Introduction
With the improvement of health conditions, the
incidence of parasitic diseases has been reducing worldwide in
recent decades (1). Pleuropulmonary
paragonimiasis is a food-borne zoonosis commonly caused by the
trematode Paragonimus westermani. The life cycle of P.
westermani involves numerous mammals, including humans
(2). In humans, the adult worms
usually infiltrate the lungs and are found less frequently in other
organs, such as the brain and heart (3). The eggs are expelled from the pulmonary
system through the bronchioles and are expectorated or swallowed
and passed in the feces, eventually reaching freshwater, such as
ponds, streams or rivers, and the next life-cycle is commenced
(4). The typical symptoms include
pleural effusions and pulmonary nodules, with the most notable
clinical features including coughing, blood-tinged sputum and
hemoptysis, distressing chest pain and dyspnea (3). However, this parasitic infection has
other diverse symptoms and may mimic other conditions, such as
tuberculosis infection or neoplasms (5). A range of compounds have been tested for
their efficacy against paragonimiasis. Praziquantel and
triclabendazole are the two World Health Organization-recommended
drugs, and praziquantel is the drug most commonly used in China
(6). The majority of the patients
have a good prognosis. Approximately 50 species of paragonimiasis
have been described worldwide, including 38 species in China, among
which the most predominant infections are P. westermani
(7). Despite this, it is extremely
rare that human paragonimiasis with abdominal wall invasion occurs.
In the present study, the case of a patient that was finally
diagnosed with human paragonimiasis that mimicked chest cancer with
abdominal wall metastasis is reported.
Case report
In March 2014, a 39-year-old emaciated male patient
was admitted to West China Medical Center (Chengdu, Sichuan, China)
with a cough and weight loss of 5 kg in one month. The patient had
no symptoms of fever, night sweats or hemoptysis, but did possess a
history of iodine allergy, mild alcohol use and heavy smoking. The
patient provided written informed consent for the publication of
the present study and the study was approved by the Ethics
Committee of the West China Hospital, Sichuan University (Chengdu,
China).
On examination, the patient demonstrated decreased
breathing sounds in the right lower lung, with pleural rub. A firm
mass in the right upper abdominal wall was palpable with slight
tenderness. Blood tests showed a normal leukocyte count
(6.1×109/l; normal range, 3.5–9.5×109/l) and
eosinophil granulocyte level of 4.2% (normal range, 0–5%), with
normal liver and renal function. Tuberculosis testing was negative.
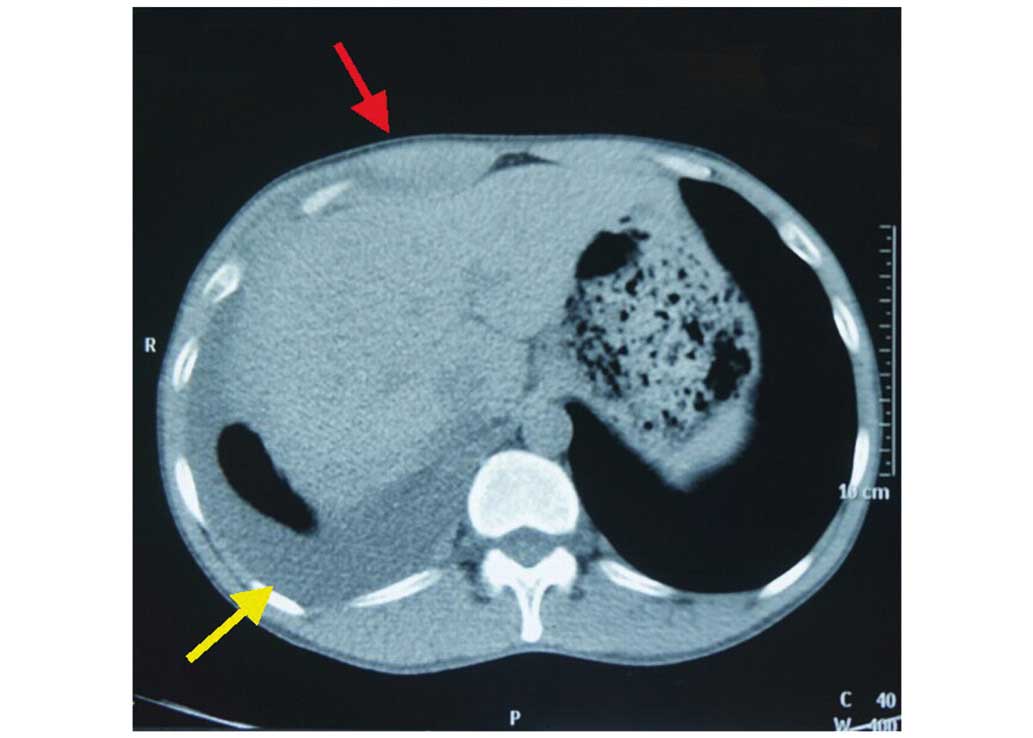
Chest X-ray (Precision Thunis 800+; GE Healthcare, Chalfont, UK)
and 32-slice plain computed tomography (Definition AS; Siemens,
Munich, Germany) of the chest and abdomen showed right pleural
effusion, several nodules in right lower lung and a mass located in
right upper abdominal wall (Fig. 1).
Based on these findings, the patient was initially diagnosed with
lung or pleural carcinoma with abdominal wall metastasis. To
clarify the diagnosis, abdominal wall mass excision was performed
under local anesthesia. Intraoperatively, the mass was identified
as edematous and fragile rectus abdominis, with a greyish section
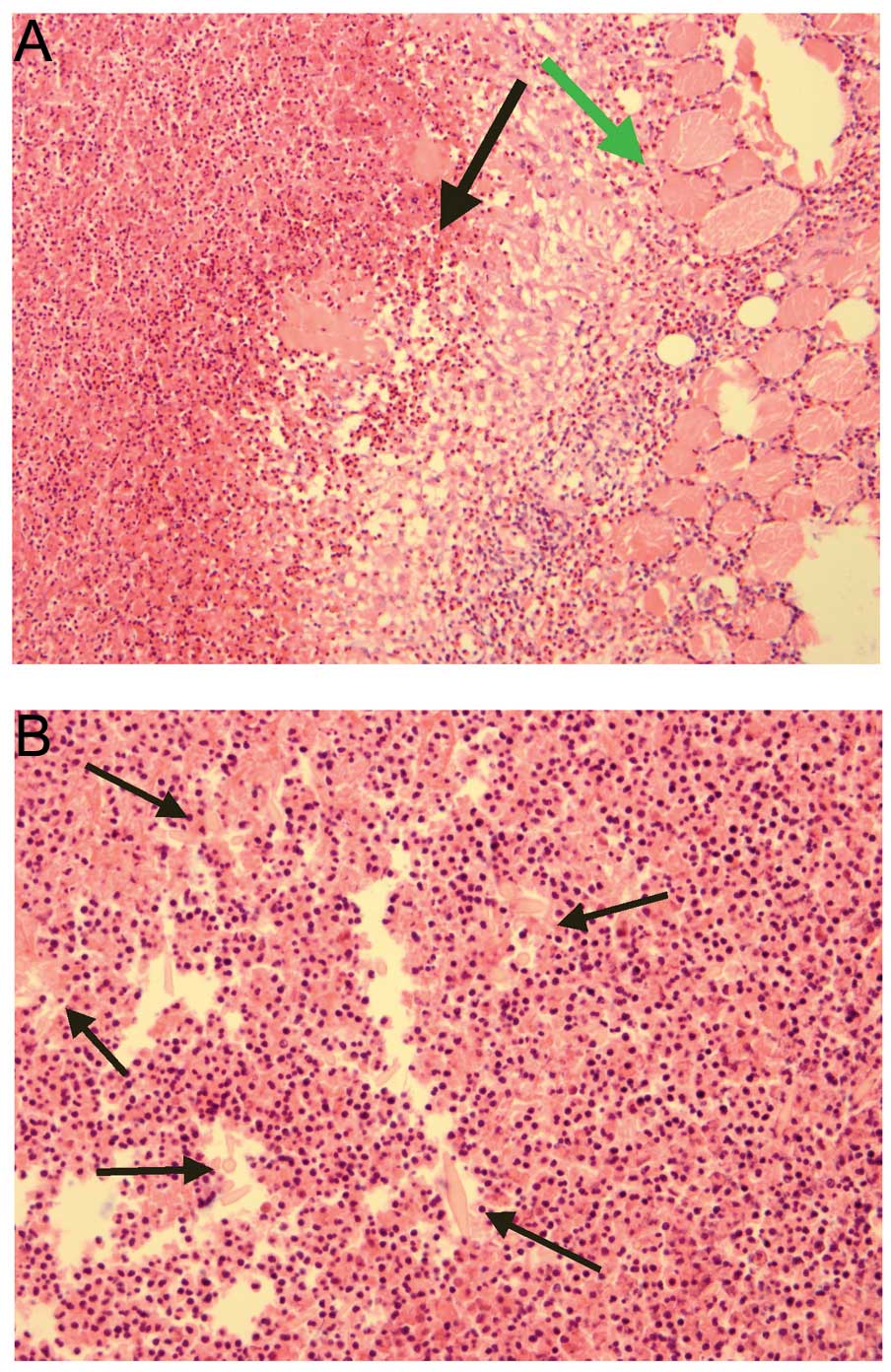
(Fig. 2). Biopsy specimens were sent
to the Department of Pathology (West China Hospital) for
pathological analysis, which revealed that the muscle fibers were
infiltrated by eosinophilic granuloma with the Charcot-Leyden
crystal formation (Fig. 3). The
patient was tested for antibodies against parasites, and the result
revealed the presence of antibodies against P. westermani
immunoglobulin (Ig)G. The patient was diagnosed with P.
westermani infection. Following 1.5 g t.i.d. of oral
praziquantel treatment for 2 days, the pleural effusion disappeared
subsequent to 1 month, and the patient was without recurrence
subsequent to 8 months of follow-up.
Discussion
Only a small number of cases of human paragonimiasis
have been described in the English and Japanese medical literature
since 1984 (8–10). To the best of our knowledge, only two
cases in the Japanese literature have reported a mass in the
abdominal wall, although paragonimiasis may invade the abdominal
wall muscle for a transient time in its life-cycle in humans
(2,3).
When humans ingest pickled or uncooked food containing an infected
crustacean host, such as crabs, crayfish or snails, excystation of
the metacercariae occurs in the small intestine and the
metacercariae penetrate the intestinal wall and enters the
peritoneal cavity, migrate to the diaphragm, pleura and finally
reach the lung (3). The central
nervous system is the most common site of extrathoracic
paragonimiasis (3).
Typical human paragonimiasis demonstrates an
elevated eosinophil count, positive immunoblot, nodular shadows of
the lung and pleural thickening with pleural effusion, and these
symptoms may be confused with tuberculosis or chest cancer
(4). In the present study, the
patient had lung nodules and small amount of pleural effusion with
a normal eosinophil granulocyte level. In addition, due to a mass
in the abdominal wall of the patient and history of weight loss,
the infection was not distinguished from chest cancer and abdominal
wall metastasis. If the patient had possessed cancer with advanced
metastasis, the opportunity for surgery would have been lost and
the patient would receive a poor prognosis (11). To clarify the diagnosis and prepare
for the following treatment, a biopsy of the abdominal wall mass
with surgical resection was performed. Therefore, surgical
intervention is possible in certain cases for the diagnosis and
treatment of paragonimiasis. The biopsy indicated that the patient
suffered from parasite infection, and the final diagnosis and blood
test for P. westermani IgG antibodies were performed.
Corresponding history, antibody tests and biopsy contribute the
convincing evidence for the correct diagnosis (12).
Praziquantel can damage the cortex of parasites and
stimulate muscle tonic contraction, causing spastic paralysis and
death, and is recommended as an orally administered agent at a
total dose of 75–150 mg/kg (13). The
cure rate is 80–90%, with infrequent side effects (14). It should be considered that
insufficient dosage may lead to a worse outcome. Other drugs, such
as mebendazole and bithionol, have been investigated as
experimental chemotherapies for paragonimiasis. Praziquantel is
orally administered at a total dose of 150 mg per kg of body
weight, and is divided into three doses per day for 2 days. The
cure rates reported are 80–90%. Mebendazole plus emetine
hydrochloride shows a cure rate of 70%, while bithionol achieves
only a 50–60% cure rate, and side effects such as urticaria, rash,
abdominal pain, nausea, vomiting, diarrhea and dizziness are common
(15,16). In the present case, the patient
achieved a good recovery subsequent to a course of oral 150 mg/kg
praziquantel treatment, which was divided into three doses per day
for 2 days, and did not experience symptoms of recurrence within 8
months.
The present study emphasizes the requirement for the
consideration of paragonimiasis when a patient presents with lung
nodules and pleural effusion, even without an elevated eosinophil
count. Paragonimiasis may mimic chest cancer and abdominal wall
metastasis. Clinical history, blood antibody and imaging studies
are important to make a correct diagnosis. Biopsy is particularly
important in selected cases to exclude other causes, such as
neoplasm and tuberculosis.
References
|
1
|
Ahn MH: Changing patterns of human
parasitic infection in Korea. Hanyang Med Rev. 30:149–155. 2010.
View Article : Google Scholar
|
|
2
|
Vélez I, Velásquez LE and Vélez ID:
Morphological description and life cycle of Paragonimus sp.
(Trematoda: Troglotrematidae): Causal agent of human paragonimiasis
in Colombia. J Parasitol. 89:749–755. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Liu Q, Wei F, Liu W, Yang S and Zhang X:
Paragonimiasis: An important food-borne zoonosis in China. Trends
Parasitol. 24:318–323. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kagawa FT: Pulmonary paragonimiasis. Semin
Respir Infect. 12:149–158. 1997.PubMed/NCBI
|
|
5
|
Jeon K, Koh WJ, Kim H, Kwon OJ, Kim TS,
Lee KS and Han J: Clinical features of recently diagnosed pulmonary
paragonimiasis in Korea. Chest. 128:1423–1430. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen MG: New developments in the clinical
study of praziquantel. Chin J Parasitol Parasit Dis. 2:193–195.
1984.
|
|
7
|
Zhang ZH: Paragonimiasis. Diseases of
Natural Focus. Tang JQ: Chinese Science Press. (Beijing).
1085–1098. 2005.
|
|
8
|
Akaba T, Takeyama K, Toriyama M, Kubo A,
Mizobuchi R, Yamada T, Tagaya E, Kondo M, Sakai S and Tamaoki J:
Pulmonary paragonimiasis: The detection of a worm migration track
as a diagnostic clue for uncertain eosinophilic pleural effusion.
Intern Med. 55:503–506. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yang X, Xu M, Wu Y and Xiang B: Pancreatic
paragonimiasis mimics pancreatic cystic-solid tumor - A case
report. Pancreatology. 15:576–578. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hoshina T, Tamura K, Kawano S, Kato T,
Sato F, Horino T, Nakazawa Y, Yosikawa K, Yoshida M, Kumagai M and
Hori S: Two cases of Paragonimiasis westermani in a Chinese
family diagnosed with the Ouchterlony double diffusion method.
Kansenshogaku Zasshi. 88:866–870. 2014.(In Japanese). PubMed/NCBI
|
|
11
|
Bagcchi S: Use of chemotherapy in patients
with metastatic lung cancer. Lancet Oncol. 16:e2632015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Castilla EA, Jessen R, Sheck DN and Procop
GW: Cavitary mass lesion and recurrent pneumothoraces due to
Paragonimus kellicotti infection: North American
paragonimiasis. Am J Surg Pathol. 27:1157–1160. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Johnson RJ, Jong EC, Dunning SB, Carberry
WL and Minshew BH: Paragonimiasis: Diagnosis and the use of
praziquantel in treatment. Rev Infect Dis. 7:200–206. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Drugs for Parasitic Infections (2nd). The
Medical Letter, Inc. New Rochelle, NY: 1–20. 2010.
|
|
15
|
Benjapong W, Naeypatimanond S, Benjapong
K, Thumaruksa C, Ruttarasarn S and Jaroonvesama N: Studies on
paragonimiasis: Treatment with mebendazole, emetine with
mebendazole and praziquantel. Southeast Asian J Trop Med Public
Health. 15:354–359. 1984.PubMed/NCBI
|
|
16
|
Chen MG, Chang ZS, Shao XY, Liu MD, Blair
D, Chen SH, Zhang YN, Hong JL, Shen BG and Feng Z: Paragonimiasis
in Yongjia County, Zhejiang Province, China: Clinical,
parasitological and karyotypic studies on Paragonimus
westermani. Southeast Asian J Trop Med Public Health.
32:760–769. 2001.PubMed/NCBI
|