Introduction
Gastrointestinal stromal tumors (GISTs) comprise the
most common type of mesenchymal neoplasm arising from the
interstitial cells of Cajal (ICCs) of the myenteric plexus. GISTs
account for 0.1–3% of all gastrointestinal malignancies (1). The ICCs in the muscularis propria and
myenteric plexus are known as the pacemaker cells of the
gastrointestinal tract (2). GISTs
have been demonstrated to express the receptor tyrosine kinase
protein cluster of differentiation (CD)117, also known as
proto-oncogene c-Kit (3). GISTs
primarily arise from the stomach (60–70%) and between the ileum and
jejunum (25–30%), and are observed less frequently in the
colorectum (5–15%), duodenum (5%) and esophagus (2%) (4).
GISTs may additionally be observed in the omentum,
mesentery, retroperitoneum, pancreas and pelvis, as well as
adjacent to, but separate from, the stomach and intestine (5–7). GISTs
identified in the aforementioned locations have been termed
extragastrointestinal stromal tumors (EGISTs), as they occur
outside the gastrointestinal tract. The clinicopathological and
molecular profiles of EGISTs are similar to those of GISTs
(8). EGISTs have additionally been
reported in the gallbladder, prostate and rectovaginal septum
(9). To the best of our knowledge,
only a small number of cases of primary EGISTs originating from
pleuropulmonary sites have been previously reported (10,11).
The present study describes a rare case of primary
EGIST originating from the right pleural cavity of a 40-year-old
man. The diagnosis was confirmed by thoracoscopy and
immunohistochemistry.
Case report
A 40-year-old man was admitted on October 17, 2013
to the Department of Respiratory Medicine, Qianfoshan Hospital
Affiliated to Shandong University (Jinan, China) presenting with a
moderate cough, which was progessive, and pyrexia that had been
ongoing for one month. The patient had been expectorating ~10 ml of
grossly frothy sputum per day, without hemoptysis or emaciation.
Temperature, pulse, respiratory rate and blood pressure were 38.2°C
(normal range, 37°C), 100 beats/min (normal range, 60–100
beats/min), 20 times/min (normal range, 16–18 beats/min) and 128/85
mmHg (normal range, 90–140/60–90 mmHg), respectively. Laboratory
tests performed upon admission revealed the following: White blood
cell count, 14.9×109/l (normal range,
4–10×109/l); segmented neutrophils, 78% (normal range,
50–70%); hemoglobin concentration, 132 g/l (normal range, 120–170
g/l); erythrocyte sedimentation rate, 87 mm in the first hour
(normal range, 0–15 mm/h); C-reactive protein concentration, 173
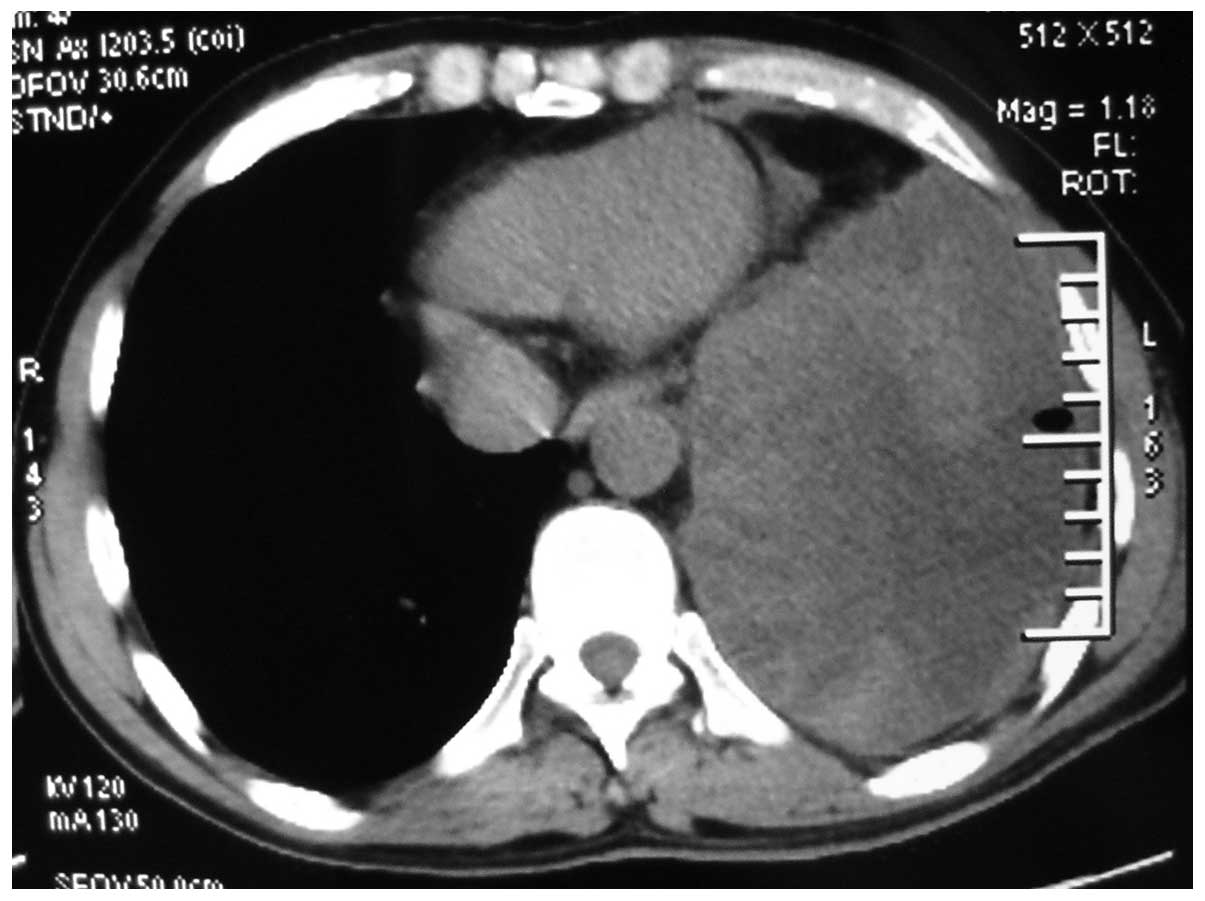
mg/l (normal range, 0–10 mg/l). A computed tomography (CT)
(Discovery CT 750 HD; GE Healthcare, Milwaukee, WI, USA) scan of
the chest revealed left-sided pleural effusion (Fig. 1). Bacterial (including mycobacterial)
and fungal examinations of the repeated sputum were negative. The
purified protein derivative skin test was also negative.
A closed drainage of the pleural cavity was
performed on day 2 following admission. Approximately 500 ml pale
red and turbid fluid was drained from the left pleural cavity. The
fluid was negative for bacterial, fungal or acid-fast organisms,
and no malignant cells were identified. Biochemical analysis of the
pleural fluid revealed the following: Adenosine deaminase, 38.2 U/l
(normal range, 0–25 U/l); total protein, 41.3 g/l (normal range,
0–30 g/l); glucose, 2.58 mmol/l (normal range, 3.9–6.1 mmol/l);
lactate dehydrogenase 3,422.8 U/l (normal range, 109–245 U/l).
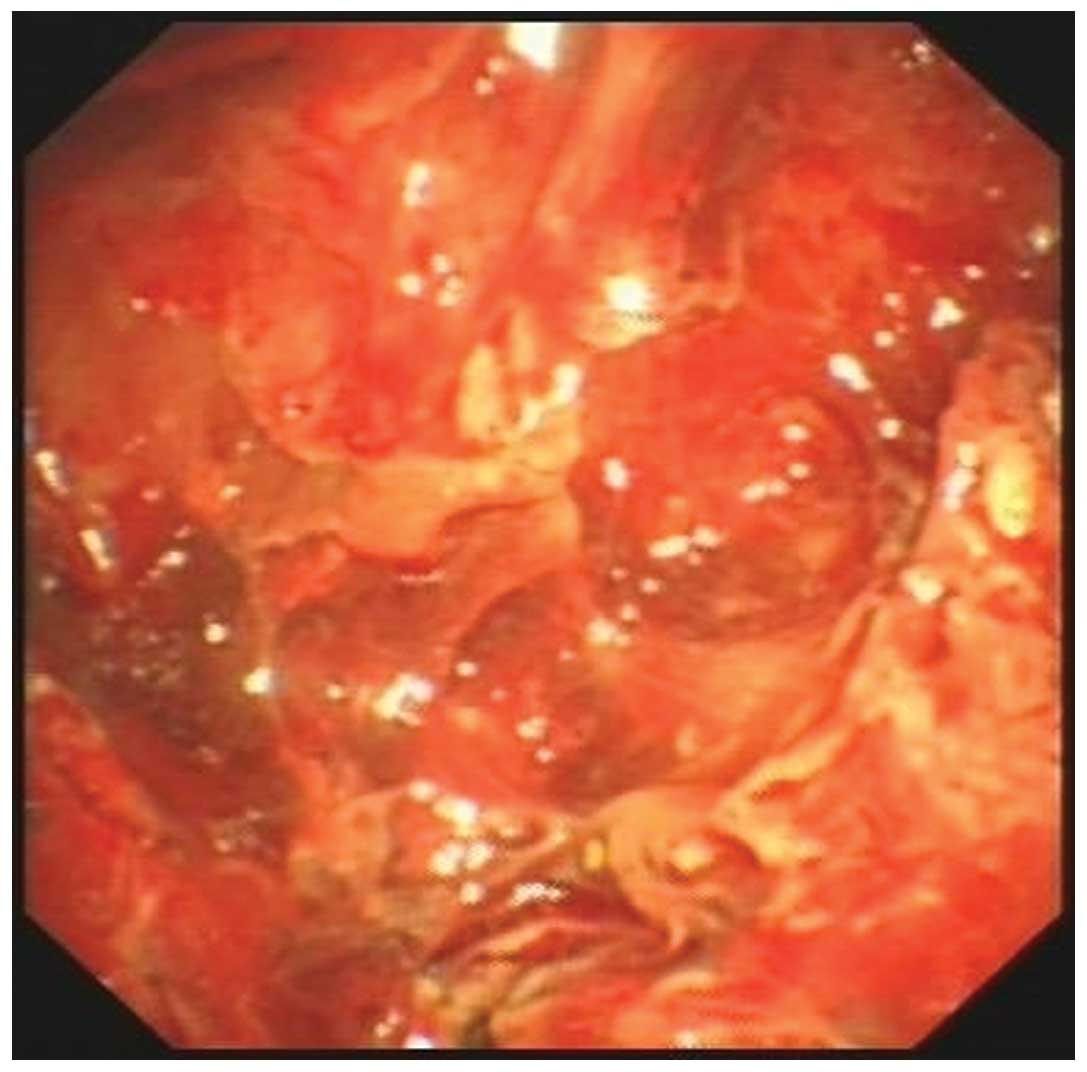
Thoracoscopy (LTF 240; Olympus Corporation, Tokyo, Japan)
identified multiple nodules of varying size throughout the parietal
pleura of the patient (Fig. 2). A
transthoracoscopic biopsy of the nodules was performed, and
formalin-fixed and paraffin-embedded tissues were sliced into 4-µm
sections on glass slides.
Immunohistochemitry was performed as follows: The
tissue sections were deparaffinized in xylene and rehydrated in
graded alcohol dilutions. Endogenous peroxidase activity was
blocked with 3% H2O2 at room temperature for
10 min. Subsequently, the tissues were fixed by heating at 95°C for
30 min and incubated overnight at 4°C with primary rabbit
monoclonal antibodies from Cell Marque™ (Sigma-Aldrich, St. Louis,
MO, USA) at a dilution of 1:200 against CD117 (catalog no. YR145)
and discovered on GIST-1 (DOG-1; catalog no. SP31). The tissues
were incubated for 20 min at room temperature with a secondary
antibody (catalog no. f03931; Roche Diagnostics, Shanghai, China).
Following staining for 3 min with 3,3′-Diaminobenzidine Substrate
(Roche Diagnostics), the tissues were counterstained with
hematoxylin (Roche Diagnostics). Negative controls were performed
by replacing the primary antibody with phosphate-buffered saline.
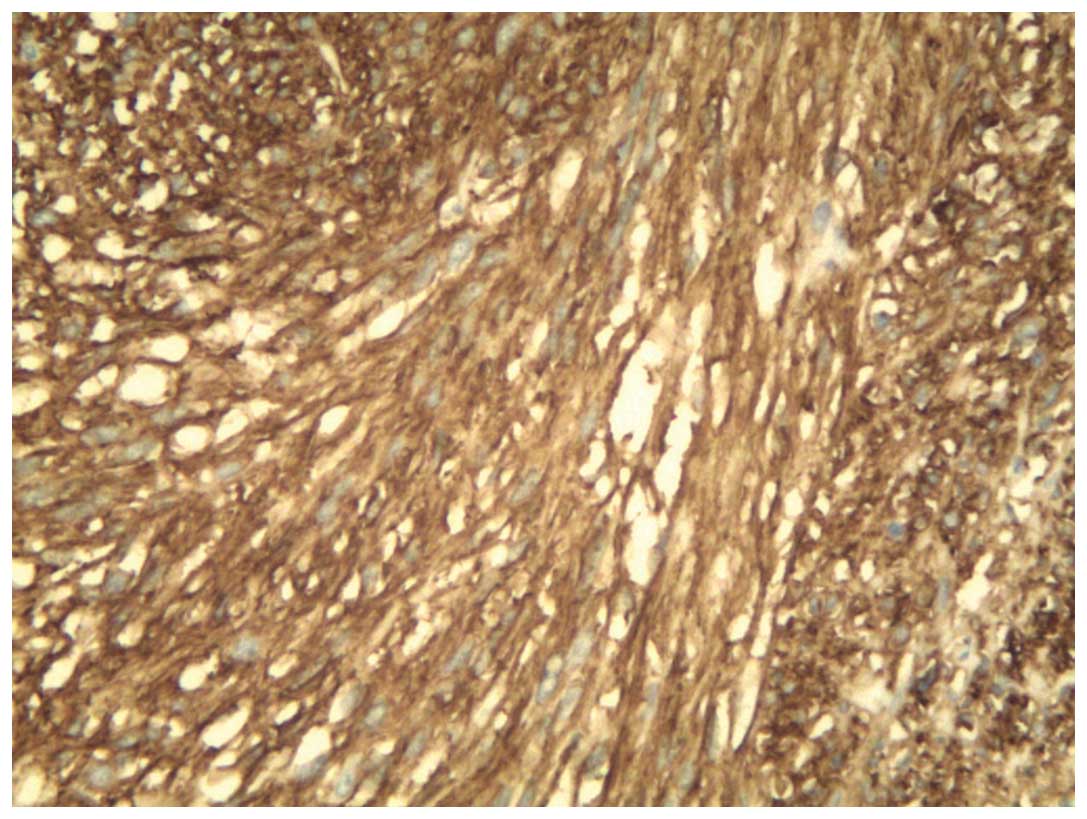
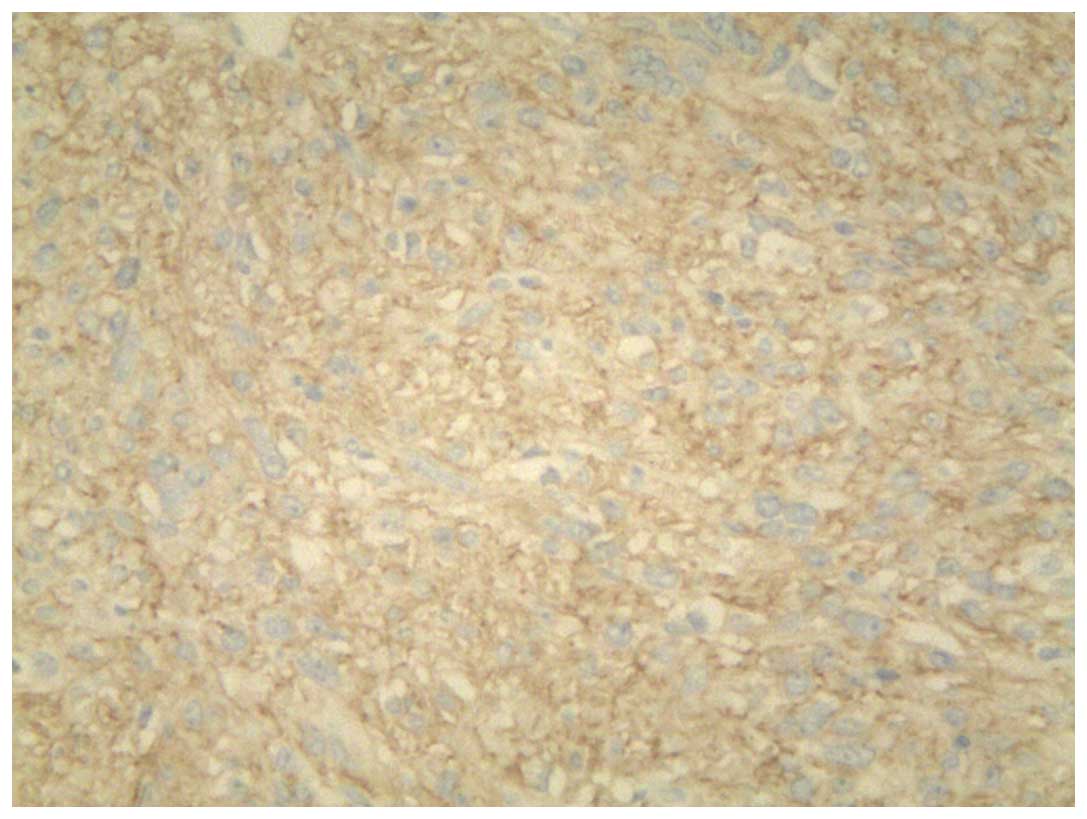
Immunohistochemistry revealed long spindle cells arranged in a
palisade or bundle arrangement, and positive staining for CD117
(Fig. 3) and DOG1 (Fig. 4) was observed. No tumors were
identified by fibergastroscopy or fibercoloscopy in the esophagus,
stomach and colorectum. The abdominal CT scan excluded the
possibility for pleural GIST metastases. The patient received
treatment of 400 mg imatinib mesylate daily for one year, following
a presumptive diagnosis of EGIST. The patient was examined with
chest CT every 3 months and no evidence of disease recurrence was
found. At the time of writing the present study, the patient
remained alive with no signs of disease recurrence.
Written informed consent was obtained from the
patient for the publication of the present study.
Discussion
The present study reports a case of a 40-year-old
man with multiple primary EGISTs in the left pleural cavity. The
diagnosis was verified by immunohistochemical staining for CD117
and DOG1, which are known to be markers for GISTs (12).
GISTs, the most commonly observed mesenchymal
neoplasms of the gastrointestinal tract, originate from ICCs or
associated CD117-positive-stem cell-like precursors (13,14). The
molecular pathogenesis of GISTs is typically driven by mutations of
the Kit gene that encodes CD117 (15). In addition, CD34 has been demonstrated
to exhibit strong and diffuse staining in ~70% of GIST cases
(16). GISTs may also be positive for
smooth muscle actin, and negative for desmin and S-100 protein
(7). GISTs are able to occur in ICCs
located anywhere along the gastrointestinal tract, including the
esophagus, stomach, duodenum, small intestine and colorectum
(17).
Primary EGISTs are rare, and typically manifest as
enlarging masses of variable duration in adults (18). In 80% of cases, EGISTs are observed in
the omentum and mesentery (19).
There have additionally been reports of EGISTs in the pleura,
pancreas and abdominal wall (20).
The origin of EGISTs remains to be elucidated; however, GISTs and
EGISTs have been confirmed to share various clinicopathological and
histological features (11). As the
presence of GISTs have been observed in numerous organs, including
the urinary bladder (21), prostate
(22), uterus (23), gall bladder (24) and myocardium (25), it can be assumed that EGISTs originate
from common precursor cells that are able to differentiate into
ICC-derived neoplasms outside of the gastrointestinal tract during
development (26). An alternative
explanation is that this type of tumor originates from the
pluripotent mesenchymal stem cells located outside the
gastrointestinal tract (10).
The clinical implications of EGISTs remain to be
fully elucidated. CT scanning is commonly used for the detection,
staging, surgical planning and follow-up of patients with EGISTs
(10). EGISTs should be considered in
the differential diagnosis of mesenchymal tumors, and
immunohistochemistry should be used to confirm the diagnosis
(27). CD117 is the most specific
diagnostic marker for EGISTs, and may be used to detect the product
of the proto-oncogene c-kit by immunohistochemical staining
(28). The majority of GISTs are
positive for CD117; only 5% demonstrate negativity (29). Immunohistochemical analysis of these
markers is being used as an alternative to expensive mutation
analysis. The positivity of an additional marker, DOG1, has been
shown to have a significant role in determining the diagnosis and
prognosis in EGISTs (30).
The prognosis of patients with EGISTs is believed to
be poorer than that of patients with GISTs (5), due to the fact that EGISTs are
frequently accompanied by adverse prognostic factors, including
high proliferative indices, large and distant metastases, and lymph
node involvement (11). Approximately
50% of patients with EGISTs have been reported to develop
metastasis or succumb to the primary tumors; therefore, EGISTs
should be considered as highly aggressive and be treated as
high-grade intra-abdominal sarcomas (6). The primary treatment for EGISTs is
surgical resection. Imatinib mesylate has been observed to be
beneficial for induction and adjuvant therapy (10). An increased number of therapeutic
strategies, that include the incorporation of molecular features,
are required to be established for the management of this
disease.
In summary, the current study presented a rare case
of GIST arising from the pleural cavity. The diagnosis was based on
pathological results and immunohistochemical findings, which
included expression of CD117 and DOG-1. EGISTs should be
acknowledged in the differential diagnosis in patients with pleural
effusion. Additional data regarding disease characterization,
treatment and prognosis are required for this rare disease.
Acknowledgements
The authors would like to thank Professor Xiaowei
(Department of Respiratory Medicine, Qilu Hospital, Shandong
University, Jinan, China) for assistance in the preparation of this
manuscript.
References
|
1
|
Liegl-Atzwanger B, Fletcher JA and
Fletcher CD: Gastrointestinal stromal tumors. Virchows Arch.
456:111–127. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Youm JB, Leem CH, Lee SR, Song IS, Kim HK,
Heo HJ, Kim BJ, Kim N and Han J: Modeling of stochastic behavior of
pacemaker potential in interstitial cells of Cajal. Prog Biophys
Mol Biol. 116:56–69. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Demetri GD, von Mehren M, Blanke CD, Van
den Abbeele AD, Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA,
Singer S, Janicek M, et al: Efficacy and safety of imatinib
mesylate in advanced gastrointestinal stromal tumors. N Engl J Med.
347:472–480. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Emory TS, Sobin LH, Lukes L, Lee DH and
O'Leary TJ: Prognosis of gastrointestinal smooth-muscle (stromal)
tumors: Dependence on anatomic site. Am J Surg Pathol. 23:82–87.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Miettinen M and Lasota J: Gastrointestinal
stromal tumors: Pathology and prognosis at different sites. Semin
Diagn Pathol. 23:70–83. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Reith JD, Goldblum JR, Lyles RH and Weiss
SW: Extragastrointestinal (soft tissue) stromal tumors: An analysis
of 48 cases with emphasis on histologic predictors of outcome. Mod
Pathol. 13:577–585. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Miettinen M, Monihan JM, Sarlomo-Rikala M,
Kovatich AJ, Carr NJ, Emory TS and Sobin LH: Gastrointestinal
stromal tumors/smooth muscle tumors (GISTs) primary in the omentum
and mesentery: Clinicopathologic and immunohistochemical study of
26 cases. Am J Surg Pathol. 23:1109–1118. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yamamoto H, Oda Y, Kawaguchi K, Nakamura
N, Takahira T, Tamiya S, Saito T, Oshiro Y, Ohta M, Yao T and
Tsuneyoshi M: c-kit and PDGFRA mutations in extragastrointestinal
stromal tumor (gastrointestinal stromal tumor of the soft tissue).
Am J Surg Pathol. 28:479–488. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hirano H, Yoshida T, Yoshimura H, Fukuoka
M, Ohmura N, Nishizawa Y, Tachibana S, Hirota S, Zozumi M and
Nishigami T: Extra-gastrointestinal stromal tumor of the pelvic
cavity: Case report. Med Mol Morphol. 45:173–177. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Long KB, Butrynski JE, Blank SD, Ebrahim
KS, Dressel DM, Heinrich MC, Corless CL and Hornick JL: Primary
extragastrointestinal stromal tumor of the pleura: Report of a
unique case with genetic confirmation. Am J Surg Pathol.
34:907–912. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yi JH, Sim J, Park BB, Lee YY, Jung WS,
Jang HJ, Ha TK and Paik SS: The primary extra-gastrointestinal
stromal tumor of pleura: A case report and a literature review. Jpn
J Clin Oncol. 43:1269–1272. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ríos-Moreno MJ, Jaramillo S, Gallardo
Pereira S, Vallejo A, Mora M, García-Escudero A, Amérigo J and
González-Cámpora R: Gastrointestinal stromal tumors (GISTs): CD117,
DOG-1 and PKCθ expression. Is there any advantage in using several
markers? Pathol Res Pract. 208:74–81. 2012.PubMed/NCBI
|
|
13
|
Kindblom LG, Remotti HE, Aldenborg F and
Meis-Kindblom JM: Gastrointestinal pacemaker cell tumor (GIPACT):
Gastrointestinal stromal tumors show phenotypic characteristics of
the interstitial cells of Cajal. Am J Pathol. 152:1259–1269.
1998.PubMed/NCBI
|
|
14
|
Hirota S, Isozaki K, Moriyama Y, Hashimoto
K, Nishida T, Ishiguro S, Kawano K, Hanada M, Kurata A, Takeda M,
et al: Gain-of-function mutations of c-kit in human
gastrointestinal stromal tumors. Science. 279:577–580. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Patil DT and Rubin BP: Genetics of
gastrointestinal stromal tumors: A heterogeneous family of tumors?
Surg Pathol Clin. 8:515–524. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rabin I, Chikman B, Lavy R, Sandbank J,
Maklakovsky M, Gold-Deutch R, Halpren Z, Wassermann I and Halevy A:
Gastrointestinal stromal tumors: A 19 year experience. Isr Med
Assoc J. 11:98–102. 2009.PubMed/NCBI
|
|
17
|
Miettinen M and Lasota J: Gastrointestinal
stromal tumors: Review on morphology, molecular pathology,
prognosis, and differential diagnosis. Arch Pathol Lab Med.
130:1466–1478. 2006.PubMed/NCBI
|
|
18
|
Iqbal N, Sharma A and Iqbal N:
Clinicopathological and treatment analysis of 13
extragastrointestinal stromal tumors of mesentery and
retroperitoneum. Ann Gastroenterol. 28:105–108. 2015.PubMed/NCBI
|
|
19
|
Gowrishankar S: Epithelioid omental
extra-gastrointestinal stromal tumor: Report of a case. Indian J
Pathol Microbiol. 54:618–619. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Alkhatib L, Albtoush O, Bataineh N,
Gharaibeh K, Matalka I and Tokuda Y: Extragastrointestinal Stromal
Tumor (EGIST) in the abdominal wall: Case report and literature
review. Int J Surg Case Rep. 2:253–255. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mekni A, Chelly I, Azzouz H, Ben Ghorbel
I, Bellil S, Haouet S, Kchir N, Zitouna M and Bellil K:
Extragastrointestinal stromal tumor of the urinary wall bladder:
Case report and review of the literature. Pathologica. 100:173–175.
2008.PubMed/NCBI
|
|
22
|
Anagnostou E, Miliaras D and
Panagiotakopoulos V: Diagnosis of gastrointestinal stromal tumor
(GIST) on transurethral resection of the prostate: A case report
and review of the literature. Int J Surg Pathol. 19:632–636. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Terada T: Gastrointestinal stromal tumor
of the uterus: A case report with genetic analyses of c-kit and
PDGFRA genes. Int J Gynecol Pathol. 28:29–34. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bolanaki H, Delladetsima I, Argyropoulou
P, Kapranou A, Kakolyris S, Simopoulos C and Karayiannakis AJ:
Primary Malignant Gastrointestinal Stromal Tumor (GIST) of the
Gallbladder: Report of a Case. J Gastrointest Cancer. 43(Suppl 1):
151–155. 2012. View Article : Google Scholar
|
|
25
|
Bashir U, Qureshi A, Khan HA and Uddin N:
Gastrointestinal stromal tumor with skeletal muscle, adrenal and
cardiac metastases: An unusual occurrence. Indian J Pathol
Microbiol. 54:362–364. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Casella C, Villanacci V, D'Adda F, Codazzi
M and Salerni B: Primary extra-gastrointestinal stromal tumor of
retroperitoneum. Clin Med Insights Oncol. 6:189–197. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Patnayak R, Jena A, Parthasarathy S,
Prasad PD, Reddy MK, Chowhan AK, Rukamangadha N and Phaneendra BV:
Primary extragastrointestinal stromal tumors: A clinicopathological
and immunohistochemical study - a tertiarycare center experience.
Indian J Cancer. 50:41–45. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Joensuu H, Roberts PJ, Sarlomo-Rikala M,
Andersson LC, Tervahartiala P, Tuveson D, Silberman S, Capdeville
R, Dimitrijevic S, Druker B and Demetri GD: Effect of the tyrosine
kinase inhibitor STI571 in a patient with a metastatic
gastrointestinal stromal tumor. N Engl J Med. 344:1052–1056. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Xu C, Han H, Wang J, Zhang B, Shao Y,
Zhang L, Wang H, Wang H, Wu Y, Li X, et al: Diagnosis value of
CD117 and PDGFRA, alone or in combination DOG1, as biomarkers for
gastrointestinal stromal tumors. Ann Transl Med.
3:3082015.PubMed/NCBI
|
|
30
|
Kim KH, Nelson SD, Kim DH, Choi KU, Kim
SJ, Min KW, Jang KS, Paik SS, Oh YH, Chae SW, et al: Diagnostic
relevance of overexpressions of PKC-θ and DOG-1 and KIT/PDGFRA gene
mutations in extra-gastrointestinal stromal tumors: A Korean
six-centers study of 28 cases. Anticancer Res. 32:923–937.
2012.PubMed/NCBI
|