Introduction
Central neurocytomas (CNCs) are rare brain tumors
that originate from neuroepithelial tissue, occurring most
frequently in young adults, and are often located in the lateral
ventricles. CNC was first described by Hassoun et al
(1) in 1982, and accounts for
0.1–0.5% of all primary brain tumors (2). Complete surgical resection is currently
the optimal treatment choice, and the prognosis of CNC is often
favorable due to its benign nature (3). Although CNC typically occurs in the
lateral ventricles, a few cases of CNC occurring in
extraventricular regions have been reported in the literature.
Case report
In March 2014, a 49-year-old man was admitted to the
Tsinghua University Yuquan Hospital (Beijing, China) after
experiencing headaches for 3 weeks. No other focal neurological
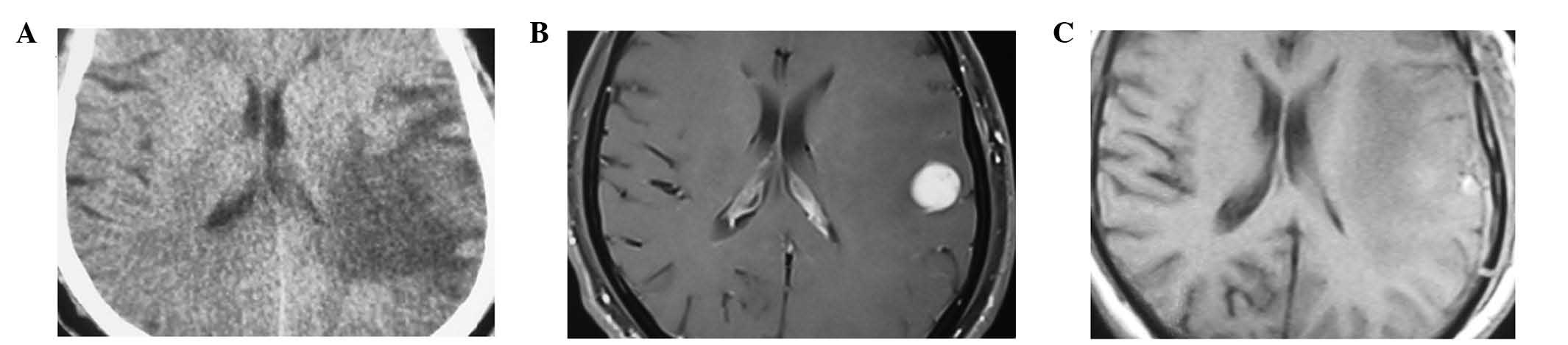
deficits were observed upon admission. Computed tomography (CT;
SOMATOM Sensation 16; Siemens AG, Munich, Germany) of the brain
identified an isodense, round, well-demarcated, 3.3-cm tumor, which
was located in the left temporal lobe, in addition to peritumoral
edema (Fig. 1A). Marked homogeneous
enhancement was observed within the mass on T1-gadolinium imaging
(Fig. 1B). The patient underwent
surgery, and the tumor was excised via a left temporal craniotomy.
As there was no adhesion between the tumor and the dura or the
brain, the radical resection of the lesion was straightforward. The
pathological report stated that the tumor was a grade II
extraventricular neurocytoma (EVN) according to the World Health
Organization (WHO) classification of tumors of the central nervous
system (4). Resected tissue specimens
were formalin (Yuekai Trading Co., Ltd., Hebei, China)-fixed,
paraffin (Sinopharm Chemical Reagent Co., Ltd., Shanghai,
China)-embedded, cut into 8-µm sections, stained with hematoxylin
and eosin (Shanghai Qianchen Biotechnologies, Co., Ltd., Shanghai,
China) and visualized using an optical microscope (CX23; Olympus
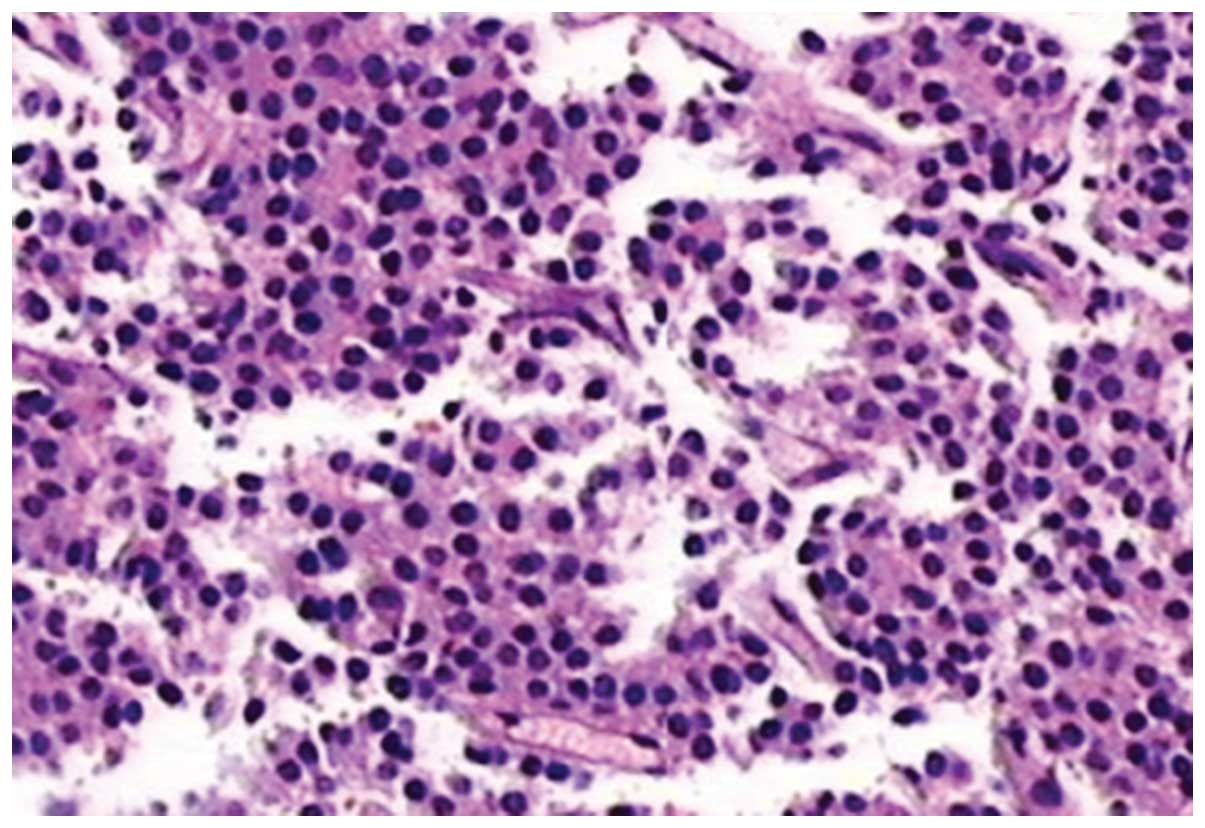
Corporation, Tokyo, Japan). Histologically, the resected tumor
tissue contained clusters of small cells with regular nuclear
morphology, and round nuclei with fine chromatin (Fig. 2). Vascular hyperplasia was also
observed. There was no evidence of ischemic necrosis or hemorrhage.
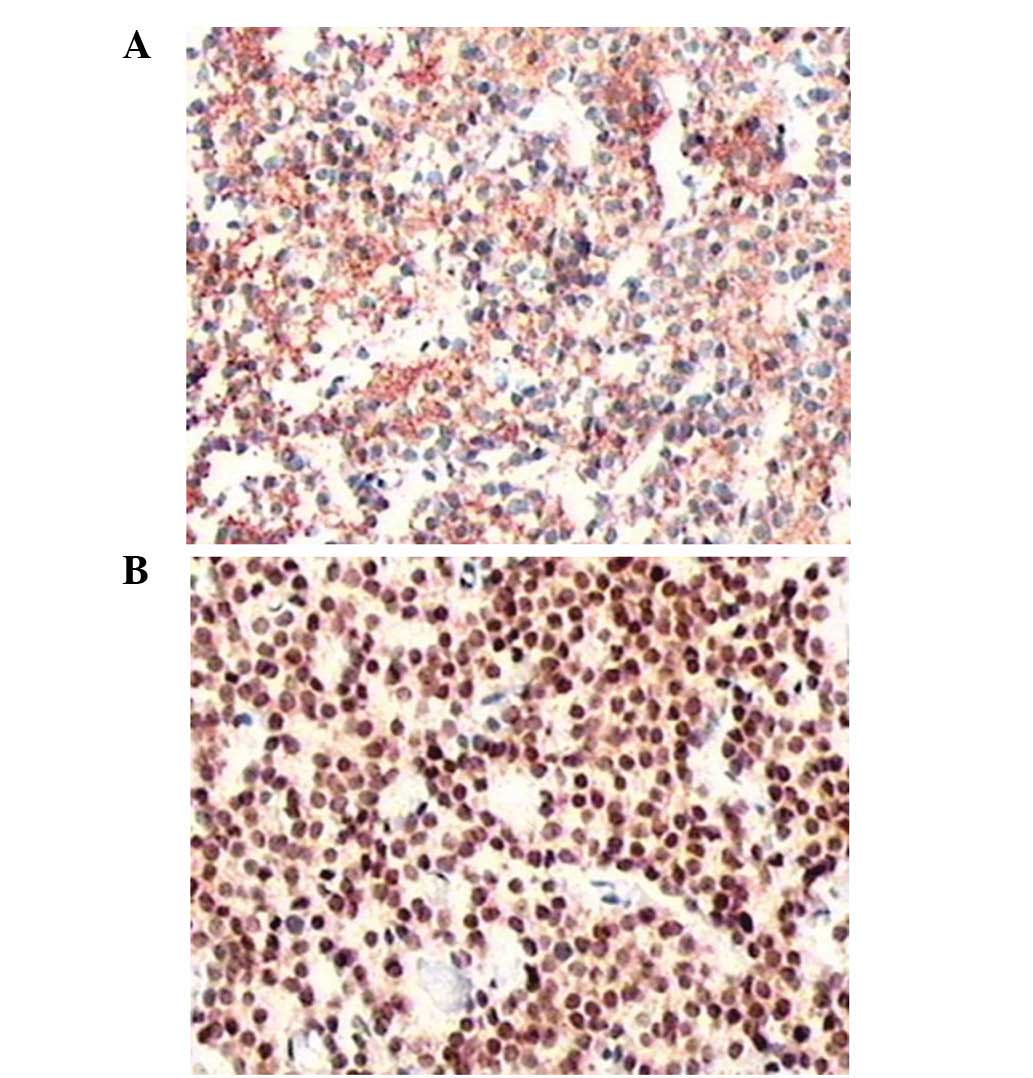
For immunohistochemical staining, tissue sections were incubated
with monoclonal mouse anti-rat synaptophysin (cat. no. ab11105;
1:500; Abcam, Cambridge, MA, USA), rabbit anti-mouse neuronal
nuclear antigen (cat. no. ab190565; 1:50; Abcam) and mouse
anti-human Ki67 (cat. no. ab8191; 1:50; Abcam) antibodies overnight
at 4°C. The sections were then washed with PBS, incubated with
biotinylated goat anti-mouse (cat. no. ab97233; 1:300; Abcam) or
goat anti-rabbit (cat. no. ab97188; 1:300; Abcam) secondary
antibodies for 30 min and staining was visualized using an optical
microscope (CX23; Olympus Corporation). Immunohistochemical
staining revealed that the tumor cells expressed the neuronal
differentiation markers, synaptophysin and neuronal nuclear antigen
(Fig. 3). Ki-67, a marker for
proliferation index, was detected in 10% of the tumor nuclei. The
patient was discharged from hospital without further treatment,
including radiotherapy or chemotherapy. The patient was followed up
for 3 months post-surgery, with magnetic resonance imaging (MRI;
Signa HDe 1.5T; GE Healthcare Bio-Sciences, Pittsburgh, PA, USA) of
the brain demonstrating no evidence of tumor recurrence (Fig. 1C). After the initial 3 month follow-up
period, the patient was followed-up every 6 months, and at the time
of writing no recurrence had been identified.
Discussion
CNC is most prevalent in adolescents and young
adults, and is often located in the lateral ventricles. In 1997,
Giangaspero et al (5) reported
the first case of a tumor that mimicked CNC, but was located in an
extraventricular region. In 2007, these tumors were classified by
the WHO as a novel brain tumor entity (4), and the incidence of EVN remains
extremely rare, with Liu et al (6) reporting a worldwide incidence of only
0.13%. The development of CNC appears to have no significant gender
predilection; however, the literature indicates that EVN has a
slight female predominance and a median patient age of 38 years
(range, 5–76 years) (7,8).
Increased intracranial pressure is the most common
clinical presentation, particularly for CNC of the lateral
ventricles. Other symptoms may vary from seizure to gait
disturbances depending on the tumor location. The most frequent
symptom of EVN is complex partial seizure, followed by headaches,
precocious puberty, cranial nerve paralysis, and on rare occasions,
hemorrhage (9). Various other
non-specific symptoms are also associated with the disease,
including headache, dizziness, weakness, and memory and
consciousness dysfunction (10). A
large number of patients present with these non-specific symptoms,
and thus there are no definitive symptoms to diagnose EVN.
EVNs do not present with specific imaging
characteristics. On imaging analysis, EVNs may appear as
well-circumscribed, round or multilobular, hypodense or isodense
masses, which are homogeneously-enhanced with contrast medium, as
observed in the present case. Liu et al (6) reported that cystic degeneration was
observed in 6 out of 9 (66%) EVN cases, with calcification in 34%
and perilesional edema in 44%, whilst Patil et al (11) reported that cystic degeneration was
present in 71% of 9 cases and perifocal edema in 57%. MRI may
exhibit an isointense or slightly hyperintense signal compared with
the cortex on T1- and T2-weighted images. The majority of EVN
tumors are solid, but largely cystic masses, and mural nodules may
be identified. Moderate enhancement is typically observed in these
tumors, however, following administration of a contrast agent, mild
to strong heterogeneous enhancement may be exhibited (12–14).
Common differential diagnoses include oligodendroglioma, ependymoma
and dysembryoplastic neuroepithelial tumors, all of which usually
lack a clear margin. Contrast enhancement and cystic changes also
assist in distinguishing EVNs from other lesions. MR spectroscopy
studies of EVNs have demonstrated a prominent choline peak with a
notably decreased or absent N-acetylaspartate peak when compared
with intraventricular neurocytomas (15).
A characteristic histological feature of EVNs is
their composition of monotonous neoplastic cells with round,
regular nuclei embedded in a matrix of fine neuronal processes,
known as a neuropils. These neuropils are much finer than glial
processes and exhibit a ‘velvety’ appearance, assisting their
differentiation from typical rosettes observed in an ependymoma
(16). Atypical EVNs are
characterized immunohistochemically by a Ki-67 index of >2%, or
by atypical histological features, including increased mitotic
activity, focal necrosis and vascular proliferation (17). Histologically, EVN may also resemble
oligodendroglioma, therefore, immunochemistry is required to a make
an accurate diagnosis. Oligodendrogliomas may exhibit a limited
amount of synaptophysin positivity in the tumor cell cytoplasm, but
not to the same degree or extent as EVNs (18,19). EVNs
may also occasionally carry the 1p19q codeletion, which is observed
in 50–80% of oligodendroglioma cases (19).
Complete surgical excision is currently considered
as the optimal treatment for EVN, but is often limited by tumor
proximity to eloquent areas (20). In
cases of incomplete resection, available data suggests that
radiotherapy offers the same tumor control rates for EVN (11). The success rate of Gamma
Knife® radiosurgery has not yet been discussed in the
literature due to the limited number of EVN cases.
Post-operative radiation therapy may be effective in
reducing tumor size and recurrence rates in cases of aggressive
atypical neurocytoma; the recommended dose of 50 Gy is considered
to be the most appropriate for long-term local control in children
(20). Additional Gamma Knife
stereotactic radiosurgery may be performed post-surgery in order to
obtain improved local control and a higher survival rate for cases
that cannot be surgically resected (7). The potential benefits of chemotherapy
for recurrent tumors and residual lesions is uncertain and is not
currently supported in the literature.
In the present case, complete surgical resection was
performed due to the clear boundary of the tumor. Further treatment
was not necessary, and the patient was followed-up 3 months
post-surgery, with MRI of the brain indicating no signs of
recurrence.
EVNs are benign in nature, with the exception of
aggressive atypical variants (21).
There is no association between tumor recurrence and tumor
location, and pathology is one important prognostic factor.
Atypical EVNs are characterized by a Ki-67 proliferation index of
>2% or by atypical histological features, including vascular
proliferation, focal necrosis and increased mitotic activity. As a
result of these features, atypical EVN is difficult to resect
completely. Kane et al (22)
reported that a typical EVN histology significantly predicts a poor
outcome with higher recurrence and mortality rates. Age is an
additional prognostic factor, with an age of >50 years serving
as a risk factor for recurrence, and an age of <18 years often
associated with atypical features (16).
In conclusion, EVN is extremely rare and presents
with varying clinical symptoms and imaging characteristics. The
current case described a 49-year-old patient with EVN and discussed
the associated clinical presentation, radiological manifestation
and histopathological features. Total surgical resection of the
tumor was considered as the optimal treatment. However,
post-operative radiation therapy may be an effective therapeutic
supplement for cases of incomplete resection. In addition,
long-term follow-up is essential for cases of atypical EVN.
References
|
1
|
Hassoun J, Gambarelli D, Grisoli F, Pellet
W, Salamon G, Pellissier JF and Toga M: Central neurocytoma. An
electron-microscopic study of two cases. Acta Neuropathol.
56:151–156. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sharma MC, Deb P, Sharma S and Sarkar C:
Neurocytoma: A comprehensive review. Neurosurg Rev. 29:270–285.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Patel DM, Schmidt RF and Liu JK: Update on
the diagnosis, pathogenesis, and treatment strategies for central
neurocytoma. J Clin Neurosci. 20:1193–1199. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Louis DN, Ohgaki H, Wiestler OD, Cavenee
WK, Burger PC, Jouvet A, Scheithauer BW and Kleihues P: The 2007
WHO classification of tumours of the central nervous system. Acta
Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Giangaspero F, Cenacchi G, Losi L,
Cerasoli S, Bisceglia M and Burger PC: Extraventricular neoplasms
with neurocytoma features. A clinicopathological study of 11 cases.
Am J Surg Pathol. 21:206–212. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu K, Wen G, Lv XF, Deng YJ, Deng YJ, Hou
GQ, Zhang XL, Han LJ and Ding JL: MR imaging of cerebral
extraventricular neurocytoma: A report of 9 cases. AJNR Am J
Neuroradiol. 34:541–546. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Choi H, Park SH, Kim DG and Paek SH:
Atypical extraventricular neurocytoma. J Korean Neurosurg Soc.
50:381–384. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Choudhari KA, Kaliaperumal C, Jain A,
Sarkar C, Soo MY, Rades D and Singh J: Central neurocytoma: A
multi-disciplinary review. Br J Neurosurg. 23:585–595. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Taylor CL, Cohen ML and Cohen AR:
Neurocytoma presenting with intraparenchymal cerebral hemorrhage.
Pediatr Neurosurg. 29:92–95. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hassoun J, Soylemezoglu F, Gambarelli D,
Figarella-Branger D, von Ammon K and Kleihues P: Central
neurocytoma: A synopsis of clinical and histological features.
Brain Pathol. 3:297–306. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Patil AS, Menon G, Easwer HV and Nair S:
Extraventricular neurocytoma, a comprehensive review. Acta
Neurochir (Wien). 156:349–354. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen H, Zhou R, Liu J and Tang J: Central
neurocytoma. J Clin Neurosci. 19:849–853. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jaiswal S, Vij M, Rajput D, Mehrotra A,
Jaiswal AK, Srivastava AK, Behari S and Krishnani N: A
clinicopathological, immunohistochemical and neuroradiological
study of eight patients with central neurocytoma. J Clin Neurosci.
18:334–339. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yang GF, Wu SY, Zhang LJ, Lu GM, Tian W
and Shah K: Imaging findings of extraventricular neurocytoma:
Report of 3 cases and review of the literature. AJNR Am J
Neuroradiol. 30:581–585. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ueda F, Suzuki M, Matsui O and Uchiyama N:
Automated MR spectroscopy of intra- and extraventricular
neurocytomas. Magn Reson Med Sci. 6:75–81. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Brat DJ, Scheithauer BW, Eberhart CG and
Burger PC: Extraventricular neurocytomas: Pathologic features and
clinical outcome. Am J Surg Pathol. 25:1252–1260. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rades D, Fehlauer F and Schild SE:
Treatment of atypical neurocytomas. Cancer. 100:814–817. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mut M, Güler-Tezel G, Lopes MB, Bilginer
B, Ziyal I and Ozcan OE: Challenging diagnosis: Oligodendroglioma
versus extraventricular neurocytoma. Clin Neuropathol. 24:225–229.
2005.PubMed/NCBI
|
|
19
|
Perry A, Scheithauer BW, Macaulay RJ,
Raffel C, Roth KA and Kros JM: Oligodendrogliomas with neurocytic
differentiation. A report of 4 cases with diagnostic and
histogenetic implications. J Neuropathol Exp Neurol. 61:947–955.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rades D, Schild SE and Fehlauer F:
Defining the best available treatment for neurocytomas in children.
Cancer. 101:2629–2632. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rades D, Schild SE and Fehlauer F:
Prognostic value of the MIB-1 labeling index for central
neurocytomas. Neurology. 62:987–989. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kane AJ, Sughrue ME, Rutkowski MJ, Aranda
D, Mills SA, Lehil M, Fang S and Parsa AT: Atypia predicting
prognosis for intracranial extraventricular neurocytomas. J
Neurosurg. 116:349–354. 2012. View Article : Google Scholar : PubMed/NCBI
|