural features of
mesothelioma. Ultrastruct Pathol. 30:3–17. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gkogkou C, Samitas K and Foteinou M:
Primary pleural epithelioid mesothelioma of clear cell type: A case
report and review of current literature. Ultrastruct Pathol.
35:267–270. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ordóñez NG: Mesothelioma with clear cell
features: An ultrastructural and immunohistochemical study of 20
cases. Hum Pathol. 36:465–473. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ordóñez NG: Clear cell mesothelioma
presenting as an incarcerated abdominal hernia. Virchows Arch.
447:823–827. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
de Pangher Manzini V: Malignant peritoneal
mesothelioma. Tumori. 91:1–5. 2005.PubMed/NCBI
|
|
10
|
Sugarbaker PH, Welch LS, Mohamed F and
Glehen O: A review of peritoneal mesothelioma at the washington
cancer institute. Surg Oncol Clin N Am. 12:605–621. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Riddell RH, Goodman MJ and Moossa AR:
Peritoneal malignant mesothelioma in a patient with recurrent
peritonitis. Cancer. 48:134–139. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Antman KH, Corson JM, Li FP, Greenberger
J, Sytkowski A, Henson DE and Weinstein L: Malignant mesothelioma
following radiation exposure. J Clin Oncol. 1:695–700.
1983.PubMed/NCBI
|
|
13
|
Chahinian AP, Pajak TF, Holland JF, Norton
L, Ambinder RM and Mandel EM: Diffuse malignant mesothelioma.
Prospective evaluation of 69 patients. Ann Intern Med. 96:746–755.
1982. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Maurer R and Egloff B: Malignant
peritoneal mesothelioma after cholangiography with thorotrast.
Cancer. 36:1381–1385. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
De Pangher Manzini V, Brollo A and Bianchi
C: Thrombocytosis in malignant pleural mesothelioma. Tumori.
76:576–578. 1990.PubMed/NCBI
|
|
16
|
Piccigallo E, Jeffers LJ, Reddy KR,
Caldironi MW, Parenti A and Schiff ER: Malignant peritoneal
mesothelioma. A clinical and laparoscopic study of ten cases. Dig
Dis Sci. 33:633–639. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mirabella F: Peritoneal mesothelioma and
abdominal hernias. Minerva Med. 87:21–24. 1996.(In Italian).
PubMed/NCBI
|
|
18
|
Smith TR: Malignant peritoneal
mesothelioma: Marked variability of CT findings. Abdom Imaging.
19:27–29. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Higashihara M, Sunaga S, Tange T, Oohashi
H and Kurokawa K: Increased secretion of interleukin-6 in malignant
mesothelioma cells from a patient with marked thrombocytosis.
Cancer. 70:2105–2108. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Melero M, Lloveras J, Waisman H, Elsner B
and Baldessari E: Malignant peritoneal mesothelioma. An infrequent
cause of prolonged fever syndrome and leucocytosis in a young
adult. Medicina (B Aires). 55:48–50. 1995.(In Spanish). PubMed/NCBI
|
|
21
|
Govender SS, Seebaran AR, Moodley V and
Rajput MC: Peritoneal mesothelioma complicated by colojejunal
fistula. A case report. S Afr J Surg. 25:103–105. 1987.PubMed/NCBI
|
|
22
|
McCaffrey JC, Foo FJ, Dalal N and Siddiqui
KH: Benign multicystic peritoneal mesothelioma associated with
hydronephrosis and colovesical fistula formation: Report of a case.
Tumori. 95:808–810. 2009.PubMed/NCBI
|
|
23
|
Yu GH, Soma L, Hahn S and Friedberg JS:
Changing clinical course of patients with malignant mesothelioma:
Implications for FNA cytology and utility of immunocytochemical
staining. Diagn Cytopathol. 24:322–327. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ahmed I, Ahmed Tipu S and Ishtiaq S:
Malignant mesothelioma. Pak J Med Sci. 29:1433–1438. 2013.(Review).
PubMed/NCBI
|
|
25
|
Baker PM, Clement PB and Young RH:
Malignant peritoneal mesothelioma in women: A study of 75 cases
with emphasis on their morphologic spectrum and differential
diagnosis. Am J Clin Pathol. 123:724–737. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chhieng DC, Yee H, Schaefer D, Cangiarella
JF, Jagirdar J, Chiriboga LA, Jagirdar J, Chiriboga LA and Cohen
JM: Calretinin staining pattern aids in the differentiation of
mesothelioma from adenocarcinoma in serous effusions. Cancer.
90:194–200. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Saad RS, Cho P, Liu YL and Silverman JF:
The value of epithelial membrane antigen expression in separating
benign mesothelial proliferation from malignant mesothelioma: A
comparative study. Diagn Cytopathol. 32:156–159. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Eltabbakh GH, Piver MS, Hempling RE, Recio
FO and Intengen ME: Clinical picture, response to therapy, and
survival of women with diffuse malignant peritoneal mesothelioma. J
Surg Oncol. 70:6–12. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sugarbaker PH, Yan TD, Stuart OA and Yoo
D: Comprehensive management of diffuse malignant peritoneal
mesothelioma. Eur J Surg Oncol. 32:686–691. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Feldman AL, Libutti SK, Pingpank JF,
Bartlett DL, Beresnev TH, Mavroukakis SM, Steinberg SM, Liewehr DJ,
Kleiner DE and Alexander HR: Analysis of factors associated with
outcome in patients with malignant peritoneal mesothelioma
undergoing surgical debulking and intraperitoneal chemotherapy. J
Clin Oncol. 21:4560–4567. 2003. View Article : Google Scholar : PubMed/NCBI
|