Introduction
Cervical cancer is a significant worldwide health
problem, particularly in developing countries. Globally, cervical
cancer accounted for the third most commonly diagnosed type of
cancer and the fourth leading cause of cancer-related mortality in
women in 2008 (1). Patients in the
early stages of cervical cancer typically exhibit no symptoms,
whereas various symptoms, such as abnormal vaginal bleeding, pelvic
pain and pain during sexual intercourse, are observed in the
advanced stages (2,3). Cancer screening with the Papanicolaou
smear test has been demonstrated to markedly reduce the occurrence
of advanced cervical cancer and mortality (2,3). However,
treatment of cervical cancer varies significantly; for example, the
early stages of the disease are treated with surgery, while the
later stages of the disease are treated only with chemotherapy
and/or radiotherapy. Generally, cervical cancer is radiosensitive;
thus, radiation may be used in all stages of disease, including
when surgery is not an option for a patient in the early stages of
disease (3). Concurrent
cisplatin-based chemoradiotherapy is the standard treatment for
locally advanced cervical cancer. Cervical cancer patients with
enlarged para-aortic nodes (PAN) may be treated with radical
hysterectomy with removal of the lymph nodes or radiation therapy,
whereas larger early stage tumors may be treated with radiation
therapy and cisplatin-based chemotherapy, hysterectomy with
adjuvant radiation therapy, or cisplatin chemotherapy followed by
hysterectomy (3,4). By contrast, advanced stages of cervical
cancer (stages IIB-IVA) are typically treated with radiation
therapy and cisplatin-based chemotherapy (3,4). However,
cervical cancer with metastasis to the PAN has a poor prognosis
(5,6).
In such cases, concurrent cisplatin-based chemotherapy with
extended-field radiotherapy (EFRT) is the standard treatment
strategy. Previous studies have demonstrated an improvement in
disease control using EFRT and concurrent chemotherapy, and have
shown a positive effect on overall survival (OS) compared with
radiotherapy alone (7–10). However, the high levels of acute and
chronic toxicities associated with EFRT are still potential
barriers. In addition to decreasing patient quality of life, acute
toxicity leads to premature termination of chemotherapy, and the
number of chemotherapy cycles is an independent predictor of
survival (11). Therefore, there is
an urgent need to evaluate novel treatment strategies to reduce
toxicity and improve treatment efficacy. A previous study discussed
the benefits of intensity-modulated radiotherapy (IMRT), which
provides more conformal dose distribution into the tumor lesion.
Furthermore, IMRT reduces the absorbed dose and the volume of the
organ at risk (OAR), thus leading to reduced acute and late
toxicity (12). Nedaplatin is an
analog of cisplatin that exhibits less nephrotoxicity,
neurotoxicity and gastrointestinal (GI) toxicity than cisplatin
(13). Thus, the present study
assessed the efficacy and toxicity of extended field-IMRT (EF-IMRT)
with concurrent nedaplatin treatment in cervical cancer.
Patients and methods
Ethics
The present study was approved by the Ethics
Committee of Anhui Tumor Hospital and Anhui Provincial Hospital
(Hefei, China). Informed consent was obtained from all patients
included in the current study.
Patients
In the present study, a total of 48 women with
histology-confirmed cervical cancer were recruited for treatment
with definitive EF-IMRT plus concurrent weekly nedaplatin from
Anhui Tumor Hospital and Anhui Provincial Hospital between February
2012 and April 2014. Patients with synchronous malignancies or
distant metastases at diagnosis were excluded from the study. Among
the total patients, 12 patients exhibited enlarged para-aortic
lymph nodes only, 17 patients exhibited multiple enlarged pelvic
lymph nodes, and 19 patients had enlarged para-aortic and pelvic
lymph nodes. The decision to use EF-IMRT was made by the medical
oncologists. Lymph nodes that measured as >1 cm in the short
axis diameter were considered malignant. Patients with confirmed
tumor metastasis to the lymph nodes (n=9) underwent pelvic
lymphadenectomy.
The median age of the 48 patients was 51 years
(range, 31–70 years), 45 (93.75%) of which had cervical squamous
cell carcinoma and 3 (6.25%) of which had adenocarcinoma. A medical
history, physical examination, gynecologic pelvic examination,
complete blood cell count, blood chemistry profile, chest X-ray or
computed tomography (CT) scan, abdominal CT scan, and pelvic
magnetic resonance imaging (MRI)/CT scan were obtained for all
patients. In addition, 7 patients received positron emission
tomography (PET). The patients were staged according to the staging
system of the International Federation of Gynecology and Obstetrics
(14), as follows: 3 patients (6.3%)
had stage IB disease, 1 patient (2.1%) had stage IIA disease, 25
patients (52.1%) had stage IIB disease, 3 patients (6.3%) had stage
IIIA disease and 16 patients (33.3%) had stage IIIB disease
(Table I).
 | Table I.Patient characteristics (n=48). |
Table I.
Patient characteristics (n=48).
| Characteristic | Patients, n (%) |
|---|
| Age, years |
|
|
Median | 51 |
|
Range | 31–70 |
| Histopathology |
|
|
Squamous | 45 (93.8) |
|
Adenocarcinoma | 3 (6.3) |
| FIGO stage |
|
|
IB2 | 3 (6.3) |
|
IIA | 1 (2.1) |
|
IIB | 25 (52.1) |
|
IIIA | 3 (6.3) |
|
IIIB | 16 (33.3) |
| Lymph node
involvement |
|
|
Para-arotic nodes positive
only | 12 (25.0) |
| Pelvic
nodes positive only | 17 (35.4) |
|
Para-aortic and pelvic nodes
positive | 19 (39.6) |
| Treatment response
according to FIGO stage |
|
|
IB2 |
|
|
CR | 3 (6.3) |
|
PR | 0 (0.0) |
|
IIA |
|
|
CR | 1 (2.1) |
|
PR | 0 (0.0) |
|
IIB |
|
|
CR | 25 (52.1) |
|
PR | 0 (0.0) |
|
IIIA |
|
|
CR | 2 (4.2) |
|
PR | 1 (2.1) |
|
IIIB |
|
|
CR | 15 (31.3) |
|
PR | 1 (2.1) |
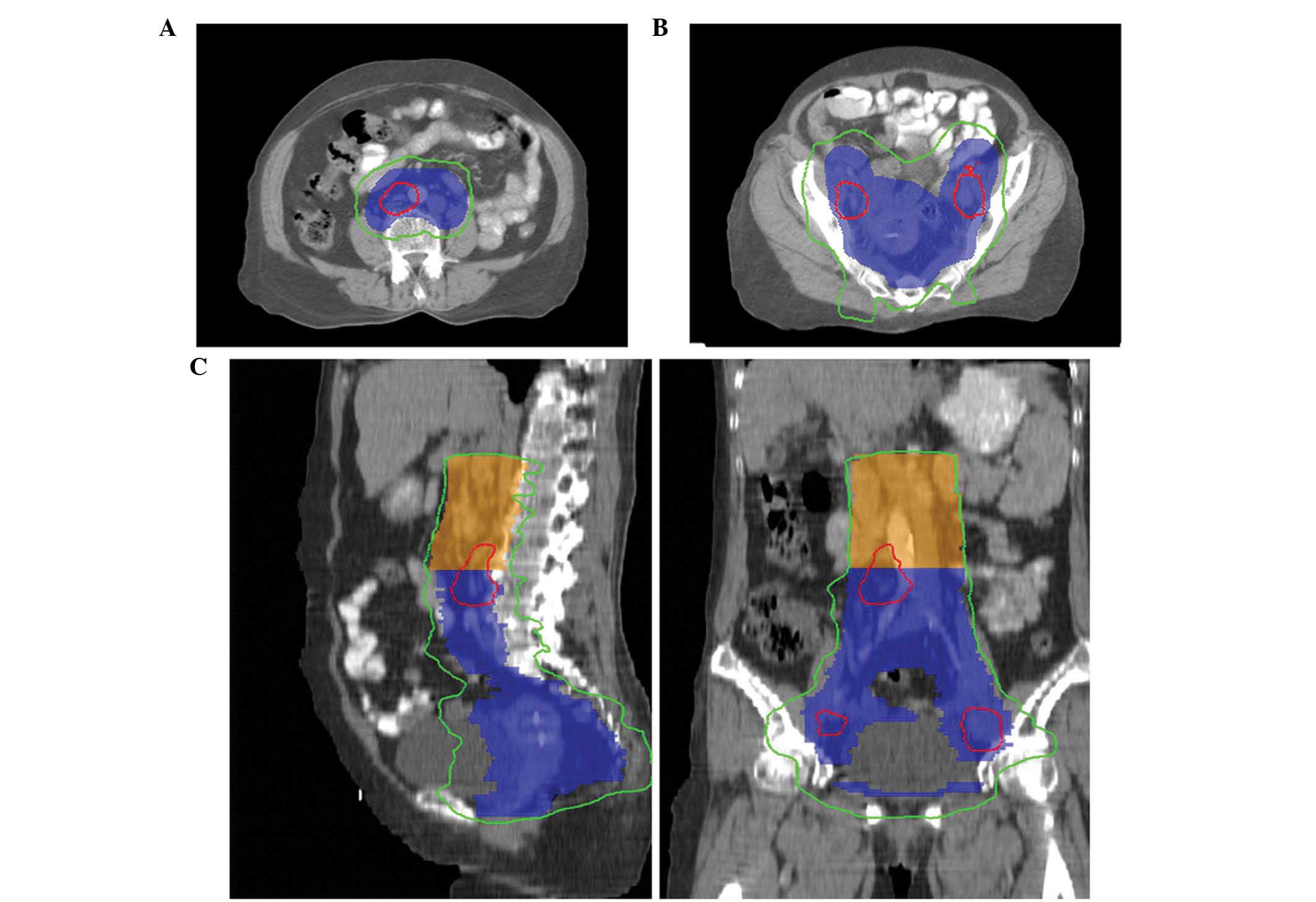
Radiotherapy technique
All patients underwent CT-based planning with custom
immobilization. The clinical target volume (CTV) included
CTV1 and CTV2. CTV1 consisted of
CTVcervix (including the gross tumor and cervix),
CTVuterus (including total uterus only),
CTVparametria [including the parametria; the entire
mesorectum was added to the parametrial volume and superior half of
the vagina (for patients with stage IIIA disease, the entire vagina
was included] and CTVnode [including regional lymph
nodes (common, internal, external iliac, obturator and presacral
lymph nodes], according to the consensus guidelines (15,16).
Different margins were added to form the planning target volume
(PTV). A 10–15 mm planning margin was applied around the cervix and
gross tumor, a 15–20 mm margin around the uterus, and a 7 mm margin
around the remainder of the CTV1 to form
PTV1. By contrast, CTV2 included the
para-aortic lymph nodes region, the lower border (bifurcation of
abdominal aorta) and the upper border (7 mm below the T12/L1
interspace). A 7 mm planning margin was applied around
CTV2 to define PTV2. The gross tumor volume
of nodes (GTVnd) included enlarged lymph nodes, and a 5 mm margin
was used around the GTVnd to produce the pGTVnd. The prescribed
dose of PTV1 ranged between 45 and 50.4 Gy in 1.8–2.0 Gy
daily fractions lasting 7–8 min, and of PTV2 ranged
between 39.6 and 50 Gy in 1.8–2.0 Gy daily fractions lasting 7–8
min. Fifteen patients received the same prescribed dose for
PTV1 and PTV2, while the others received the
different prescribed dose for PTV1 and PTV2.
pGTVnd was treated with a total dose of 55–60 Gy in 2.0–2.4 Gy
daily fractions using simultaneous integrated boost-IMRT (Fig. 1). The target planning constraints were
as follows: i) >99% of the PTV received >90% of the
prescribed dose and >97% PTV received >97% of the prescribed
dose; and ii) <1% of the PTV received >115% of the prescribed
dose. The maximum dose applied to all tissues was <115–117% of
the prescription dose. The normal tissue planning constraints were
as follows: i) Rectum [volume receiving >50 Gy (V50), <30%;
maximum dose, <52 Gy]; ii) small bowel [volume receiving >45
Gy (V45), <250 cm3]; iii) bladder [volume receiving
>50 Gy (V50), <30%; maximum dose, <52 Gy]; iv) bone marrow
[volume receiving >20 Gy (V20), <75%; volume receiving >10
Gy (V10), <95% (35/48 patients were planned prior to the
introduction of bone marrow sparing)]; v) kidney [volume receiving
>20 Gy (V20), <20%; mean dose, <18 Gy] vi) liver [volume
receiving >30 Gy (V30), <40%]; and vii) spinal cord (maximum
dose, <45 Gy). Radiotherapy was suspended when the peripheral
neutrophil count was <500/mm3 or the peripheral
platelet count was <50,000/mm3 until the patient
recovered. Patients were treated with a Varian Trilogy System
Linear Accelerator (Varian Medical Systems, Palo Alto, CA, USA) at
Anhui Tumor Hospital while Elekta Synergy (Elekta, Crawley, UK) was
used at Anhui Provincial Hospital. All IMRT treatments were planned
with Pinnacle3 v 9.10 (Philips Medical Systems,
Fitchburg, WI, USA), and delivered using the step and shoot
mode.
Following EF-IMRT, all patients underwent high
dose-rate (HDR) intracavitary brachytherapy using iridium-192. Five
fractions of 5.5–6.0 Gy each were delivered to point A (defined as
2 cm lateral to the central canal of the uterus and 2 cm up from
the mucous membrane of the lateral fornix in the axis of the
uterus) once or twice weekly, with no EF-IMRT treatment
administered on the day of the HDR intracavitary treatment.
Chemotherapy
Nedaplatin, developed by Jiangsu Aosaikang
Pharmaceutical Co., Ltd. (Nanjing, China), was dissolved in 500 ml
saline and infused intravenously. The first cycle was administered
on the first day of EF-IMRT. All patients received weekly
nedaplatin at a median dose of 30 mg/m2 (range, 25–40
mg/m2) once a week for 5 weeks (a total dose of 150
mg/m2 every 5 weeks) during the course of EF-IMRT.
Anti-emetics, such as 5-hydroxytryptamine-3 receptor antagonist,
were administered routinely prior to nedaplatin infusion. However,
nedaplatin infusion was delayed if the peripheral neutrophil count
was <1,000/mm3 or the peripheral platelet count was
<75,000/mm3. The optimal number of chemotherapy
cycles administered was 5.
Evaluation of treatment efficacy and
follow-up of patients
During treatment, all the patients underwent weekly
physical examinations, complete blood counts, and liver and renal
function tests prior to the concurrent chemotherapy. Patient
response was evaluated for 3 months after completion of the
treatment. Complete response (CR) was defined clinically
(gynecological pelvic examination and imaging) as the disappearance
of all gross lesions. Partial response (PR) was defined as a
>50% reduction of the tumor. Stable disease (SD) was defined as
the presence of the tumor with <50% reduction of the tumor size.
Progressive disease (PD) was defined as a >25% increase in the
size of the local tumor or the appearance of any new lesion.
The treatment responses of all the patients were
assessed by a radiation oncologist and/or a gynecological
oncologist at 4 weeks and 3 months after the completion of
treatment, and then followed up every 3 months during the first 2
years, and every 6 months thereafter. Follow-up evaluation included
physical examination, gynecological pelvic examination, abdominal
ultrasound or CT, pelvic ultrasound or CT and/or MRI, blood counts,
and chemistry profiles. These patients were followed up regularly
and the most recent follow-up was performed in August 2014.
Evaluation of treatment
toxicities
Acute toxicity was measured from initiation of
EF-IMRT to 90 days after the completion of treatment, while late
toxicity was measured from >90 days after the completion of the
treatment. Acute toxicity was graded according to the National
Cancer Institute Common Terminology Criteria for Adverse Events
version 3.0 (17) and late toxicity
was graded according to the Radiation Therapy Oncology Group (RTOG)
(18) late radiation morbidity
scoring criteria.
Statistical analysis
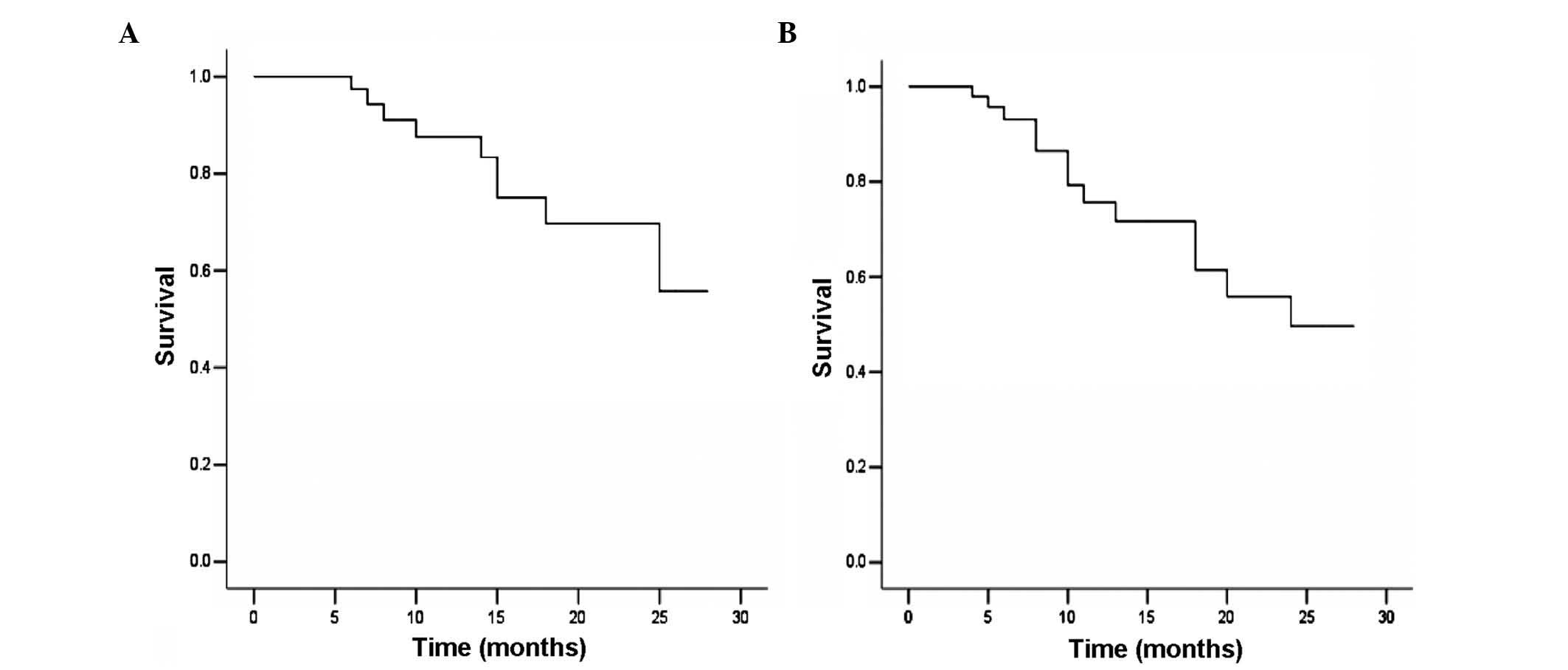
Disease-free survival (DFS) and OS rate were
analyzed using Kaplan-Meier curves, and treatment outcome was
estimated by using Kaplan-Meier curves, in addition to the log-rank
test for univariate analysis and the Cox proportional hazards model
for multivariate analysis. SPSS software (version 13.0; SPSS, Inc.,
Chicago, IL, USA) was used to perform the statistical analyses.
Data are presented as the mean ± standard deviation, and P<0.05
was considered to indicate a statistically significant
difference.
Results
Treatment response
Patient response was evaluated for 3 months after
the completion of treatment. It was found that 46 patients had CR
and 2 had PR, with a response rate of 100% (Tables I and II). After 10 and 11 months, 2 patients with
CR exhibited relapsed disease inside the radiation field and lung
metastasis, while 9 patients with CR developed distant metastasis
only. The most common site of distant metastasis was the lung (5 to
the lung, 3 to the mediastinal lymph nodes, 3 to the inguinal lymph
nodes, 3 to the supraclavicular lymph nodes, 1 to the liver and 1
to the lumbar vertebrae bone) (Table
II).
 | Table II.Treatment responses and failures. |
Table II.
Treatment responses and failures.
| Treatment responses
and failures | Patients, n |
|---|
| Treatment
response |
|
| CR | 46 |
| PR | 2 |
| Treatment
failure |
|
| PR and
metastasis to the lung | 1 |
| CR and
recurrence and metastasis to the lung | 2 |
| CR and distant
metastasis |
|
| Liver
only | 1 |
| Lung
only | 1 |
|
Inguinal lymph nodes only | 1 |
|
Supraclavicular lymph
nodes | 1 |
|
Inguinal lymph nodes and
lung | 1 |
|
Inguinal lymph nodes and
bone | 1 |
|
Mediastinal lymph nodes
only | 1 |
|
Mediastinal and
supraclavicular lymph nodes | 2 |
OS and DFS
At the most recent follow-up in August 2014, 9/48
patients (18.8%) had succumbed to disease, between 6 and 25 months
after treatment. Of these 9 patients, 2 had exhibited PR (one
sucumbed to suicide at 8 months after therapy, the other succumbed
to local tumor progression and distant metastasis). Among the
remaining 7 patients, 1 patient succumbed due to local tumor
relapse and distant metastasis, and 6 succumbed to distant
metastasis. The median follow-up time was 12 months (range, 4–28
months). The 12-month OS and DFS were 87.5 and 75.8%, respectively,
and the 24-month OS and DFS were 69.7 and 49.7%, respectively
(Fig. 2).
Treatment toxicities
None of the 48 patients succumbed within 1 month
after treatment, although 20/48 patients (41.7%) had grade 3 or
higher neutropenia, 4 patients (8.3%) had grade 3 or higher
thrombocytopenia, and 2 patients (4.2%) had grade 3 diarrhea. No
patients developed grade 3 or higher vomiting (Table III).
 | Table III.Treatment toxicities. |
Table III.
Treatment toxicities.
|
| Cases, n (%) |
|---|
|
|
|
|---|
| Toxicity | Grade 0 | Grade 1 | Grade 2 | Grade 3 | Grade 4 |
|---|
| Acute |
|
|
Diarrhea | 22 (45.8) | 11 (22.9) | 13 (27.1) | 2 (4.2) | 0 (0.0) |
|
Vomiting | 32 (66.7) | 9 (18.8) | 7 (14.6) | 0 (0.0) | 0 (0.0) |
|
Genitourinary | 45 (93.8) | 2 (4.2) | 1 (2.1) | 0 (0.0) | 0 (0.0) |
| Hematological |
|
|
Anemia | 19 (39.6) | 16 (33.3) | 9 (18.8) | 4 (8.3) | 0 (0.0) |
|
Leukopenia | 1 (2.1) | 9 (18.8) | 17 (35.4) | 18 (37.5) | 3 (6.3) |
|
Neutropenia | 1 (2.1) | 9 (18.8) | 18 (37.5) | 19 (39.0) | 1 (2.1) |
|
Thrombcytopenia | 22 (45.8) | 15 (31.3) | 7 (14.6) | 3 (6.3) | 1 (2.1) |
| Late |
|
|
Gastrointestinal | 33 (68.8) | 3 (6.3) | 10 (20.8) | 2 (4.2) | 0 (0.0) |
|
Genitourinary | 43 (89.6) | 2 (4.2) | 3 (6.3) | 0 (0.0) | 0 (0.0) |
Specifically, 44/48 patients (91.7%) were able to
complete 5 weeks of concurrent nedaplatin chemotherapy, and only 4
patients (8.3%) received 3/4 cycles of chemotherapy due to grade 4
hematologic toxicity. A platelet transfusion was required by 1
patient, however, all patients completed radiotherapy. The median
treatment duration from EF-IMRT to the last day of brachytherapy
was 52 days (range, 48–61 days) and 45/48 patients (93.75%)
completed radiotherapy in 8 weeks. Furthermore, 2 patients (4.2%)
developed grade 3 late GI toxicity, 1 patient experienced a sigmoid
stricture that required colostomy, and 1 patient a experienced
small intestine obstruction that required surgical management.
Discussion
In the present study, patients with cervical cancer
were treated with EF-IMRT plus concurrent nedaplatin therapy for ≤8
weeks. All patients responded to this treatment regimen, although
24/48 (45%) patients experienced grade 3 or 4 neutropenia and
thrombocytopenia. However, this treatment regimen featured a low
rate of high-grade GI toxicity. The 12-month OS and DFS were 87.5
and 75.8%, respectively, and the 24-month OS and DFS were 69.7 and
49.7%, respectively. Thus, the present study indicates that EF-IMRT
plus concurrent nedaplatin treatment in cervical patients is a safe
and highly effective treatment strategy.
EFRT causes known side-effects on the bone marrow
and small bowel, and the addition of concurrent chemotherapy to
EFRT only exacerbates its toxicity. Previously, a prospective phase
II cooperative group clinical trial, in which para-aortic lymph
nodes were treated with 4,500 cGy, reported grade 3–4 acute GI
toxicity in 18.6% of patients. Furthermore, a late morbidity
actuarial risk of 14% at 4 years primarily involved the rectum in
cervical cancer patients treated with concurrent chemotherapy and
EFRT (7). However, the use of the
IMRT significantly reduced doses to the OAR, and decreased GI and
hematological toxicities (12).
Consensus guidelines for delineation of the CTV have been published
(15,16). The theoretical drawbacks of IMRT
treatment include dose inhomogeneity within target volumes, longer
treatment times than conventional radiotherapy and the uncertainty
of organ motion. However, previous studies demonstrated the
advantages of IMRT over EFRT delivered by three-dimensional
conformal radiotherapy for extended field treatments (19–21). For
example, Portelance et al (19) performed a dosimetric analysis to
determine the feasibility of pelvic and para-aortic IMRT in 10
patients who underwent CT simulation from T2 to the ischial
tuberosities with conventional 2- and 4-field plans versus 4-, 7-
and 9-fields IMRT plans. IMRT resulted in a statistically
significant reduction (P<0.05) in the volume of small bowel
irradiation, demonstrating 11, 15 and 13.6% reduction in the 4-, 7-
and 9-field IMRT, respectively. By contrast, 35 and 34% reduction
occurred in the conventional 2- and 4-field plans, respectively.
The rectal dose was significantly lower with IMRT (P<0.001)
(19). Furthermore, Gerszten et
al demonstrated a significant reduction in critical organ
irradiation with EF-IMRT, and proposed that the treatment may
reduce both acute and late treatment-associated side-effects
(20). Salama et al reported
the preliminary outcome and toxicity of EF-IMRT for gynecological
malignancies, in which 13 women with gynecologic malignancies
tolerated EF-IMRT and only 2 patients experienced grade 3 or higher
acute toxicity (21). By contrast,
Jensen et al demonstrated high toxicity rates in patients
with cervical cancer that underwent EF-IMRT and concurrent
cisplatin treatment; acute grade 3 or higher GI toxicity was 19.0%
and acute grade 3 or higher hematological toxicity was 57.1%
(22). In the current study, 20/48
patients (41.7%) exhibited grade 3 or higher neutropenia, 4
patients (8.4%) had grade 3 or higher thrombocytopenia and 2
patients (4.2%) developed grade 3 diarrhea. This further indicates
that the hematological toxicity was significant, however, the
majority of patients tolerated the side effects, with >90% of
patients able to complete the treatment regime.
Nedaplatin is an analog of cisplatin that exhibits
less nephrotoxicity, neurotoxicity and GI toxicity than cisplatin
itself. A previous phase I study determined that the recommended
weekly dose of nedaplatin was 30 mg/m2, administered for
>5 cycles and ≤8 cycles if possible. Weekly administration of
nedaplatin may be more tolerable and less toxic than weekly
administration of cisplatin (23).
Furthermore, a phase II study confirmed that concurrent
chemoradiotherapy using weekly nedaplatin (30 mg/m2) is
safe and effective (24). No grade 3
vomiting was observed in the present study, and the total
high-grade GI toxicity was 4.2%, which is considerably lower than
reported in a previous study by Jensen et al (22).
The impact of total length of radiation treatment is
critical for determining OS rate. Walker et al reported that
delays in treatment were predominantly a result of dehydration due
to diarrhea, nausea and vomiting, which may be caused by cisplatin
toxicity and increased small bowel radiation toxicity in the
para-aortic field (25). With the
integrated boost of involved nodes using EF-IMRT, the median
treatment time from the first day of EF-IMRT to the last day of
brachytherapy in the current study was 53 days (range, 48–61 days),
which did not significantly prolong the length of radiation
treatment compared with previous studies of chemoradiotherapy
(7,25). Furthermore, regarding renal toxicity
in patients treated with EFRT (3,5), the
current study did not induce any acute or late renal grade 3 or
higher toxicity. Jensen et al reported 18-month cumulative
incidences of late grade 3 or higher genitourinary and GI toxicity
were 4.8 and 0%, respectively, following EF-IMRT with concurrent
cisplatin chemotherapy (22). RTOG
90–01 reported a late toxicity rate of 12% in patients treated with
EFRT without concurrent chemotherapy (26). In prior studies of EFRT and concurrent
chemotherapy, the reported late toxicity rates were 0–14% (7,27–30). The present study revealed that 2/48
patients (4.2%) developed grade 3 GI late toxicity. The current
results are consistent with reports from these prior studies
(7,27–31).
The delivery of radiation to grossly involved nodes
has been limited due to its toxicity to adjacent organs and tissues
(6). However, IMRT has been shown to
permit delivery of ≤60 Gy to para-aortic and/or pelvic nodes, with
substantially reduced doses to the bowel, bladder and bone marrow
(17,32). In the current study, tumors
metastasized to the para-aortic and/or pelvic nodes were treated
with a total dose of 55–60 Gy in 2.0–2.4 Gy daily fractions using
simultaneous integrated boost-IMRT. Following this treatment, no
recurrence was observed in the para-aortic regions, and no
increased acute or late GI toxicity was observed.
The present study demonstrated that concurrent
treatment with nedaplatin and definitive EF-IMRT was effective in
cervical cancer patients, with a low incidence of high-grade acute
gastrointestinal toxicity. The results also revealed that distant
metastasis was the major cause of mortality; thus, novel treatment
regimens, such as multidrug concurrent chemo/radiotherapy or
immunotherapy with or without radiotherapy, require investigation.
The current study was not a randomized controlled trial and was
limited by the small number of patients. Thus, in order to confirm
the safety and efficacy of this treatment regime on patients with
cervical cancer, further studies are warranted using a larger
sample size and a randomized controlled trial.
Acknowledgements
We thank Medjaden Bioscience Limited (Hong Kong,
China) for editing and proofreading this manuscript.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kumar V, Mitchell RS, Abbas AK and Fausto
N: The female genital system and breast. Robbins Basic Pathology
(8th). Saunders Elsevier. (Philadelphia, PA). 345–355. 2007.
|
|
3
|
Canavan TP and Doshi NR: Cervical cancer.
Am Fam Physician. 61:1369–1376. 2000.PubMed/NCBI
|
|
4
|
Waggoner SE: Cervical cancer. Lancet.
361:2217–2225. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Berman ML, Keys H, Creasman W, DiSaia P,
Bundy B and Blessing J: Survival and patterns of recurrence in
cervical cancer metastatic to periaortic lymph nodes (a Gynecologic
Oncology Group study). Gynecol Oncol. 19:8–16. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Piver MS, Barlow JJ and Krishnamsetty R:
Five-year survival (with no evidence of disease) in patients with
biopsy-confirmed aortic node metastasis from cervical carcinoma. Am
J Obstet Gynecol. 139:575–578. 1981.PubMed/NCBI
|
|
7
|
Varia MA, Bundy BN, Deppe G, Mannel R,
Averette HE, Rose PG and Connelly P: Cervical carcinoma metastatic
to para-aortic nodes: Extended field radiation therapy with
concomitant 5-fluorouracil and cisplatin chemotherapy: A
Gynecologic Oncology Group study. Int J Radiat Oncol Biol Phys.
42:1015–1023. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim YS, Kim JH, Ahn SD, Lee SW, Shin SS,
Nam JH, Kim YT, Kim YM, Kim JH and Choi EK: High-dose
extended-field irradiation and high-dose-rate brachytherapy with
concurrent chemotherapy for cervical cancer with positive
para-aortic lymph nodes. Int J Radiat Oncol Biol Phys.
74:1522–1528. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Grigsby PW, Heydon K, Mutch DG, Kim RY and
Eifel P: Long-term follow-up of RTOG 92-10: Cervical cancer with
positive para-aortic lymph nodes. Int J Radiat Oncol Biol Phys.
51:982–987. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Small W Jr, Winter K, Levenback C, Iyer R,
Gaffney D, Asbell S, Erickson B, Jhingran A and Greven K:
Extended-field irradiation and intracavitary brachytherapy combined
with cisplatin chemotherapy for cervical cancer with positive
para-aortic or high common iliac lymph nodes: Results of ARM 1 of
RTOG 0116. Int J Radiat Oncol Biol Phys. 68:1081–1087. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nugent EK, Case AS, Hoff JT, Zighelboim I,
DeWitt LL, Trinkhaus K, Mutch DG, Thaker PH, Massad LS and Rader
JS: Chemoradiation in locally advanced cervical carcinoma: An
analysis of cisplatin dosing and other clinical prognostic factors.
Gynecol Oncol. 116:438–441. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Carballo N, González-Cortijo L,
González-Martin A, Rojo A and Chiva L: Indications for adjuvant
radiotherapy treatment after surgery and novel modalities for
treatment. Gynecol Oncol. 110(Suppl 2): S41–S44. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Desoize B and Madoulet C: Particular
aspects of platinum compounds used at present in cancer treatment.
Crit Rev Oncol Hematol. 42:317–325. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pecorelli S, Zigliani L and Odicino F:
Revised FIGO staging for carcinoma of the cervix. Int J Gynaecol
Obstet. 105:107–108. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lim K, Small W Jr, Portelance L,
Creutzberg C, Jürgenliemk-Schulz IM, Mundt A, Mell LK, Mayr N,
Viswanathan A, Jhingran A, et al: Consensus guidelines for
delineation of clinical target volume for intensity-modulated
pelvic radiotherapy for the definitive treatment of cervix cancer.
Int J Radiat Oncol Biol Phys. 79:348–355. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Small W Jr, Mell LK, Anderson P,
Creutzberg C, De Los Santos J, Gaffney D, Jhingran A, Portelance L,
Schefter T, Iyer R, et al: Consensus guidelines for delineation of
clinical target volume for intensity-modulated pelvic radiotherapy
in postoperative treatment of endometrial and cervical cancer. Int
J Radiat Oncol Biol Phys. 71:428–434. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cancer Therapy Evaluation Program: Common
Terminology Criteria for Adverse Events. Version 3.0. simplectep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcaev3.pdf#searchAccessed.
December 20–2008
|
|
18
|
Cox JD, Stetz J and Pajak TF: Toxicity
criteria of the Radiation Therapy Oncology Group (RTOG) and the
European Organization for Research and Treatment of Cancer (EORTC).
Int J Radiat Oncol Biol Phys. 31:1341–1346. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Portelance L, Chao KS, Grigsby PW, Bennet
H and Low D: Intensity-modulated radiation therapy (IMRT) reduces
small bowel, rectum, and bladder doses in patients with cervical
cancer receiving pelvic and para-aortic irradiation. Int J Radiat
Oncol Biol Phys. 51:261–266. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gerszten K, Colonello K, Heron DE, Lalonde
RJ, Fitian ID, Comerci JT, Selvaraj RN and Varlotto JM: Feasibility
of concurrent cisplatin and extended field radiation therapy (EFRT)
using intensity-modulated radiotherapy (IMRT) for carcinoma of the
cervix. Gynecol Oncol. 102:182–188. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Salama JK, Mundt AJ, Roeske J and Mehta N:
Preliminary outcome and toxicity report of extended-field,
intensity-modulated radiation therapy for gynecologic malignancies.
Int J Radiat Oncol Biol Phys. 65:1170–1176. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jensen LG, Hasselle MD, Rose BS, Nath SK,
Hasan Y, Scanderbeg DJ, Yashar CM, Mundt AJ and Mell LK: Outcomes
for patients with cervical cancer treated with extended-field
intensity-modulated radiation therapy and concurrent cisplatin. Int
J Gynecol Cancer. 23:119–125. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kodama J, Takemoto M, Seki N, Nakamura K,
Hongo A, Kanazawa S and Hiramatsu Y: Phase I study of weekly
nedaplatin and concurrent pelvic radiotherapy as adjuvant therapy
after radical surgery for cervical cancer. Int J Gynecol Cancer.
18:1037–1041. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Niibe Y, Tsunoda S, Jobo T, Imai M, Matsuo
K, Matsunaga K, Unno N and Hayakawa K: Phase II study of radiation
therapy combined with weekly nedaplatin in locally advanced uterine
cervical carcinoma (LAUCC): Kitasato Gynecologic Radiation Oncology
Group (KGROG 0501)-initial analysis. Eur J Gynaecol Oncol.
29:222–224. 2008.PubMed/NCBI
|
|
25
|
Walker JL, Morrison A, DiSilvestro P and
von Gruenigen VE: Gynecologic Oncology Group: A phase I/II study of
extended field radiation therapy with concomitant paclitaxel and
cisplatin chemotherapy in patients with cervical carcinoma
metastatic to the para-aortic lymph nodes: A Gynecologic Oncology
Group study. Gynecol Oncol. 112:78–84. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Eifel PJ, Winter K, Morris M, Levenback C,
Grigsby PW, Cooper J, Rotman M, Gershenson D and Mutch DG: Pelvic
irradiation with concurrent chemotherapy versus pelvic and
para-aortic irradiation for high-risk cervical cancer: An update of
radiation therapy oncology group trial (RTOG) 90-01. J Clin Oncol.
22:872–880. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sood BM, Gorla GR, Garg M, Anderson PS,
Fields AL, Runowicz CD, Goldberg GL and Vikram B: Extended-field
radiotherapy and high-dose-rate brachytherapy in carcinoma of the
uterine cervix: Clinical experience with and without concomitant
chemotherapy. Cancer. 97:1781–1788. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ring KL, Young JL, Dunlap NE, Andersen WA
and Schneider BF: Extended-field radiation therapy with whole
pelvis radiotherapy and cisplatin chemosensitization in the
treatment of IB2-IIIB cervical carcinoma: A retrospective review.
Am J Obstet Gynecol. 201:109.e1–e6. 2009. View Article : Google Scholar
|
|
29
|
Uno T, Mitsuhashi A, Isobe K, Yamamoto S,
Kawakami H, Ueno N, Usui H, Tate S, Kawata T and Ito H: Concurrent
daily cisplatin and extended-field radiation therapy for carcinoma
of the cervix. Int J Gynecol Cancer. 18:80–84. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chung YL, Jian JJ, Cheng SH, Hsieh CI, Tan
TD, Chang HJ, Hung CF, Horng CF, Soong T and Tsou MH:
Extended-field radiotherapy and high-dose-rate brachytherapy with
concurrent and adjuvant cisplatin-based chemotherapy for locally
advanced cervical cancer: A phase I/II study. Gynecol Oncol.
97:126–135. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Malfetano JH, Keys H, Cunningham MJ,
Gibbons S and Ambros R: Extended field radiation and cisplatin for
stage IIB and IIIB cervical carcinoma. Gynecol Oncol. 67:203–207.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ahmed RS, Kim RY, Duan J, Meleth S, De Los
Santos JF and Fiveash JB: IMRT dose escalation for positive
para-aortic lymph nodes in patients with locally advanced cervical
cancer while reducing dose to bone marrow and other organs at risk.
Int J Radiat Oncol Biol Phys. 60:505–512. 2004. View Article : Google Scholar : PubMed/NCBI
|