Introduction
The typical course of ovarian metastasis is
intraabdominal spread manifesting as peritoneal carcinomatosis. In
addition, malignant pleural effusions are observed in ~10% of women
diagnosed with ovarian cancer (1). In
contrast, metastatic lesions of the breast from an extramammary
origin are rare events and account for 0.3% of malignant breast
tumors (1). Metastatic lesions of the
breast from an extramammary origin are rare events and account for
0.3% of malignant breast tumors (1).
Metastatic lesions of the breast have a diverse appearance and
tumor characteristics vary according to the site of the primary
tumor. According to a Pubmed search performed in February 2015,
using the search terms ‘breast metastasis’, ‘ovarian cancer’,
‘non-mammary breast metastasis’ and ‘intramammary metastasis’, 110
cases of metastasis of ovarian cancer to the breast (MOCB) have
been reported in the literature. A study by Abbas et al
described ultrasonographic and mammographic features in a series of
280 women with intramammary metastases, 41 of which were diagnosed
with MOCB (2). In the study,
intramammary masses and architectural distortion were the two main
radiological patterns exhibited by the metastases. The masses also
typically exhibited microlobulated margins and posterior
enhancement on ultrasound. In a similar study, DeLair et al
analyzed 85 cases of non-mammary metastases to the breast and
axilla, 14 of which were MOCB (3).
Notably, the ovaries was the predominant site of origin among all
carcinomas causing metastases to the breast, comprising 58% of all
cases. Morphologically, the majority of cases presented as a
solitary nodule with noteworthy recurrent histological findings,
including a metastatic lesion with a fibrous pseudocapsule and
well-circumscribed growth pattern, and the lack of in situ
carcinoma. The survival time was generally poor and 96% of patients
succumbed to the disease, with a median overall survival time of 15
months post-diagnosis.
Karam et al investigated 29 ovarian cancer
patients with malignant breast lesions, 10 of whom exhibited MOCB
and 19 of whom presented with primary breast cancer (4). The study found marked differences
between the two groups regarding disease-free survival time and the
mean time interval between the diagnosis of ovarian cancer and the
diagnosis of the breast tumor. Each time was significantly shorter
for MOCB. The breast tumors of patients with MOCB were also less
likely to be diagnosed on mammogram and the patients were less
likely to have a family history of breast cancer. Overall survival
time was significantly shorter for women with MOCB.
Another series of women with MOCB comprised 18 cases
from a 14-year period (5). In this
series, serous papillary carcinoma was the most common histological
type of MOCB. Of the 18 patients, 4 presented with multiple breast
lesions and 8 with a single metastasis, while 6 patients only
exhibited involvement of the axillary lymph nodes. In 17/18 cases,
the metastases exhibited papillary features, with psammoma bodies
present in 4 cases. Immunoperoxidase studies showed positivity for
Wilm's tumor (WT)-1 and negativity for prolactin-induced protein
(GCDFP-15) in all cases.
Dursun et al reported 9 cases of bilateral
MOCB (6). In this series, the mean
survival time was 12 months. Smaller series of MOCB have also
described 5 (7), 4 (1), 3 (8), 2
(9), 1 (10), 1 (11),
1 (12), and 1 (13) cases, respectively.
Histologically, the basis to the diagnosis of MOCB
is that the papillary architecture consistent with serous papillary
carcinoma is not a typical pattern of the majority of histological
types of invasive breast carcinoma. Serous papillary carcinoma may
resemble invasive micropapillary breast carcinoma and
calcifications are observable in the two entities (1). In addition to histology,
immunohistochemistry is frequently used to discern MOCB from other
extramammary breast metastases and primary breast cancers. For
example, the expression of WT-1, paired box 8 (PAX8) and mesothelin
have been described as being useful in this regard (1–3).
The present study describes two cases of women with
recurrent ovarian cancer and MOCB, and discusses the clinical and
histological characteristics, and management of these patients.
Case report
Case 1
A 52-year-old woman, who was first diagnosed with
recurrent ovarian cancer in April 2011, presented to the Department
of Obstetrics and Gynecology, Ruhr University (Bochum, Germany) in
June 2014 with a localized, palpable, painful mass in the upper
outer quadrant of the right breast. The patient had no family
history of breast cancer and no history of a previous breast
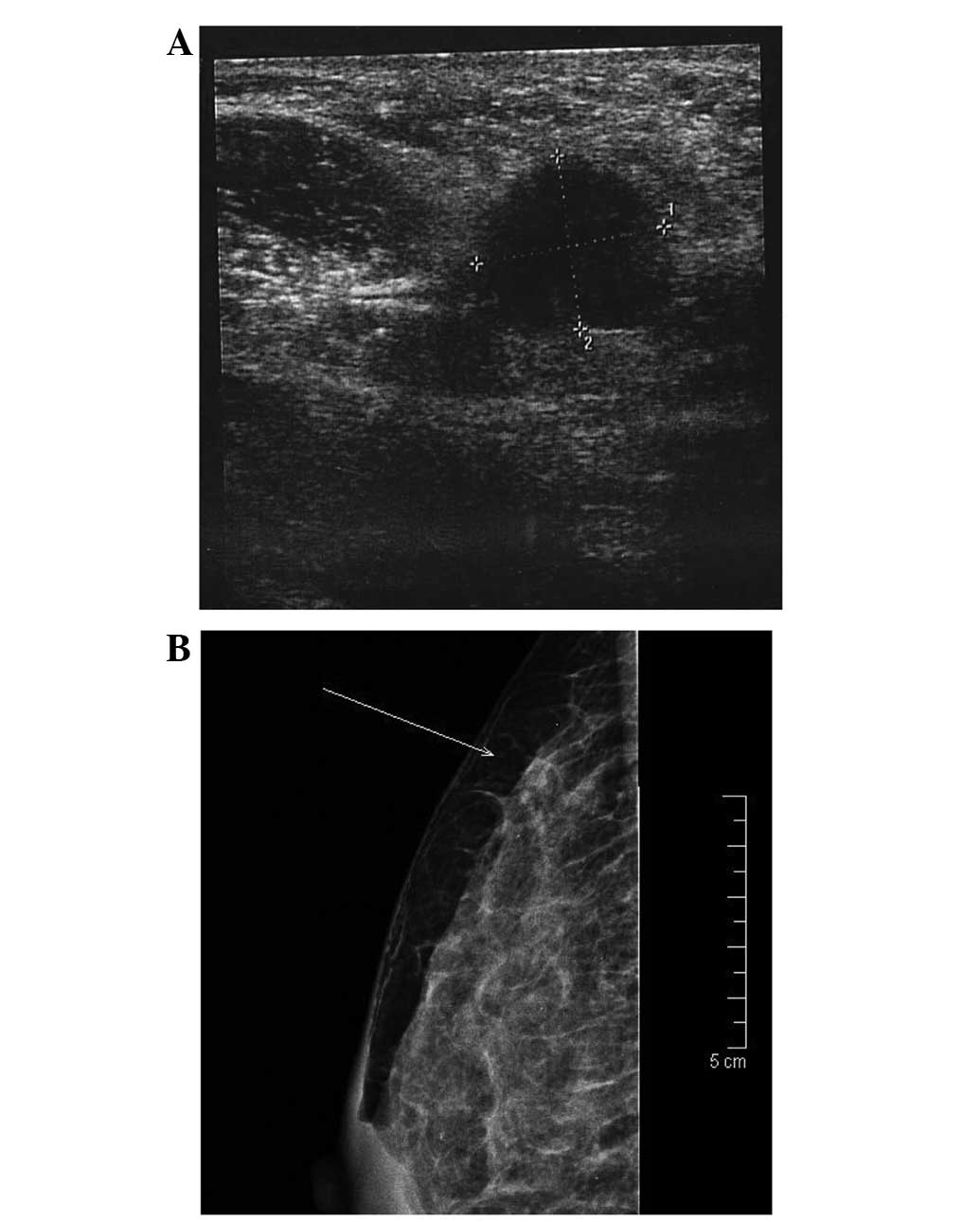
pathology. Breast sonography and mammography revealed a singular,
round, homogenous tumor with a well-defined border (Fig. 1). A singular, enlarged axillary lymph
node was palpable. On mammography, the tumor presented as a loose,
dense area with monomorphous calcifications, without clear borders
(Fig. 1). The tumor was 0.5×0.8 cm in
size. A vacuum jet biopsy (Histocore® Automatic Biopsy
system; BIP GmbH, Tuerkenfeld, Germany) was performed and the
histology showed an undifferentiated adenocarcinoma of unknown
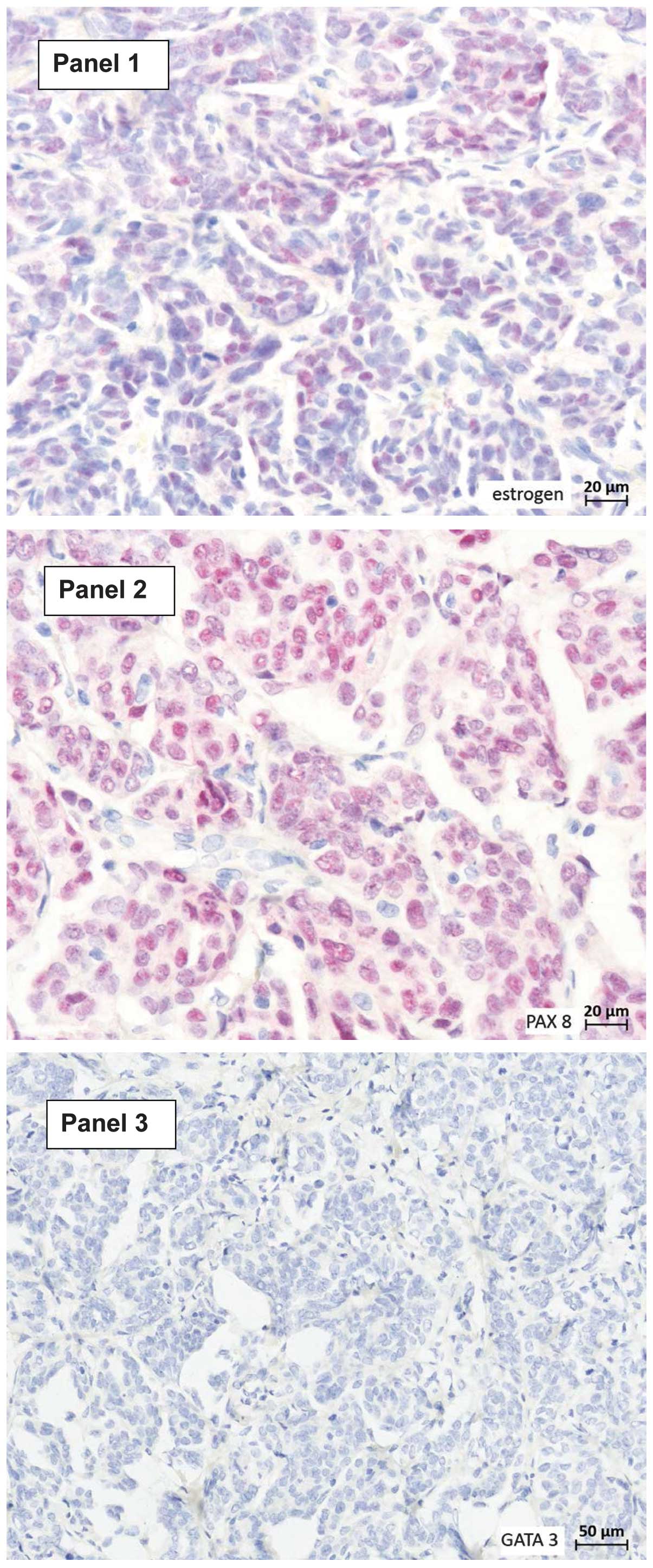
origin. Immunohistochemically, the tumor cells expressed estrogen
receptor (ER) and PAX8 and were negative for GATA binding protein 3
(GATA3) (Fig. 2). A lumpectomy was
performed and the final histology confirmed a diagnosis of MOCB.
The post-operative course of the disease was uneventful and the
patient continued with ovarian cancer-specific chemotherapy, i.e.,
two cycles of topotecan 1.5 mg/m2 by intravenous
infusion on days 1–5 of a 21-day course. The patient succumbed to
disease progression 2 months after breast surgery.
Case 2
A 51-year-old woman, who was first diagnosed with
recurrent ovarian cancer in October 2013, presented to the
Department of Obstetrics and Gynecology, Ruhr University in January
2014 with a centrally localized, palpable, painful mass in the left
breast. The patient had no family history of breast cancer and no
history of previous breast pathology. Breast sonography revealed a
singular, lobulated, inhomogenous tumor with an irregular border.
No enlarged axillary lymph nodes were palpable. On mammography, the
tumor presented as a central, dense area without clear borders and
with monomorphous, ring-shaped calcifications. The tumor was 8×7.5
cm in size. A vacuum jet biopsy (Histocore Automatic Biopsy system;
BIP GmbH) was performed and the histology showed a
moderately-differentiated adenocarcinoma that was suspected of
being a primary breast cancer. A mastectomy and ipsilateral
axillary sentinel node resection were performed. The final
histology revealed a diagnosis of MOCB and confirmed the ovarian
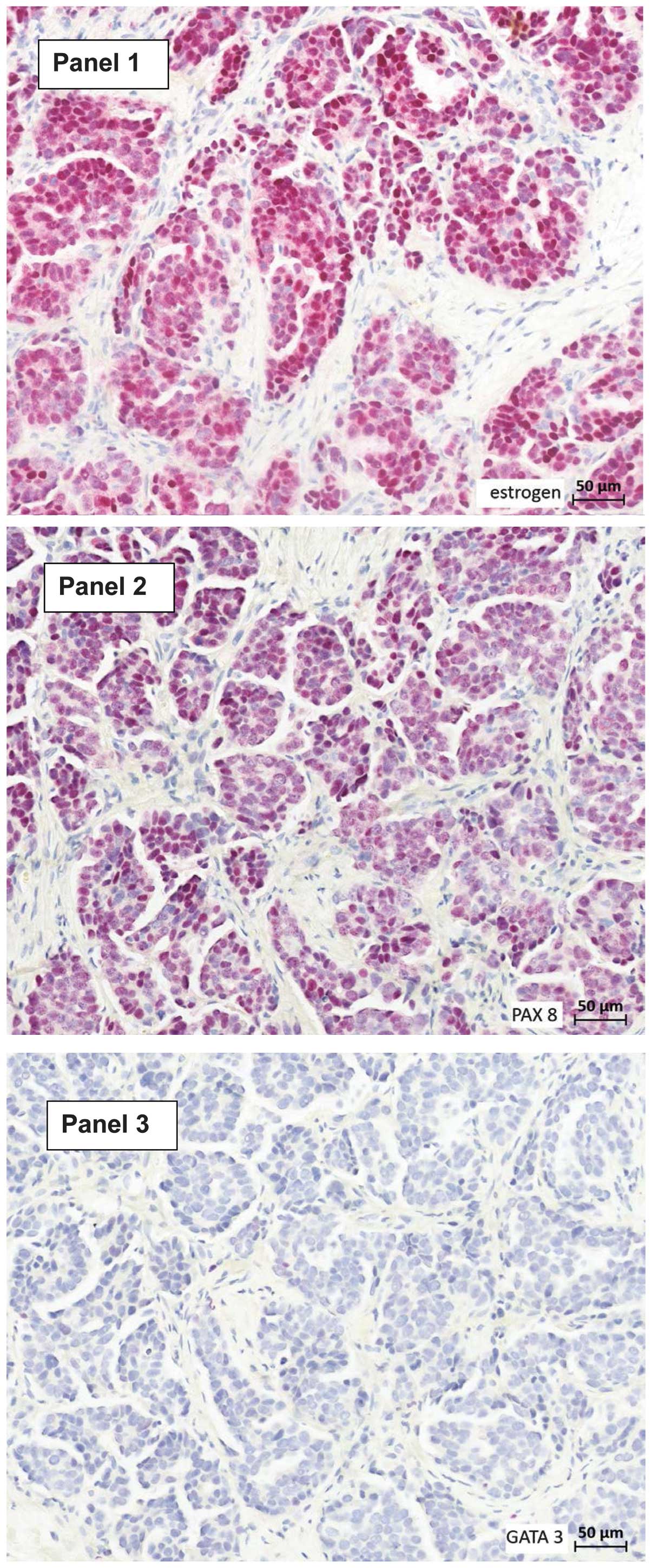
origin of the lesion. Immunohistochemically, the tumor cells
expressed ER and PAX8, and were negative for GATA3 (Fig. 3). The post-operative course of the
disease was uneventful and the patient continued with ovarian
cancer-specific chemotherapy, i.e., six cycles of liposomal
doxorubicin 50 mg/m2 by intravenous infusion on day 1 of
a 28-day course. After the 6 cycles, the patient was lost to
follow-up.
Discussion
The present study describes two cases of MOCB in
women with recurrent ovarian cancer presenting as a solitary,
painful breast mass. Breast sonography and mammography showed a
singular, round, homogenous tumor with irregular borders in each
case. Tumor biopsy revealed an undifferentiated adenocarcinoma of
unknown origin in one case and a moderately-differentiated
adenocarcinoma suspected of being breast cancer in the other case.
The tumor cells were positive for ER and PAX8, and negative for
GATA3 in the two cases. Lumpectomy was performed in one case and
mastectomy with ipsilateral axillary sentinel node biopsy in the
other case. The final histology revealed MOCB in each case. One
patient succumbed to disease progression 2 months after breast
surgery. The other patient remains alive and is currently
undergoing systemic chemotherapy.
MOCB is a rare manifestation of recurrent ovarian
cancer, with 110 cases reported in the literature (1–13). The
typical morphological features of MOCB include a localized, painful
mass with microlobulated margins and posterior enhancement on
ultrasound (2) and a
well-circumscribed growth pattern surrounded by a fibrous
pseudocapsule, with notable absence of an in situ carcinoma
(3). Local palliative surgical
resection with free margins is the primary treatment of choice, and
is consistently described in the literature (3–13).
Although the local resection of the breast lesion does not
positively affect the prognosis, it appears to be important to have
an adequate specimen in order to establish the diagnosis of MOCB.
This is difficult per se and even more so on a biopsy specimen
only. Notably, in one of the present cases, the jet biopsy specimen
was initially misdiagnosed as an undifferentiated adenocarcinoma of
the breast. Bernadi et al (14) found that the status of resection
margins and the management of infiltrated or narrow margins exerted
no significant influence on local tumor recurrence rates or on
overall patient survival. Instead, biological factors connected
with tumor aggressiveness seem to play the most important role in
breast cancer prognosis, independent of surgical radicality. The
most important differential diagnoses of MOCB are primary breast
cancer and extramammary metastases from a malignant tumor other
than ovarian cancer. The unequivocal establishment of the diagnosis
of MOCB is important, as primary breast cancer and extramammary
metastases from a malignant tumor other than ovarian cancer require
different therapies. The prognosis of MOCB has been described as
poor, mostly reflecting the late stage of ovarian cancer
progression (3–5). In one series, for example, >90% of
patients succumbed, with a median survival time of 15 months after
diagnosis (3). This is consistent
with the present study, in which one patient succumbed 2 months
after the diagnosis of MOCB and the other patient was alive after a
short follow-up of 3 months. In a series of 169 patients with
confirmed metastases to the breast from non-breast solid organ
primary tumors at the University of Texas M. D. Anderson Cancer
Center, Williams et al (13)
found that the median survival time from the diagnosis of breast
metastasis was 10 months. On univariate analysis, a significantly
higher survival rate was observed in patients who underwent
surgical resection for breast metastases. On multivariate analysis,
those individuals who did not undergo surgery were 88% more likely
to succumb than those who underwent surgery (13). These data support the use of local
surgery for the management of MOCB.
Histological classification of extramammary breast
metastases and the differentiation from primary breast cancers is
challenging, and is based on a combination of morphological and
immunohistochemical features. For example, mammary and non-mucinous
ovarian carcinomas are usually positive for cytokeratin 7, often
positive for ER and typically negative for cytokeratin 20. The
epithelial membrane antigen expression pattern is typical for
serous papillary carcinoma, with expression on the outside of the
papillary clusters and around the central spaces (1). The expression of WT-1 in the nuclei of
cells occurs in ~70% of ovarian carcinomas and in 95% of serous
papillary carcinomas; however, <10% of breast cancers exhibit
this expression (15–18). GCDFP-15 expression is rarely observed
in ovarian carcinoma (1,19,20),
whereas staining for cancer antigen (CA)125 is present in ~60% and
90% of ovarian and serous papillary carcinomas, respectively
(1). CA125 expression is also
normally observed in endocervical, endometrial, pancreatic and
biliary carcinomas, but is less typically present in breast cancer
(1,21,22).
Another immunohistochemical marker is mesothelin, which is
expressed in >90% of serous papillary carcinomas of the ovary,
but is weakly expressed in 3–14% of breast cancer cases (1,23–25). Lung, colorectal and gastric
adenocarcinomas present with intermediate levels of staining.
The present study describes two cases of MOCB in
women with recurrent ovarian cancer presenting as a solitary,
painful breast mass. The lesions were positive for ER and PAX8, and
negative for GATA3. Management consisted of local surgical
resection without further treatment. In the literature, the
prognosis of MOCB has been described as poor, which is attributed
to the fact that MOCB represents a late stage of ovarian cancer
progression. The histological diagnosis of MOCB is difficult and
MOCB may be misdiagnosed as primary breast cancer. A number of
immunohistochemical markers have been described as useful in the
differential diagnosis of MOCB, including ER, PAX8, GATA3, CA125,
WT-1, GCDFP-15 and mesothelin.
The case studies and literature review presented in
this study add to the literature on MOCB characterizing this tumor
as a late stage manifestation of ovarian cancer with a poor
prognosis. Future clinical studies on MOCB should concentrate on
conservative treatment and comprehensive histopathological
diagnosis based on biopsy specimens with the goal of avoiding local
surgery.’
References
|
1.
|
Lee AH: The histological diagnosis of
metastases to the breast from extramammary malignancies. J Clin
Pathol. 60:1333–1341. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Abbas J, Wienke A, Spielmann RP, Bach AG
and Surov A: Intramammary metastases: Comparison of mammographic
and ultrasound features. Eur J Radiol. 82:1423–1430. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
DeLair DF, Corben AD, Catalano JP, Vallejo
CE, Brogi E and Tan LK: Non-mammary metastases to the breast and
axilla: A study of 85 cases. Mod Pathol. 26:343–349. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Karam AK, Stempel M, Barakat RR, Morrow M
and Gemignani ML: Patients with a history of epithelial ovarian
cancer presenting with a breast and/or axillary mass. Gynecol
Oncol. 112:490–495. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Recine MA, Deavers MT, Middleton LP, Silva
EG and Malpica A: Serous carcinoma of the ovary and peritoneum with
metastases to the breast and axillary lymph nodes: A potential
pitfall. Am J Surg Pathol. 28:1646–1651. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Dursun P, Yanik FB, Kuscu E, Gultekin M
and Ayhan A: Bilateral breast metastasis of ovarian carcinoma. Eur
J Gynaecol Oncol. 30:9–12. 2009.PubMed/NCBI
|
|
7.
|
Zhou S, Yu B, Cheng Y, Xu X, Shui R, Bi R,
Lu H, Tu X and Yang W: Metastases to the breast from non-mammary
malignancies: A clinicopathologic study of 28 cases. Zhonghua Bing
Li Xue Za Zhi. 43:231–235. 2014.(In Chinese). PubMed/NCBI
|
|
8.
|
Fulciniti F, Losito S, Botti G, Di Mattia
D, La Mura A, Pisano C and Pignata S: Metastases to the breast:
Role of fine needle cytology samples. Our experience with nine
cases in 2 years. Ann Oncol. 19:682–687. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Amzerin M, Garcia C, Stanciu C, Veys I,
Awada A, Errihani H and Gombos A: Case report: Mammary and rectal
metastases from an ovarian cancer: Report of two cases and review
of literature. F1000Res. 3:2552014.PubMed/NCBI
|
|
10.
|
Wood B, Sterrett G, Frost F and Swarbrick
N: Diagnosis of extramammary malignancy metastatic to the breast by
fine needle biopsy. Pathology. 40:345–351. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Yeh CN, Lin CH and Chen MF: Clinical and
ultrasonographic characteristics of breast metastases from
extramammary malignancies. Am Surg. 70:287–290. 2004.PubMed/NCBI
|
|
12.
|
Susini T, Olivieri S, Molino C,
Castiglione F, Tavella K and Viligiardi R: Ovarian cancer initially
presenting as intramammary metastases and mimicking a primary
breast carcinoma: A case report and literature review. J Womens
Health (Larchmt). 19:169–174. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Williams SA, Ehlers RA II, Hunt KK, Yi M,
Kuerer HM, Singletary SE, Ross MI, Feig BW, Symmans WF and
Meric-Bernstam F: Metastases to the breast from nonbreast solid
neoplasms: Presentation and determinants of survival. Cancer.
110:731–737. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Bernardi S, Bertozzi S, Londero AP,
Gentile G, Angione V and Petri R: Influence of surgical margins on
the outcome of breast cancer patients: A retrospective analysis.
World J Surg. 38:2279–2287. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Cormio G, di Vagno G, Melilli GA, Loverro
G, Cramarossa D and Selvaggi L: Ovarian carcinoma metastatic to the
breast. Gynecol Obstet Invest. 52:73–74. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Goldstein NS, Bassi D and Uzieblo A: WT1
is an integral component of an antibody panel to distinguish
pancreaticobiliary and some ovarian epithelial neoplasms. Am J Clin
Pathol. 116:246–252. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Lee BH, Hecht JL, Pinkus JL and Pinkus GS:
WT1, estrogen receptor and progesterone receptor as markers for
breast or ovarian primary sites in metastatic adenocarcinoma to
body fluids. Am J Clin Pathol. 117:745–750. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Hwang H, Quenneville L, Yaziji H and Gown
AM: Wilms tumor gene product: Sensitive and contextually specific
marker of serous carcinomas of ovarian surface epithelial origin.
Appl Immunohistochem Mol Morphol. 12:122–126. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Tornos C, Soslow R, Chen S, Akram M,
Hummer AJ, Abu-Rustum N, Norton L and Tan LK: Expression of WT1, CA
125 and GCDFP 15 as useful markers in the differential diagnosis of
primary ovarian carcinomas versus metastatic breast cancer to the
ovary. Am J Surg Pathol. 29:1482–1489. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Kaufmann O, Deidesheimer T and Muehlenberg
M: Immunohistochemical differentiation of metastatic breast
carcinomas from metastatic adenocarcinomas of other common primary
sites. Histopathology. 29:233–240. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Wick MR, Lillemoe TJ, Copland GT, Swanson
PE, Manivel JC and Kiang DT: Gross cystic disease fluid protein-15
as a marker for breast cancer: Immunohistochemical analysis of 690
human neoplasms and comparison with alpha-lactalbumin. Hum Pathol.
20:281–287. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Lagendijk JH, Mullink H, van Diest PJ,
Meijer GA and Meijer CJ: Immunohistochemical differentiation
between primary adenocarcinomas of the ovary and ovarian metastases
of colonic and breast origin. Comparison between a statistical and
an intuitive approach. J Clin Pathol. 52:283–290. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Loy TS, Quesenberry JT and Sharp SC:
Distribution of CA 125 in adenocarcinomas. An immunohistochemical
study of 481 cases. Am J Clin Pathol. 98:175–179. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Frierson HF, Moskaluk CA, Powell SM, Zhang
H, Cerilli LA, Stoler MH, Cathro H and Hampton GM: Large scale
molecular and tissue microarray analysis of mesothelin expression
in common human carcinomas. Hum Pathol. 34:605–609. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Ordonez NG: Application of mesothelin
immunostaining in tumor diagnosis. Am J Surg Pathol. 27:1418–1428.
2003. View Article : Google Scholar : PubMed/NCBI
|