Introduction
Colorectal cancer is the fourth most frequently
diagnosed cancer in the USA (1).
Primary colonic lymphoma is rare, accounting for 0.16–0.60% of all
primary colorectal cancers and 10–20% of all gastrointestinal
lymphomas (2). The most frequent
location of colonic lymphoma at diagnosis is the ileocecal region
(2–4).
Follicular lymphoma (FL) is the most common subtype of indolent
non-Hodgkin's lymphoma (NHL) and the second most common type of
gastrointestinal lymphoma (5).
Collision colorectal adenocarcinoma and lymphoma are extremely rare
and only a few cases have been reported in the literature (6–12).
Lymphoma is frequently characterized by chromosomal translocations
and certain genetic aberrations, and its growth and development
into a malignant neoplasm is dependent on its ability to escape
natural host defenses (13).
Chemotherapy may cause the patient to develop an immunocompromised
status (13), and immunosuppression
is known to play a role in the pathogenesis of lymphoma and
therefore may be involved in the pathogenesis of collision tumor
(14,15). The present study reports the case of a
patient with a collision tumor of primary follicular lymphoma and
adenocarcinoma, located in the cecum. Following adjuvant treatment
of colon carcinoma, the low grade lymphoma demonstrated an
unexpected aggressive course. Therefore, it is possible that
receiving chemotherapy for the treatment of one type of tumor may
trigger the progression of the other type of cancer in collision
tumors.
Case report
A 73-year-old male was referred to Gaziantep
University Hospital (Gaziantep, Turkey) in August 2013 with a
history of muscle weakness, fatigue, weight loss and colic
abdominal pain for the previous 2 months. A physical examination
revealed that the right side of the lower abdomen of the patient
was painful, but there was no lymphomegaly or hepatosplenomegaly.
Laboratory tests demonstrated that the patient possessed a
hemoglobin level of 9.9 g/dl (normal range, 11.2–15.7 g/dl), white
blood cell count of 12,300 cells/µl [normal range, 3,980-10,040;
neutrophils, 85% (normal range, 34–71%); lymphocytes, 9.0% (normal
range, 19.3–51.7%); monocytes, 4.1% (normal range, 4.4–12.5%)],
platelet count of 356,000 cells/µl (normal range, 182,000–369,000
cells/µl), lactate dehydrogenase (LDH) level of 255 units/l (normal
range, 125–247 units/l), erythrocyte sedimentation rate (ESR) of 55
mm/h (normal range, 1–20 mm/h) and carcinoembryonal antigen (CEA)
level of 2.8 ng/ml (normal range, 0–3.0 ng/ml). Abdominal computed
tomography revealed the presence of a 8-cm mass located in the
cecum of the patient. A preliminary diagnosis of an abscess was
made, however when the patient underwent a laparotomy, the mass was
observed to be tumorous. A right hemicolectomy with lymph node,
adjacent omentum and intestine dissection and an appendectomy was
performed. An ulcerovegetant mass ~4 cm in diameter at the
ileocecal valve was detected. Macroscopically, the tumor appeared
to exceed the serosa and extend to the appendix. The pathology
results provided a diagnosis of adenocarcinoma and grade 1 FL in
the cecum, with metastasis to 1 out of 6 regional lymph nodes.
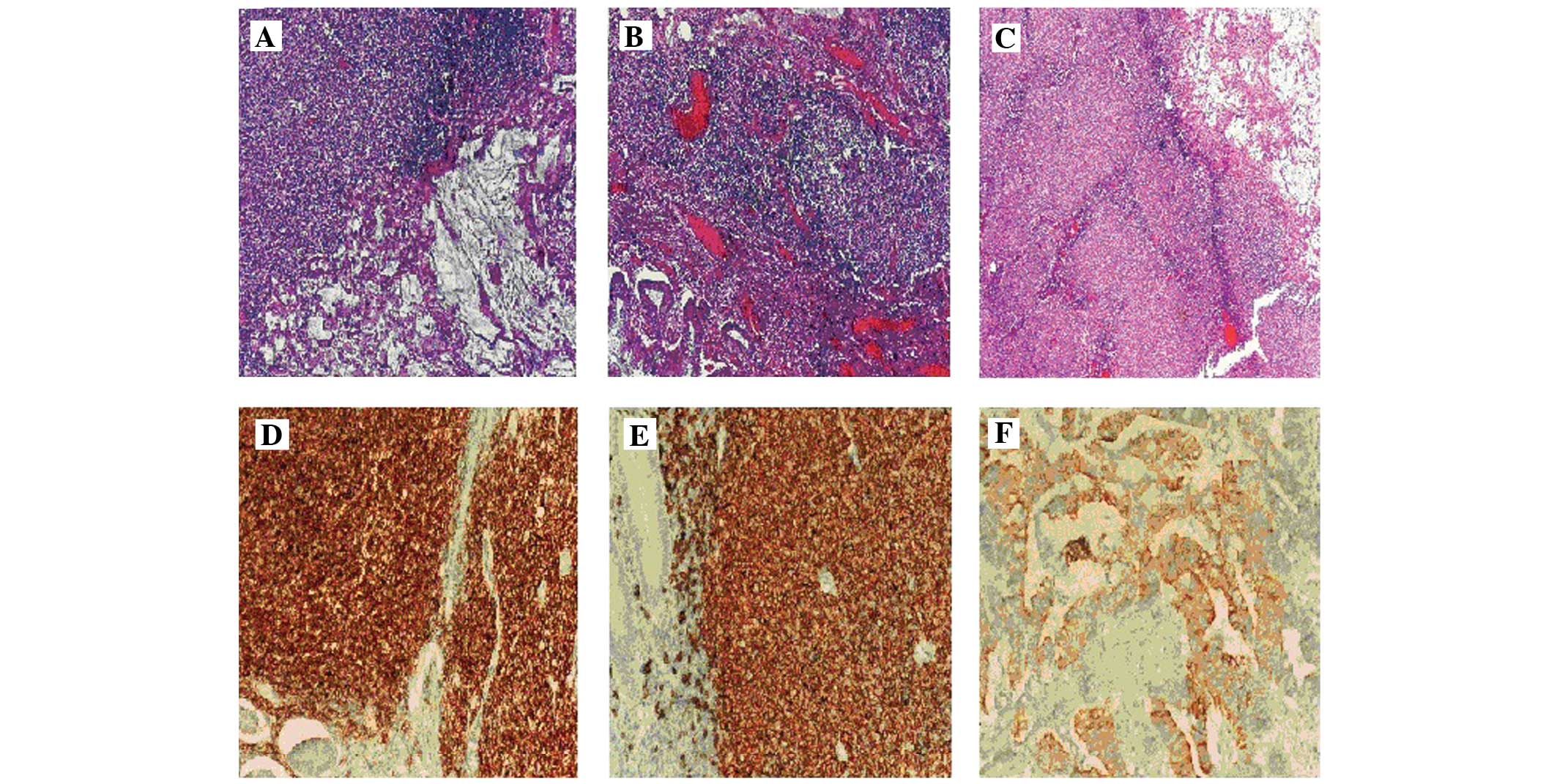
Immunohistochemical analysis, using a light microscope (E600; Nikon
Corporation, Tokyo, Japan) supported this diagnosis (Fig. 1), as the adenocarcinoma tissue
expressed pancytokeratin (detected by mouse anti-human monoclonal
cytokeratin cocktail antibody; cat. no. 313M-18; ready to use;
Sigma-Aldrich, St. Louis, MO, USA), and the FL tissue expressed
cluster of differentiation (CD)-20 (detected by rabbit anti-human
monoclonal CD20 antibody; cat. no. 120R-18; ready to use;
Sigma-Aldrich), B-cell lymphoma-2 (Bcl-2; detected by rabbit
anti-human monoclonal Bcl-2 antibody; cat. no. 226R-28; ready to
use; Sigma-Aldrich) and CD10 (detected by mouse anti-human
monoclonal CD10 antibody; cat. no. 110M-18; ready to use;
Sigma-Aldrich), but did not express CD3 (detected by rabbit
anti-human monoclonal CD3 antibody; cat. no. MRQ-39; ready to use;
Sigma-Aldrich), CD5 (detected by rabbit anti-human monoclonal CD5
antibody; cat. no. 205R-18; ready to use; Sigma-Aldrich), cyclin D1
(detected by rabbit anti-human monoclonal cyclin D1 antibody; cat.
no. 241R-18; ready to use; Sigma-Aldrich) and CD23 (detected by
rabbit anti-human monoclonal CD23 antibody; cat. no. 123R-18; ready
to use; Sigma-Aldrich). Sections were stained using the ultraView
Universal DAB Detection kit (Ventana Medical Systems, Inc., Tucson,
AZ, USA) in an automated slide processing system (BenchMark ULTRA;
Ventana Medical Systems, Inc.). The colon carcinoma was staged as
T3N1M0 according to the American Joint Committee on Cancer
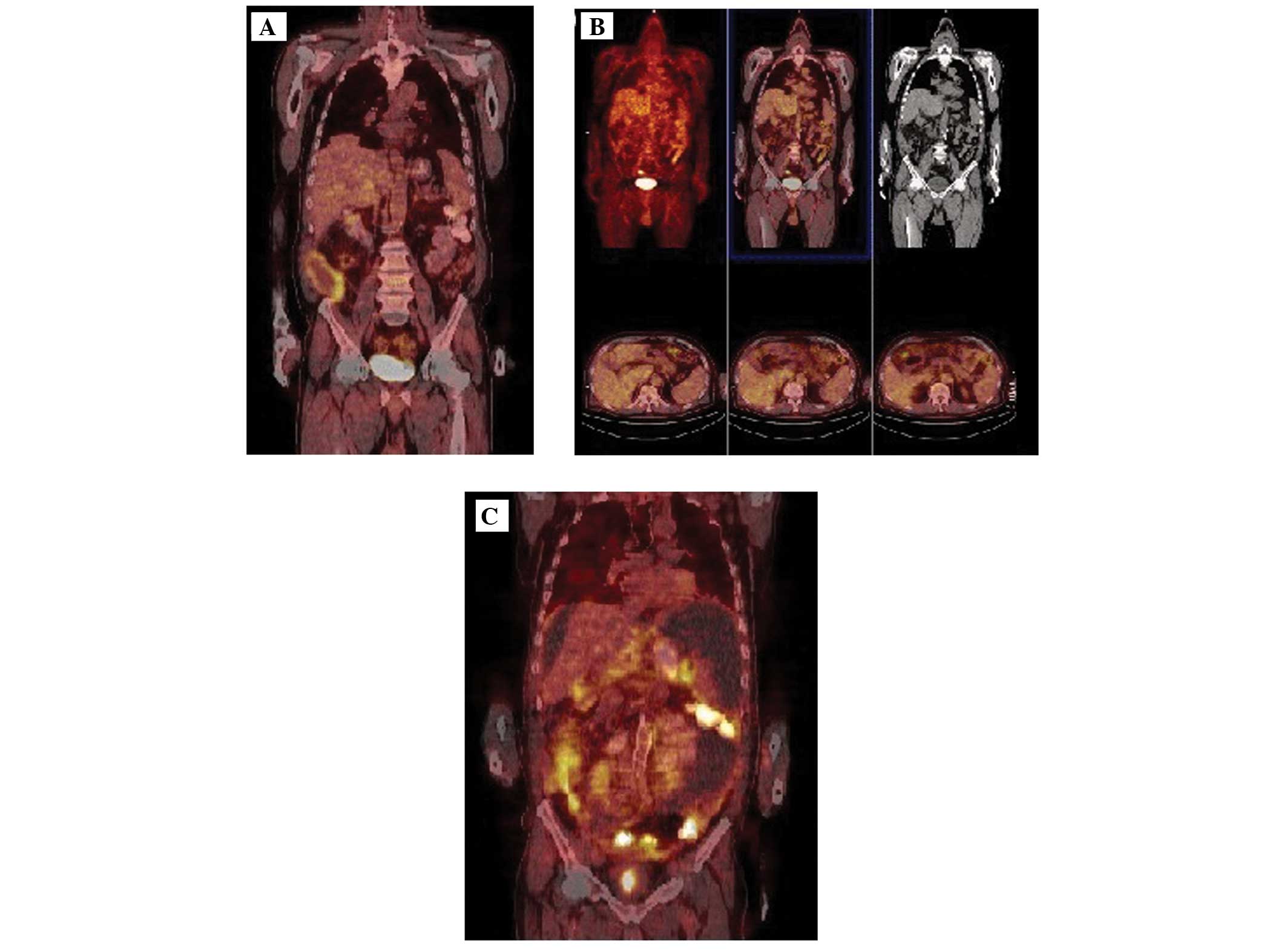
Tumor-Node-Metastasis staging system (16). The post-operative positron emission
tomography-computed tomography (PET-CT) scan demonstrated the
presence of a hypermetabolic lesion [standardized uptake value
(SUV), 8.5] located in the right lower abdomen (Fig. 2A). The lesion was diagnosed as an
abscess formation due to numerous neutrophils and pus identified by
aspiration biopsy. At follow-up 2 weeks subsequent to surgery, the
abscess had regressed due to aspiration and antibiotherapy for 14
days (1 g meropenem, 3 times daily; 500 mg metronizadole, 3 times
daily). PET-CT revealed that there was no metastasis to the
lymphoid system or bone marrow, which was confirmed by a bone
marrow biopsy.
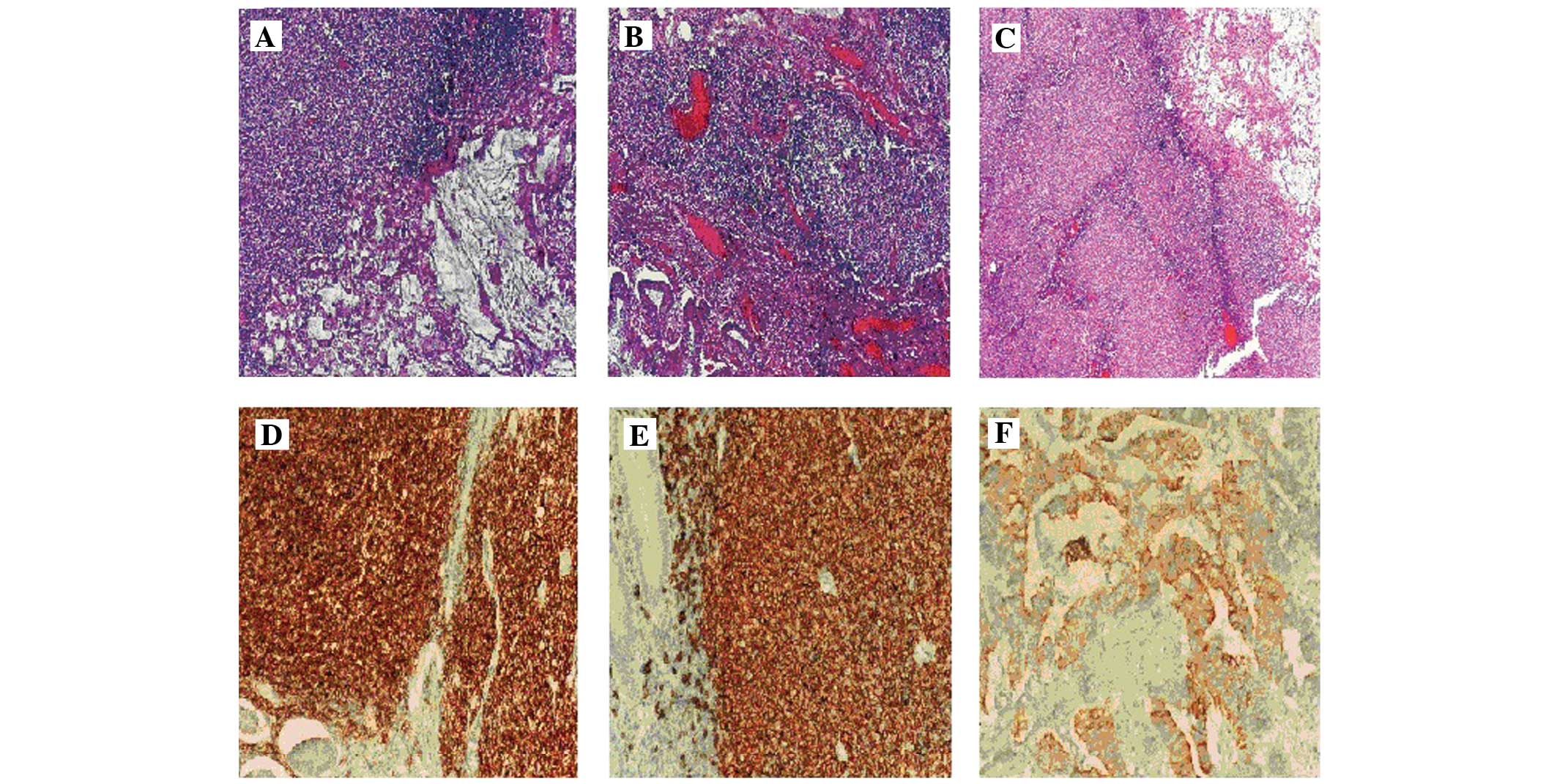 | Figure 1.Photomicrographs demonstrating the
presence of collision sections of adenocarcinoma and lymphoma in
the (A) lymph node (stain, H&E; magnification, x100) and (B)
cecum as mucin rich atypical glands and follicular lymphoma (stain,
H&E; magnification, x100) and the (C) lymph node (stain,
H&E; magnification, x40). Immunohistochemical staining revealed
(D) CD10 positivity (magnification, x200) and (E) CD20 positivity
(magnification, x200) in the lymph node and (F) pancytokeratin
positivity in the adenocarcinoma component of the cecum
(magnification, x200). CD, cluster of differentiation. H&E,
hematoxylin and eosin. |
The FL of the patient was stage 1EA, according to
the Ann Arbor staging system (17),
and the Follicular Lymphoma International Prognostic Index (FLIPI)
(18) score was 2, which indicated
that the patient was in the intermediate-risk of survival group.
The Eastern Cooperative Oncology Group (ECOG) performance status of
the patient was 0 (19). The
treatment of the patient was coordinated in October 2013 following
stabilization of the abscess. The adjuvant chemotherapy
administered to the patient consisted of 5-fluorouracil (2,000
mg/m2 on days 1 and 15) with leucovorin and oxaliplatin
(85 mg/m2 on days 1 and 15) (FOLFOX-4) for 28 days in 6
cycles. Following 6 cycles of FOLFOX-4 chemotherapy, the patient
presented with abdominal pain, and on physical examination it was
observed that the patient exhibited shifting dullness on percussion
indicating ascites. A PET-CT scan revealed novel SUVs in the
hepatic (SUV, 3.3), paraaortic (SUV, 2.9) and peripancreatic lymph
nodes (SUV, 2.8) and in the ascending colon (SUV, 6.1; Fig. 2B). Laboratory tests revealed that the
patient possessed a hemoglobin concentration of 10.8 g/dl, white
blood cell count of 6,500 cells/µl, platelet count of 153,000
cells/µl, LDH level of 320 units/l, ESR of 80 mm/h and CEA level of
2.5 ng/ml. The ascites possessed malignant features, which
confirmed that the lymphoma had progressed. The patient did not
exhibit stage B symptoms and was staged as 2EA FL using the Ann
Arbor staging system. The ECOG performance status of the patient
increased to 2. Consequently, chemotherapy was administered to the
patient, which consisted of cyclophosphamide (750 mg/m2
on day 1), vincristine (1.4 mg/m2 on day 1),
prednisolone (100 mg on days 1–5) and rituximab (375
mg/m2 on day 1) once every 3 weeks. The symptoms of the
patient rapidly progressed and the patient succumbed to the cancer
2 months subsequent to the initiation of treatment.
Discussion
NHL is the most common hematological malignancy,
consisting of a heterogeneous group of neoplastic disorders
(20). The pathogenesis of lymphoma
results from a combination of acquired somatic mutations, leading
to defects in the antitumor immunity of the patient and the local
microenvironment of the tumor (13).
The progression of lymphoma depends on various factors, including
the age and immune status of the patient (21). For the optimal management of lymphoma,
the medical history, ECOG performance status and symptoms of the
patient, history of lymphoma, including if the tumor was indolent
or aggressive, long-term outcome (curative or palliative) and B
cell or T cell origin of the tumor, and stage of the disease are
notable features. Indolent B-cell lymphomas are characterized by a
relapsing and remitting course (22).
Treatment should be decided by considering the grade, stage and
symptoms of the disease. FL is the most common subtype of indolent
NHL and accounts for 22% of newly diagnosed NHLs (21). Intermittent chemo therapy is provided
to control the symptoms of the disease, but this is not curative in
the majority of cases. Clinical observation, also termed watchful
waiting, is an important strategy for asymptomatic patients with a
low tumor burden, since spontaneous remission occurs in 8–10% of
patients, as a lack of curative therapy and an insufficient result
of early treatment has not improved the survival rate of patients.
The risk of FL developing into a more aggressive disease in
untreated indolent lymphomas is 20% at 5 years and 30% at 10 years
(23).
FL possesses a t(14;18) (q32;q21) translocation,
which is observed in 80–90% of patients and leads to the Bcl-2
oncogene becoming under the control of the immunoglobulin H locus,
which leads to impaired cellular apoptosis (24). Immunohistochemical analysis is used
for the determination of immonophenotype, and flow cytometry is
used for cell surface marker analysis. FL has a characteristic
immunophenotype, which is CD20+, CD10+ and
Bcl-2+. While grade 1 and 2 FLs exhibit an indolent
clinical behavior, grade 3 FL resembles a large diffuse B-cell
lymphoma. Currently, involved site radiation therapy (ISRT) is the
standard treatment for stage 1 or 2 low-grade FL, and patients that
were initially treated with radiation therapy (RT) have a median
overall survival time of ~14 years (25). According to previous studies, if the
tumor burden is low the preferred management of FL is RT or
clinical observation; however, if the tumor burden is high or
abdominal disease is present, rituximab with or without
chemotherapy is advised (25,26).
The present study reviewed collision tumor cases
from the literature and identified little information concerning a
treatment option for collision tumors. Lin et al (11) reported the case of a patient with
T3N1aM1 colon cancer and low-grade lymphoma, who received
oxaliplatin chemotherapy with leucovorin and 5-fluorouracil
(FOLFOX-6) chemotherapy for 6 cycles, followed by capecitabine for
24 months for the treatment of colon cancer. Chemotherapy was
continued due to suspicion of metastases in the lungs, however,
lymphoma did not recur during the 24-month follow-up. In addition,
Sasaki et al (10) reported
the case of a patient with T3N0M0 colon cancer and stage IV FL, who
received 6 courses of combined chemotherapy, consisting of
cyclophosphamide, doxorubicin, vincristine and prednisone regimen
with rituximab, for the treatment of FL. Malignant lymphoma was
dominant in this case and the initial systemic chemotherapy was
administered for malignant lymphoma, and a complete response was
obtained. However, there were multiple liver metastases of colon
adenocarcinoma present, despite the early stage of disease.
The present patient was diagnosed with stage 1EA and
grade 1 FL and was considered to belong to the intermediate-risk
group, according to the FLIPI score. Therefore, the T3N1M0 colon
cancer was considered to require treatment priority. Slow disease
progression is expected in grade 1 and stage 1 FL; therefore, a
watchful waiting strategy or local RT appeared to be a reasonable
management alternative for the present patient in the early stages
of FL. However, the progression of lymphoma developed unexpectedly
and rapidly within 6 months. The patient presented with a stage
IIEA symptomatic lymphoma progression, consisting of massive
abdominal lymphadenopaties and massive ascites (Fig. 2C). The immunodeficiency effect of
colon cancer chemotherapy may explain the progression of FL, which
is usually estimated to not occur for a long time. Consequently, a
reassessment of the present case suggests that the addition of ISRT
for FL with adjuvant colon cancer treatment may have been an
appropriate treatment option for the present patient.
The association between the immune system and cancer
development has been previously well described (27). This association may explain the
pathogenesis of the collision tumor and premature recurrence of FL
in the present case. The present study demonstrated the challenges
in deciding the optimal therapy for collision tumors and highlights
the importance of close follow-up for the two tumors during
treatment. Previous studies have limited data recommending
convenient treatment and follow-up strategies; therefore, novel
cases of patients with collision tumors in the literature may
provide additional information concerning optimal treatment
approaches and the prognosis of these patients.
References
|
1
|
Howlader N, Noone AM, Krapcho M, Garshell
J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,
et al: SEER Cancer Statistics Review (CSR) 1975–2012. National
Cancer Institute. Bethesda, MD: 2015.http://seer.cancer.gov/csr/1975_2012/Accessed.
January 15–2016
|
|
2
|
She WH, Day W, Lau PY, Mak KL and Yip AW:
Primary colorectal lymphoma: Case series and literature review.
Asian J Surg. 34:111–114. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tevlin R, Larkin JO, Hyland JM, O'Connell
PR and Winter DC: Primary colorectal lymphoma - A single centre
experience. Surgeon. 13:151–155. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Saber MM, Zeeneldin AA, Samra MA and Farag
SA: Primary gastrointestinal lymphoma in an Egyptian district: A
study using a population-based cancer registry. J Egypt Natl Canc
Inst. 25:95–101. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rodríguez-Abreu D, Llanos Muñoz M,
Provencio Pulla M, Rueda Domínguez A and Isla Casado D: SEOM
(Spanish Society for Medical Oncology): SEOM clinical guidelines
for the treatment of follicular non-Hodgkin's lymphoma. Clin Transl
Oncol. 12:760–764. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cornes JS: Multiple primary cancers:
Primary malignant lymphomas and carcinomas of the intestinal tract
in the same patient. J Clin Pathol. 13:483–489. 1960. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chazouillères O, Andréani T, Boucher JP,
Calmus Y, de Sigalony H, Nordlinger R and Poupon R: Rectal
adenocarcinoma in association with lymphoma (“collision tumor”).
Gastroenterol Clin Biol. 14:185–186. 1990.(In French). PubMed/NCBI
|
|
8
|
Mannweiler S, Dinges HP, Beham-Schmid C,
Hauser H, Starlinger M and Regauer S: Colliding / concomitant
tumors of the intestine: Report of 3 cases. Pathol Oncol Res.
9:188–192. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Eshra A, Al-Hendal A, Al Enezi M,
Al-Mishaan M and Dief Abo W: One patient, two lymphomas, three
primaries. Gulf J Oncolog. 1:39–43. 2010.
|
|
10
|
Sasaki S, Hatanaka K, Sahara N, Uekusa T,
Hirayama K, Shirahata A and Ishimaru M: Collision tumor of primary
malignant lymphoma and adenocarcinoma in the colon: Report of a
case. Surg Today. 40:975–981. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lin HH, Jiang JK and Lin JK: Collision
tumor of low-grade B-cell lymphoma and adenocarcinoma with
tuberculosis in the colon: A case report and literature review.
World J Surg Oncol. 12:1472014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chang H, Chuang WY, Shih LY and Tang TC:
Collision in the colon: Concurrent adenocarcinoma and diffuse large
B-cell lymphoma in the same tumour. Acta Clin Belg. 66:302–304.
2011.PubMed/NCBI
|
|
13
|
Upadhyay R, Hammerich L, Peng P, Brown B,
Merad M and Brody JD: Lymphoma: Immune evasion strategies. Cancers
(Basel). 30:736–762. 2015. View Article : Google Scholar
|
|
14
|
Kamel OW, van de Rijn M, Hanasono MM and
Warnke RA: Immunosuppression-associated lymphoproliferative
disorders in rheumatic patients. Leuk Lymphoma. 16:363–368. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mishra S, Malhotra P, Gupta AK, Singh PK,
Javed S and Kumar R: A semiquinone glucoside derivative isolated
from Bacillus sp. INM-1 provides protection against
5-fluorouracil-induced immunotoxicity. J Immunotoxicol. 12:56–63.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Edge S, Byrd DR, Compton CC, Fritz AG,
Greene FL and Trotti A: American Joint Committee on Cancer (AJCC)
Cancer Staging Manual (7th). Springer. New York, NY: 1432010.
|
|
17
|
Rosenberg SA: Validity of the Ann Arbor
staging classification for the non-Hodgkin's lymphomas. Cancer
Treat Rep. 61:1023–1027. 1977.PubMed/NCBI
|
|
18
|
Solal-Céligny P, Roy P, Colombat P, White
J, Armitage JO, Arranz-Saez R, Au WY, Bellei M, Brice P, Caballero
D, et al: Follicular lymphoma international prognostic index.
Blood. 104:1258–1265. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sørensen JB, Klee M, Palshof T and Hansen
HH: Performance status assessment in cancer patients. An
inter-observer variability study. Br J Cancer. 67:773–775. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chihara D, Ito H, Matsuda T, Shibata A,
Katsumi A, Nakamura S, Tomotaka S, Morton LM, Weisenburger DD and
Matsuo K: Differences in incidence and trends of haematological
malignancies in Japan and the United States. Br J Haematol.
164:536–545. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
No authors listed: Aclinical evaluation of
the International Lymphoma Study Group classification of
non-Hodgkin's lymphoma. The Non-Hodgkin's Lymphoma Classification
Project. Blood. 89:3909–3918. 1997.PubMed/NCBI
|
|
22
|
Armitage JO and Weisenburger DD: New
approach to classifying non-Hodgkin's lymphomas: Clinical features
of the major histologic subtypes. Non-Hodgkin's Lymphoma
Classification Project. J Clin Oncol. 16:2780–2795. 1998.PubMed/NCBI
|
|
23
|
Montoto S and Fitzgibbon J: Transformation
of indolent B-cell lymphomas. J Clin Oncol. 29:1827–1834. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cleary ML and Sklar J: Nucleotide sequence
of a t(14;18) chromosomal breakpoint in follicular lymphoma and
demonstration of a breakpoint-cluster region near a
transcriptionally active locus on chromosome 18. Proc Natl Acad Sci
USA. 82:7439–7443. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Campbell BA, Voss N, Woods R, Gascoyne RD,
Morris J, Pickles T, Connors JM and Savage KJ: Long-term outcomes
for patients with limited stage follicular lymphoma: Involved
regional radiotherapy versus involved node radiotherapy. Cancer.
116:3797–3806. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Friedberg JW, Byrtek M, Link BK, Flowers
C, Taylor M, Hainsworth J, Cerhan JR, Zelenetz AD, Hirata J and
Miller TP: Effectiveness of first-line management strategies for
stage I follicular lymphoma: Analysis of the National LymphoCare
Study. J Clin Oncol. 30:3368–3375. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Disis ML: Immune regulation of cancer. J
Clin Oncol. 28:4531–4538. 2010. View Article : Google Scholar : PubMed/NCBI
|